Table 1
advertisement
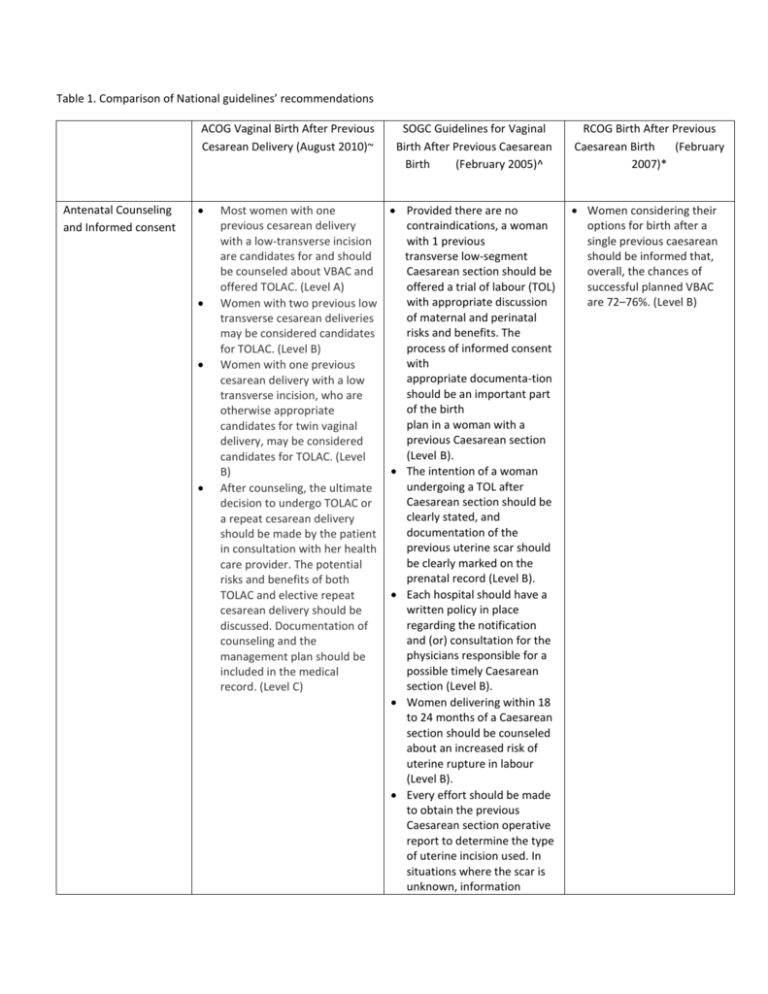
Table 1. Comparison of National guidelines’ recommendations ACOG Vaginal Birth After Previous Cesarean Delivery (August 2010)~ Antenatal Counseling and Informed consent Most women with one previous cesarean delivery with a low-transverse incision are candidates for and should be counseled about VBAC and offered TOLAC. (Level A) Women with two previous low transverse cesarean deliveries may be considered candidates for TOLAC. (Level B) Women with one previous cesarean delivery with a low transverse incision, who are otherwise appropriate candidates for twin vaginal delivery, may be considered candidates for TOLAC. (Level B) After counseling, the ultimate decision to undergo TOLAC or a repeat cesarean delivery should be made by the patient in consultation with her health care provider. The potential risks and benefits of both TOLAC and elective repeat cesarean delivery should be discussed. Documentation of counseling and the management plan should be included in the medical record. (Level C) SOGC Guidelines for Vaginal Birth After Previous Caesarean Birth (February 2005)^ Provided there are no contraindications, a woman with 1 previous transverse low-segment Caesarean section should be offered a trial of labour (TOL) with appropriate discussion of maternal and perinatal risks and benefits. The process of informed consent with appropriate documenta-tion should be an important part of the birth plan in a woman with a previous Caesarean section (Level B). The intention of a woman undergoing a TOL after Caesarean section should be clearly stated, and documentation of the previous uterine scar should be clearly marked on the prenatal record (Level B). Each hospital should have a written policy in place regarding the notification and (or) consultation for the physicians responsible for a possible timely Caesarean section (Level B). Women delivering within 18 to 24 months of a Caesarean section should be counseled about an increased risk of uterine rupture in labour (Level B). Every effort should be made to obtain the previous Caesarean section operative report to determine the type of uterine incision used. In situations where the scar is unknown, information RCOG Birth After Previous Caesarean Birth (February 2007)* Women considering their options for birth after a single previous caesarean should be informed that, overall, the chances of successful planned VBAC are 72–76%. (Level B) Delivery resources and facilities Risks and benefits A trial of labor after previous cesarean delivery should be undertaken at facilities capable of emergency deliveries. Because of the risks associated with TOLAC and that uterine rupture and other complications may be unpredictable, the College recommends that TOLAC be undertaken in facilities with staff immediately available to provide emergency care. When resources for immediate cesarean delivery are not available, the College recommends that health care providers and patients considering TOLAC discuss the hospital's resources and availability of obstetric, pediatric, anesthetic, and operating room staffs. Respect for patient autonomy supports that patients should be allowed to accept increased levels of risk, however, patients should be clearly informed of such potential increase in risk and management alternatives. (Level C) None as a recommendation concerning the circumstances of the previous delivery is helpful in determining the likelihood of a low transverse incision. If the likelihood of a lower transverse incision is high, a TOL after Caesarean section can be offered (Level B). For a safe labour after Caesarean section, a woman should deliver in a hospital where a timely Caesarean section is available. The woman and her health care provider must be aware of the hospital resources and the availability of obstetric, anesthetic, pediatric, and operating-room staff.(Level A) Suspected uterine rupture requires urgent attention and expedited laparotomy to attempt to decrease maternal and perinatal morbidity and mortality (Level A). In the case of a TOL after Caesarean, an approximate time frame of 30 minutes should be Women should be advised that planned VBAC should be conducted in a suitably staffed and equipped delivery suite, with continuous intrapartum care and monitoring and available resources for immediate caesarean section and advanced neonatal resuscitation. (Level B) Women considering the options for birth after a previous caesarean should be informed that planned VBAC carries a risk of uterine rupture of 22– 74/10,000. There is virtually no risk of uterine rupture in women undergoing ERCS. (Level B) Women considering the considered adequate in the set-up of an urgent laparotomy (Level C). options for birth after a previous caesarean should be informed that planned VBAC compared with ERCS carries around 1% additional risk of either blood transfusion or endometritis.(Level B) Women considering planned VBAC should be informed that this decision carries a 2–3/10,000 additional risk of birthrelated perinatal death when compared with ERCS. The absolute risk of such birth-related perinatal loss is comparable to the risk for women having their first birth. (Level B) Women considering the options for birth after a previous caesarean should be informed that planned VBAC carries an 8/10,000 risk of the infant developing hypoxic ischaemic encephalopathy. The effect on the longterm outcome of the infant upon experiencing HIE is unknown. (Level B) Women considering the options for birth after a previous caesarean should be informed that attempting VBAC probably reduces the risk that their baby will have respiratory problems after birth: rates are 2–3% with planned VBAC and 3–4% with ERCS. (Level B) Women considering the options for birth after a previous caesarean should be informed that the risk of anaesthetic complications is extremely low, irrespective of whether they opt for planned VBAC or ERCS. Fetal Heart Rate monitoring None as a recommendation Continuous electronic fetal monitoring of women attempting a TOL after Caesarean section is recommended (Level A). Induction and augmentation of labor Medical induction of labour with oxytocin may be associated with an increased risk of uterine rupture and should be used carefully after appropriate counseling (Level B). Medical induction of labour with prostaglandin E2 (dinoprostone) is associated with an increased risk of uterine rupture and should not be used except in rare circumstances and after appropriate counseling (Level B). Medical induction of labour with oxytocin may be associated with an increased risk of uterine rupture and should be used carefully after appropriate counseling (Level B). Oxytocin augmentation is not contraindicated in women undergoing a TOL after Caesarean section (Level A). Prostaglandin E1 (misoprostol) is associated with a high risk of uterine rupture and should not be used as part of a TOL after Caesarean section (Level A). A foley catheter may be safely used to ripen the Induction of labor for maternal or fetal indications remains an option in women undergoing TOLAC. (Level B) Misoprostol should not be used for third trimester cervical ripening or labor induction in patients who have had a cesarean delivery or major uterine surgery. (Level A) (Level B) Women considering the options for birth after a previous caesarean should be informed that ERCS may increase the risk of serious complications in future pregnancies. (Level B) Women should be advised to have continuous electronic fetal monitoring following the onset of uterine contractions for the duration of planned VBAC. (Level B) Women should be informed of the two- to three-fold increased risk of uterine rupture and around 1.5-fold increased risk of caesarean section in induced and/or augmented labours compared with spontaneous labours. (Level B) Success Rate Contraindications and special circumstances None as a recommendation External cephalic version for breech presentation is not contraindicated in women with a prior low transverse uterine incision who are at low risk for adverse maternal or neonatal outcomes from external cephalic version and TOLAC. (Level B) Those at high risk for complications (eg, those with previous classical or T-incision, prior uterine rupture, or extensive transfundal uterine surgery) and those in whom vaginal delivery is otherwise contraindicated (eg, those with placenta previa) are not generally candidates for planned TOLAC. (Level B) TOLAC is not contraindicated for women with previous cesarean delivery with an unknown uterine scar type unless there is a high clinical suspicion of a previous classical uterine incision. (Level B) cervix in a woman planning a TOL after Caesarean section (Level A). The available data suggest that None as a a trial of labour in women recommendation with more than 1 previous Caesarean section is likely to be successful but is associated with a higher risk of uterine rupture (Level B). Multiple gestation is not a Women with a previous contraindication to TOL uterine incision other than after Caesarean section an uncomplicated low (Level B). transverse caesarean section incision who wish Diabetes mellitus is not a to consider vaginal birth contraindication to TOL should be assessed by a after Caesarean section consultant with full access (Level B). to the details of the Suspected fetal macrosomia previous surgery. (Level C) is not a contraindication to TOL after Caesarean section Women with a prior history of two (Level B). uncomplicated low Postdatism is not a transverse caesarean contraindication to a TOL sections, in an otherwise after Caesarean section uncomplicated pregnancy (Level B). at term, with no contraindication for vaginal birth, who have been fully informed by a consultant obstetrician, may be considered suitable for planned VBAC. (Level B) Women who are preterm and considering the options for birth after a previous caesarean should be informed that planned preterm VBAC has similar success rates to planned term VBAC but with a lower risk of uterine rupture. (Level B) A cautious approach is advised when considering planned VBAC in women with twin gestation, fetal macrosomia and short interdelivery interval, as there is uncertainty in the safety and efficacy of planned VBAC in such Anesthesia Epidural analgesia for labor may be used as part of TOLAC. (Level A) situations. (Level C) The routine use of intrauterine pressure catheters in the early detection of uterine scar rupture is not recommended. (Level C) Epidural anaesthesia is not contraindicated in planned VBAC. (Level C) SOGC, Society of Obstetricians and Gynaecologists of Canada; RCOG, Royal College of Obstetricians and Gynaecologists The grade of recommendation is in parenthesis. ~ American College of Obstetricians and Gynecologist; Vaginal Birth After Previous Cesarean Delivery. Practice Bulletin No. 115, 2010 (reference #). ^ Society of Obstetricians and Gynaecologists of Canada; Guidelines for Vaginal Birth After Previous Caesarean Birth Clinical Practice guideline, No. 155, 2005 (reference #). * Royal College of Obstetricians and Gynaecologists: Birth After Previous Caesarean Birth: Green-top Guideline No. 45, February 2007 (reference #).