PATHOLOGY OF THE SKIN
advertisement

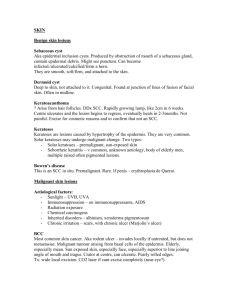
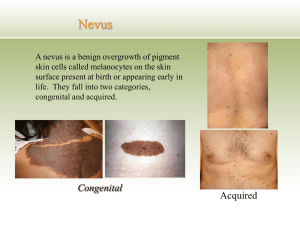
PATHOLOGY OF THE SKIN 1. Disorders of pigmentation and melanocytes Vitiligo -a common disorder characterized by partial or complete loss of pigmentproducing melanocytes in the skin- irregular, well-demarcated plaque devoid of pigmentation -pathogenetically- autoimmune mechanisms- circulating autoantibodies against melanocytes, moreover vitiligo may be associated with other disorders involving autoimmune mechanisms, such as pernicious anemia, Addison disease, autoimmune thyroiditis -histologically-loss of melanocytes Benign pigmented lesions. melanocytic proliferations are composed of one or more of three types of cells: melanocytes epidermal, dermal, nevus cells and melanoma cells -melanocytes are solitary dendritic cells that are generally separated one from another by other cells, such as keratinocytes or fibroblasts- in contrast nevus cells proliferate to form solid nests, melanoma cells- have nuclear abnormalities benign pigmented lesions composed of epidermal melanocytes- include freckles, solar lentigo, melanotic macules in Albright syndrome, and Becker´s melanosis benign pigmented lesions derived from dermal melanocytes include mongolial spot, the nevi of Ota and Ito, and blue nevus benign tumors of nevus cells are called melanocytic nevi- they can be divided into- junctional, compound, intradermal, and there are special variants of melanocytic nevi, such as Spitz nevus, congenital melanocytic nevus, and dysplastic nevus Lesions of epidermal melanocytes: Freckle -a common pigmented lesion of childhood, tan-red to brown, occurring after sun exposure, they are small, flat, sun exposure deepens the pigmentation of freckles (in contrast to lentigo simplex) histologically- normal number of melanocytes but increased melanin within basal keratinocytes Lentigo -common benign hyperpigmented macules in the skin, most often in infancy and childhood, in contrast to freckles they do not darken after sun exposure -histologically-linear basal hyperpigmentation due to melanocyte hyperplasia -the term “lentigo” is derived from the Latin “lenz” meaning lens or lentilthus the term refers to small ovoid or lens-shaped pigmented lesions- then the term has become to be applied to larger pigmented lesions with lentiginous pattern- which includes basal proliferation of melanocytes arranged as single cells rather than nests associated with elongation of rete ridges -two major types of benign lentigo can be distinguished, solar (actinic) lentigo and lentigo simplex (simple lentigo) solar lentigo- occur as multiple lesions in areas exposed to sun, such as face, extensor surfaces of the forearms, and hands, they occur in the fifth decade and later lentigo simplex- is macular hyperpigmentation that arises in childhood, these are few scattered lesions without predilection to sun-exposed skin, they are small symmetrical, few milimeters in diameter melanocytic macules of Albright syndrome- Albright syndrome is characterized by unilateral polyostotic fibrous dysplasia, precocious puberty and melanotic patches- large in size, few in number, located on the same side as bone lesions-hyperpigmentation of basal layer Becker´s melanosis- occurs most commonly as large patch showing hyperpigmantation and hypertrichosis on the shoulder, back or chest of a man, skin lesion is sharply demarcated, histologically- epidermis shows acanthosis, rete ridges are elongated, basal layer is hyperpigmented, number of melanocytes is increased Lesions of dermal melanocytes: Mongolian spot- occurs in sacrococcygeal region as a uniformly blue discoloration, it is present at birth, usually disappears spontaneously within 34 years histology-the dermis shows in its lower part elongated slender dendritic cells containing melanin pigment, these cells are scattered between collagen fibres Nevi of Ota and Ito- are dermal melanocyte hamartomas, characterized by irregular brown-blue discoloration of the skin, there is greater concentration of dermal melanocytes in upper rather than in lower dermis The nevus of Ota- unilateral discoloration of the face composed of blue and brown, confluent lesions- periorbital, forehead, and nose are involved, blue discoloration may affect retina, conjuctiva and cornea, the nevus of Ota may be present at birth The nevus of Ito- supraclavicular, scapular and deltoid region is affected- mottled macular appearance Blue nevus- characterized by presence of pigmented spindle dendritic melanocytes in the reticular dermis associated with alteration in the dermal collagen architecture clinically- small well circumscribed, dome-shaped nodule of blue or blueblack colour, the lesion rarely exceeds 1 cm in diameter, most frequently found on the dorsa of the hands and feet histologically-melanocytes are elongated, lie grouped in irregular bundles in the dermis predominantly with their long axes parallel to the epidermis, most are heavily pigmented with melanin, melanophages are frequently observed near the bundles of melanocytes, the number of fibroblasts is increased within the lesion Benign pigmented lesion composed of nevus cells-melanocytic nevi: Nevocellular nevus -nevus-denotes any congenital skin lesion, nevocellular nevus-refers to a group of congenital or acquired melanocyte lesions having different histologic characteristics, but composed of nevus cells mostly in nesting patterns -clinically- tan-brown papules, five clinical types can be distinguished, flat lesions, slightly elevated, papillomatous, dome-shaped, and pedunculated lesions -the first three types are always pigmented, the latter two may or may not be pigmented -nevi begin as well-defined nests along the dermoepidermal junctionjuntional nevi, with time- extensions of melanocytes form nest within both dermis and epidermis- compound nevi -later epidermal component is lost- intradermal nevi, all these variants are benign junctional nevus- nevus cells lie in well-circumscribed nests within the lower part of epidermis or at the junction with dropping off into the dermis, the nevus cells are regular, cuboidal or spindle shaped, mostly appear in children compound nevus- possesses features of both junctional and intradermal nevi, nevus cell nests are in the epidermis and dermis, and dropping off from the epidermis, the decrease in size observed in nevi is called maturation- is regarded as evidence of benignity intradermal nevus- shows essentially no junctional activity, the upper dermis contains nests and cords of nevus cells, some intradermal nevi contain large fat cells, foreign-body giant cells, foci of ossification, and inflammatory reaction Special types of melanocytic nevi: Spitz nevus- named after Sophie Spitz, who first described it in 1948, also known as juvenile benign melanoma, or spindle and epithelioid cell nevus -lesion occurs mostly in children, is solitary, mostly on the lower extremity and face, it consists of dome-shaped pink nodule, most Spitz nevi are small, less than 6 mm in diameter -histologically- the colour is pink because of a scarcity of melanin, (clinically often looks like hemangioma), nuclei of nevus cells are large slightly polymorphic, nevus cells are spindle-shaped and epithelioid- picture resembles nodular melanoma, the epidermis is often hyperplastic (pseudoepitheliomatous hyperplasia) -in some examples of Spitz nevus- diffuse fibrosis, these are usually composed of spindle cells, called desmoplastic Spitz nevus Pigmented spindle cell nevus- Nevus of Reed- first described as variant of Spitz nevus in 1973, the lesion are usually 3-6 mm in diameter, most patients are young, macro- black flat plaque -heavy pigmentation and sudden appearance- result in clinical diagnosis of melanoma -histologically- pigmented spindle cells of uniform size, heavily pigmented at the dermal-epidermal junction, nests of spindle melanocytes tend to blend with keratinocytes Congenital melanocytic nevus- is a lesion present at birth, found in 1-2% of newborn infants, in many instance congenital nevi are larger than acquired nevi, nevi more than 20 cm in diameter- are called giant congenital nevideeply pigmented and covered by hairs Dysplastic nevus- multiple lesions occurring in patients with some melanomas in family, in relatives, dysplastic nevi may be also solitary without relationship to melanoma -criteria for diagnosis of dysplastic nevus include: melanocytic dysplasia, elongation of rete ridges, lentiginous proliferation of nevus cell in the epidermis, spindle shape of nevus cells, inflammatory infiltrate mild to moderate -significance- patients with dysplastic nevi may develop melanoma, but mostly de novo, and not from pre-existing dysplastic nevus Halo nevus- also known as Sutton nevus, represents a pigmented nevus surrounded by a depigmented zone, halo, -halo nevus is characterized by heavy lymphocytic infiltrate within and below the nevus, most persons are children and young adults, and the back is the most common site Malignant melanoma may be located in situ or may be invasive, invasive melanomas are characterized by two growth patterns: tumorigenic (vertical growth phase) and nontumorigenic (radial growth phase) -melanomas in situ and those with radial growth phase can be divided into: lentigo maligna, superficial spreading, acral lentiginous, and mucosal lentiginous types -invasive melanomas may either arise in association with these in situ types or de novo- nodular melanoma -relatively common malignant neoplasm, currently increasing in incidence -sun exposure seems to be important pathogenetic factor, lightly pigmented persons are in higher risk Classification of melanoma -there are two major categories of melanoma-in the nontumorigenic growth phase- neoplastic melanocytes are confined to epidermis- melanoma in situ or to the epidermis and papillary dermis without formation of a tumor massmicroinvasive melanoma - this is called clinically radial growth phase, and histologically horizontal growth pattern- during this time melanoma does not metastasize -this phase is followed by vertical growth phase - characterized by dermal invasion with tumor formation- means development of capacity to metastasize Nontumorigenic melanoma- radial growth phase include Superficial spreading melanoma- is the most frequent form of melanoma (about 70% of all cases) most frequent sites are upper back, and lower legs the lesions are slightly elevated, with palpable borders, and irregular outlines, often variation in colour, that include tan, brown, blue, gray and pink, the diameter is less than 6 mm histologically- the lesion is assymetric, the epidermis is thickened, large melanocytes are scattered in pagetoid pattern within epidermis, the melanoma cells lie in nest in lower epidermis Lentigo maligna melanoma- morbus Dubreuilh-accounts for about 10% of all cases of melanoma, typically occurs in chronically sun exposed surfaces of the elderly- face, back (men), lower legs (women), forearms, the lesion grows slowly over years, starting as unevenly pigmented macule and gradually extends the size to several centimeters in diameter, the colour varies from brown, to black, in contrast to SSM, LMM is not accurately deliniated histologically- in early stage lentigo maligna shows hyperpigmentation in periphery with melanocytic proliferation, the epidermis is flattened, some nesting of melanocytes is observed in junction, the other melanocytes retain dendritic processes Acral lentiginous melanoma- occurs on the hairless skin of palms and soles, and in the ungual regions, clinically- shows uneven pigmentation with irregular indefinite borders histologically-majority of melanocytes are single in lentiginous pattern located at the junction Tumorigenic melanoma- vertical growth phase -any of nontumorigenic types of melanomas may develop vertical growth phase Nodular melanoma- in contrast to other types, contains only vertical growth, occurs in slightly older patients than the common superficial spreading melanoma, and is relatively more frequent in men -nodular melanoma- is elevated variably pigmented papule that increases its size rapidly, histologically- there is continuous growth of uniformly atypical melanocytes in dermis, upward pagetoid growth of tumor cells into the epidermis is typical feature, the tumor cells show great variation in size and shape, often they are epithelioid and spindle shaped Variants of melanoma include desmoplastic and neurotropic melanoma Desmoplastic melanoma- melanoma cells are elongated and usually amelanotic and are embedded in markedly fibrotic stroma Neurotropic melanoma- is composed of fascicles of spindle shaped melanomas cells often with desmoplasia, that invade the nerves Prognosis and management of melanomas -tumor thickness (described by Breslow) and level of invasion (according to Clark) are considered to be most important prognostic factors -level I- (100% 10-year disease-free survival)- melanoma cells confined to the epidermis-melanoma in situ -level II (96% survival) - there is extension to the papillary dermismicroinvasive melanoma -level III (86%)- there is extension of tumor cells throughout the papillary dermis -level IV (66%)- are invasive and tumorigenic, invade reticular dermis -level V (53%)- invade subcutaneous fat -other prognostic factors, such as mitotic rate, ulceration, histological type, biological markers are of limited value treatment: local excision is recommended, with safe margins at least 5 mm beyond the perimeter of the lesion, clinically positive lymph nodes should be biopsied BENIGN EPITHELIAL TUMORS. Seborrheic keratosis -most often in middle-aged and older persons -uniform tan-brown round granular plaques, histologically exophytic lesions with hyperplasia of variably pigmented basaloid cells and hyperkeratosis. Keratoacanthoma -common lesion presenting as rapidly growing tumor, typically located in sun-exposed skin, this is a self-limited lesion that may heal spontaneously -macroscopically- flesh-colored, superficial lesion several centimeters in diameter, located on face and hands histologically- cup-shaped epithelial proliferation enclosing the central keratin-filled plug, the pattern of keratinization is similar to that one of hair follicles- no granular cell layer -minimal inflammation is present within the dermis Premalignant and malignant epidermal tumors. Actinic keratosis- a premalignant dysplastic lesion associated with chronic sun exposure, macroscopically- usually less than 1 cm in diameter, tan-brown or red with rough consistency histologically-there is cytologic atypia in the lower epidermis, frequently with basal cell hyperplasia and hyperkeratosis, dyskeratosis and parakeratosis may be present, basal membrane is intact, upper dermis contains inflammatory infiltrate, local excision is recommended- may undergo malignant transformation Squamous cell carcinoma-the most common tumor of sun-exposed skin of older individuals, sunlight (especially ultraviolet irradiation) is well known predisposing factor- it causes direct DNA damage in keratinocytes -in situ squamous cell carcinoma- Bowen disease- appears as welldemarcated red scaling plaque, histologically - full thickness severe dysplastic changes within the epidermis, basement membrane is intact -invasive lesions- tend to be ulcerated, histologically invasive tumors vary from well differentiated with prominent keratinization to highly anaplastic tumors with abortive keratinization Basal cell carcinoma- is common slowly growing tumor in sun-exposed skin, it grows in locally aggressive manner but does not metastasize, grossly- it appears as pearly papules or plaques and advanced lesions become ulcerated, some are melanin pigmented, histologically- basal cell proliferation extending to the dermis Merkel cell carcinoma- a rare malignant neoplasm derived of neuroendocrine Merkel cells, the tumor is composed of small round basophilic malignant cells (the cells contain neurosecretory granules) and resemble small cell carcinoma of the lung ADNEXAL TUMORS. -most are single or multiple nondescript nodules, most are benign cylindroma- typically occurs as multiple coalescing nodules on the forehead and scalp, they may be inherited and appear early in life histologically- they display apocrine differentiation with islands of basaloid cells within the hyalinized matrix syringoma-usually occur as multiple small, tan papules near the lower eyelids, microscopically- it is composed of tadpole-shaped islands of basaloid epithelium with focal eccrine differentiation trichoepithelioma- may be inherited, usually present as multiple semitransparent papules on the face, scalp and neck, histologically -composed of proliferations of basaloid cells forming follicle-like structures trichilemmoma- composed of the cells resembling hair follicle infundibulum TUMORS OF DERMIS. Benign fibrous histiocytoma- a heterogenous group of benign neoplasms composed of dermal fibroblasts and histiocytes, usually in adults, frequently on legs of young to middle-aged women grossly- tan-brown firm papules, sometimes tender, histologically-the most common form is composed of spindle-shaped fibroblasts and histiocytes (sometimes foamy cells, deposits of hemosiderin) Dematofibrosarcoma protuberans- well-differentiated slow-growing tumor of the skin that is locally aggressive but does not metastasize grossly- firm solid nodules, plaques, sometime ulcerated- often on the trunk, histologically- cellular neoplasms composed of radially oriented fibroblasts in storiform pattern clinical behavior is that of low grade sarcoma Xanthoma- not true neoplasm, but rather focal accumulations of foamy histiocytes, may be idiopathic, or associated with familiar hyperlipidemia Xanthelesma- soft yellow plaques on the eyelids in patients with or without lipid metabolism abnormalities Eruptive xanthoma- sudden occurrence of yellow papules that appear and disappear with changing plasma lipid levels- located in buttocks, posterior thighs, knees, etc. Tuberous xanthoma- yellow, flat nodules over the joints, especially knees and elbows Tendinous xanthoma- yellow nodules over the Achilles tendon and finger extensor tendons All these xanthomas are characterized by variably cellular dermal aggregates of macrophages with foamy cytoplasm containing cholesterol and triglycerids OTHER TYPES OF SKIN TUMORS AND PROLIFERATIONS Histiocytosis X- the systemic patterns have been discussed, cutaneous form presents as solitary or multiple papules or nodules in the skin histologically- composed of Langerhans cells- mononuclear cells with bland indented nuclei with variable admixture of eosinophilic leukocytes Mycosis fungoides (cutaneous T-cell lymphoma)- is a lymphoproliferative disorder characterized by neoplastic cell infiltrates in the skin, if associated with generalized T-cell leukemia- Sézary syndrome grossly- MF presents as eczema-like lesions- scaly, red-brown patches or plaques, and nodules- usually on the trunk, extremities face and scalp histologically-presence of Sézary cell- neoplastic T lymphoid cells Mastocytosis- rare disorder characterized by cutaneous mast cell proliferation, symptoms reflect histamine and heparin release, clinical symptoms include pruritus, flushing, triggered by specific foods, temperature, alcohol or certain drugs urticaria pigmentosa- is exclusively cutaneous form, occurs mostly in children grossly- skin lesions are multiple, round-to-oval, red-brown papules, microscopically composed of eosinophils, mast cells with fibrosis and edema NON-TUMOROUS DISORDERS OF THE SKIN -chronic inflammatory dermatoses -acute inflammatory disorders -blisters -infections of the skin –dermatoses of ticks Chronic inflammatory dermatoses: are persistent inflammatory disorders, lasting over several months to years Psoriasis- a common inflammatory cutaneuous disorder, etiology unknown, genetic predisposition is likely, but a genesis of new lesions at the sites of trauma suggests a possible role for exogenous stimuli, damage to the stratum corneum may induce the deposition of complement-fixing antibodies with secondary complement-mediated immune injury, psoriasis may be associated with other diseases, such as enteropathies, myopathies, rheumatoid arthritis, etc grossly- lesions are well-demarcated, salmon pink, plaques with silvery scaling- elbows, knees, scalp, lumbosacral area, histologically- marked acanthosis with rete elongations, stratum granulosum is absent, with extensive overlying parakeratosis, epidermis overlying dermal papillae is thinned, aggregates of neutrophils in epidermis occur within stratum spinosusm- Munro microabscesses Lichen planus- a self-limited disease, pathogenesis is unknown, cell-mediated immune injury is likely grossly- pruritic, purple papules, that may coalesce to plaques, they are multiple, symmetrically distributed, often on the writs and elbows, oral mucosa may be affected histologically- there is a dense, band-like dermoepidermal junction lymphocytic infiltrate with basal cell degeneration- basal cell die by apoptosisto form colloid or Civatte bodies Lupus erythematodes- two major variants -systemic LE, and discoid LElocalized cutaneous form of LE without systemic manifestation pathogenesis is unknown, immune complex mediated or cell-mediated immune injury is suspected grossly- skin lesions of both SLE and DLE include ill-defined erythematous scaling plaques with zones of irregular pigmentation histologically- DLE is characterized by dermoepidermal junction, perivascular and periapendical lymphocytic infiltrates, subcutaneus tissue may be also infiltrated acne vulgaris- a common chronic inflammatory dermatosis affecting hair follicles, typically in the middle to late adolescence, more severe in men than in girls, pathogenesis is speculative, heritable component is included, the lesions are however triggered by sex hormone stimulation, and bacterial infection also seems to participate (Propionibacterium acnes)- this bacterium causes lipase degradation of sebaceous oils, thus highly irritative fatty acids appear, antibiotics may be effective by inhibiting the lipase activity, the vitamine A derivates are also partly effective in therapy grossly-acne is characterized by open comedones (follicular papules with central plug trapped beneath the epidermis and therefore not visible), inflammatory acne shows erythematous papules nodules and pustules histologically- comedones are composed of lipid and keratin deposits within the midportion of hair follicles with follicle dilatation and epithelial and sebaceous gland atrophy -there is variable lymphohistiocytic infiltrate, and the chronic extensive inflammation may cause scar formation acute inflammatory disorders -are characterized by short-lived lesions (days to weeks) marked by lymphocytic infiltrate with edema and local tissue damage Urticaria (hives)- a common disorder characterized by focal mast cell degranulation, with histamine-mediated dermal pruritus, edema, and wheal, it occurs in young adults, histologically-sparse lymphocytic perivascular infiltrate with edema, most lesion are mediated by antigen-specific IgE, that results in degranulation of mast cells in sensitive patients Acute eczematous dermatitis- a group of pathogenetically different conditions with similar histological features, five major types of eczema exist, contact dermatitis (caused by local contact with irritative chemicals), atopic dermatatis (heritable immune-mediated dermatitis), drug-related eczematous dermatitis (caused by systemic administration of certain drug, such as penicilin), photoeczematous eruptions (caused by UV light in sensitive persons), and primary irritant dermatitis (repeated trauma) grossly- all types of acute eczema are pruritic, red, papulovesicular lesions with blistering, in chronic lesions- scaling plaques microscopically-spongiosis with progressive fluid accumulationintraepidermal vesicles, dermal perivascular lymphocytic infiltrate blisters: -these are primary blistering disorders, the level of blister formation is critical for diagnosis (subcorneal, suprabasal, subepidermal, intraepidermal) pemphigus- rare autoimmune disorder, typically occurs in 4.-6.decades, characterized by circulating antibodies to keratinocytes, it involves oral mucosa, face, scalp, trunk, etc, if untreated it is fatal grossly-superficial easily ruptured blisters, that leave shallow crusted erosions micro-acantholyis leading to intercellular clefting- and intraepidermal blisters dermatitis herpetiformis- a rare disorder typically in the 3.-4.decades, in males more common, associated with specific HLA types, DH is presumably mediated either by immune complex deposition in the skin, or by antibodies to gliadin (protein of gluten-DH may be associated with celiac disease and may respond to gluten-free diet)- that cross-reacts with junctional anchoring components in the basement membrane of the skin -presence of granular IgA deposits in the dermal papillae tips is characteristic histologically- neutrophils and fibrin accumulates in the tips of dermal papillae-subepidermal blisters porphyria-is non-inflammatory blistering disorder, is a group of inborn or acquired disturbances of porphyrin metabolism, the cutaneous lesions consists of urticaria and vesicles that are triggered by sun exposure and heal without scarring, histologically- subepidermal vesicles and blisters skin infections Warts (Verruca)- common spontaneously regressing lesions, typically in children and adolescents, caused by HPV transmitted by direct contact types 6, 11, 16, and 18 are associated with anogenital warts, type 16 and 34 may cause dysplasia. verruca vulgaris (common wart)-most common, most frequently on the hand, grey to white flat to convex papule with rough surface verruca plana (flat wart)- on the face or dorsum of the hand, uterine cervix, flat tan-coloured papule with smooth surface verruca plantaris (soles) and palmaris (palms)- rough scaly lesions condyloma accuminatum (anogenital and venereal warts)- soft tan masses up to several centimeters in diameter histologically- all warts are characterized by epidermal hyperplasia and superficial keratinocyte perinuclear vacuolization (koilocytosis)- elmi-reveals numerous viral particles within koilocytes molluscum contagiosum- common, self-limited disease caused by poxvirus transmitted by direct contact grossly- pruritic pink papule seen on the trunk, or anogenital region micro-verrucous cuplike epidermal hyperplasia with molluscum bodies-large eosinophilic cytoplasmic inclusions in the stratum granulosum-represent virions impetigo- streptococcal or staphylococcal skin infection seen in normal children especially on the face and hands (rarely may affect sick adults), it begins as an erythematous macule that progresses to small pustules and erosions-with honey-coloured crust histologically- subcorneal pustules filled with neutrophils dermatoses from ticks -ticks are ectoparasites that cause dermatologic disease directly by their bites and indirectly as vectors of bacterial, viral, protozoal and ricketssial diseases tick bites cause a variety of acute and chronic skin lesions -tick-borne diseases include Lyme disease, tick-borne relapsing fever, tularaemia, Rocky Mountains spotted fever, and others Lyme disease is the most common vector-born skin disease- over the last decade, knowledge about pathobiology, molecular immunology and clinical course of Lyme disease has expanded rapidly -Lyme disease is caused by borrelia (Burgdorferi in the U.S., and B. afzelii and B. garinii in Europe and Asia), microorganism transmission is unlikely when ticks are removed within 24 h. of attachment -Lyme d. occurs in stages with different clinical manifestation in each stage stage 1- localized infection, erythema migrans is seen in most patients, headache, fatigue, malaise, arthralgias, in few lymphadenopathy stage 2- disseminated infection-within days to weeks after inoculationmultisystem involvement- migratory pains in joints, tendons, muscles, bones, neurological problems include meningitis, motor and sensory palyradiculopathy stage 3- late and persistent infection- acrodermatitis chronica atrophicans, fibrotic nodules, sclerotic and atropohic skin lesions, such as lichen sclerosus et atrophicus