Menorrhagia: a clinical update Carl E Wood
advertisement

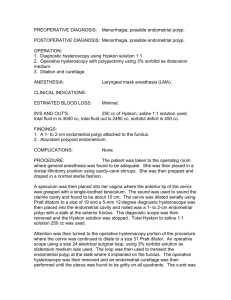
Menorrhagia: a clinical update Carl E Wood Almost every woman experiences episodes of abnormal or excessive menstrual bleeding MJA 1996; 165: 510-514 Readers may print a single copy for personal use. No further reproduction or distribution of the articles in whole or in part should proceed without the permission of the publisher. For copyright permission, contact the Australasian Medical Publishing Company Journalists are welcome to write news stories based on what they read here, but should acknowledge their source as "an article published on the Internet by The Medical Journal of Australia <http://www.mja.com.au/>". Introduction - Assessment of blood loss - Causes - Diagnosis - Management - Drug therapy - Surgery - References - Authors' details Make a comment - Register to be notified of new articles by e-mail - Current contents list - ©MJA1996 Introduction Menorrhagia is defined as a blood loss of 80 mL or more per period. Population studies show that the typical menstrual blood loss is 30-40 mL, and that 90% of women have losses of less than 80 mL. 1 Menorrhagia is still one of the more common reasons for women to be referred to a gynaecologist, and is the main presenting symptom in 38% of Australian women having hysterectomies. 2 Box 1 summarises the stages in clinical assessment and management of menorrhagia. 1: Assessment and management of menorrhagia Assessment of blood loss Women seeking treatment for menorrhagia often do not have greater blood losses than average. In a population study, 26% of women with normal menstrual loss ( < 60 mL) considered their periods heavy, while 40% of those with heavy losses ( > > 80 mL) considered their periods to be moderate or light. 1 In one study, over half the women referred for endometrial ablation complaining of heavy periods had menstrual blood losses of less than 80 mL. 3 Social embarrassment, inconven ience, costs of sanitary protection, the safety of using tampons, and interference with sexual activity all make coping with menstruation difficult. An approximate assessment of blood loss can be made from a pad and tampon count. 4 If blood loss does not appear excessive, then counselling on how best to manage menstrual loss may avoid unnecessary drug treatment or surgical intervention. Causes The volume of blood lost at menstruation is controlled by local uterine vascular tone, haemostasis, and regeneration of endometrium. Studies of patients with menorrhagia have shown a greater endometrial concentration of the vasodilator prostaglandin E (PGE), 5,6 and a relationship between total prostaglandin (PGE, PGI 2 and PGF 2 a ) concentration and average blood loss. 6 Increased endometrial fibrinolysis may be of importance, 7 as suggested by reduction in mean menstrual blood loss in women taking fibrinolytic inhibitors (e.g., tranexamic acid). 8 The wide variety of causes of menorrhagia are shown in Box 2. The frequency of the organic causes in a normal population is not known. Anovulation may be associated with menorrhagia close to menarche and to menopause. It may be particularly important when prolonged menstrual cycles occur, as oestrogen in the absence of progesterone may cause endometrial hyperplasia, atypical hyperplasia and eventually carcinoma. Progesterone alone or progesterone associated with the oral contraceptive pill prevents such changes. Management of women with menorrhagia may be more effective if psychosocial factors (depression, work difficulties, heavy smoking [> 20 per day], excessive alcohol intake, and sexual problems) 9,10 are taken into consideration. Diagnosis The main diagnostic procedures for menorrhagia include: Dilatation and curettage Outpatient endometrial sampling Hysteroscopy Vaginal ultrasonography. Dilatation and curettage (D&C) involves a general anaesthetic and a one-day stay in hospital; it is not cost effective for diagnosing endometrial malignancy in women under 40 years (who have a low prevalence of serious uterine conditions and endometrial cancer). 11 The potential benefits need to be weighed up against the risks (general anaesthesia and possible uterine perforation and laceration of the cervix). 12 Moreover, a significant proportion of endometrial lesions are not detected by D&C, 12,13 and its usefulness as a diagnostic tool has been repeatedly questioned. 12,14,15 Endometrial sampling and hysteroscopy: Endometrial sampling (the passage of intrauterine catheters which scrape or brush the endometrial surface) or hysteroscopy (which enables targeted biopsy of abnormal endometrium) have high levels of patient acceptability, lower complication rates, usually do not require inpatient admission and general anaesthesia, and are as accurate and cost effective as D&C. 15-17 Vaginal ultrasound: Ultrasound diagnosis markedly increases the accuracy of clinical diagnosis and assists in treatment choice (including avoidance of surgery) and selection of patients most suited to endometrial resection, intrauterine resection of polyps and fibromyomas, open, vaginal or laparoscopic myomectomy, adenomyomectomy and hysterectomy. 18 Management Drug therapy Over the last decade, a wide variety of drugs have been used for the treatment of menorrhagia (Box 3). Medical treatment avoids major surgery, but has associated side effects and is generally only effective for the duration of treatment. Thirty-one randomised controlled trials of drug therapy with objective measurement of menstrual blood loss have been published. The one controlled study, comparing tranexamic acid (1 g given four times daily on Days 1-4 of menstruation) and norethisterone taken on Days 9-26, showed tranexamic acid to be more effective and with no significant side effects. Although isolated case reports of thrombotic episodes with tranexamic acid exist, a Scandinavian study of 238 000 treatments with this drug over 19 years showed no increased thrombotic events compared with those in an agematched general population. 22 The possibility of minor subclinical thrombosis with long term use can be excluded only by a follow-up study. In women with a pretreatment blood loss of 80-200 mL per cycle, 92% had their blood loss reduced to less than 80 mL per cycle with tranexamic acid. Those with a menstrual blood loss of more than 250 mL per cycle did not achieve a normal blood loss and required surgery. 23 A comparison of the drugs used in all the controlled trials indicates that a norgestrelreleasing intrauterine device (IUD), 28,30 danazol, 20,28 and tranexamic acid 24,30 are most effective in reducing menstrual blood loss, while mefenamic acid, 20,28 the oral contraceptive pill and progestogens are usually less effective. A recent study has shown tranexamic acid to be more effective (54% reduction in blood loss) than mefenamic acid (20% reduction), whereas ethamsylate (a clotting agent) was ineffective. 31 (The hormone-releasing IUD is not registered for use in Australia or the United Kingdom as treatment for menorrhagia.) Danazol's serious side effects (menopausal symptoms and mild androgenic effects) make it unacceptable for long term use and it is also relatively expensive.Tranexamic acid has few side effects and offers the advantage of alleviating menstrual pain. Surgery Abdominal hysterectomy v. endometrial resection Randomised controlled trials have been performed comparing abdominal hysterectomy with less invasive surgical intervention for menorrhagia. 32,33 Abdominal hysterectomy requires longer theatre times and six or seven days' hospital stay, whereas endometrial resection (ablation) is a day-stay or overnight procedure. Abdominal hysterectomy has a higher complication rate (45%) compared with transcervical endometrial resection (0-15%). Complications include uterine perforation, fluid overload, haemorrhage and cervical stenosis. Reported mortality rates for abdominal hysterectomy are two to five times higher than those for endometrial resection (0.06%-0.16% v. 0.03%), and major complication rates are five to twelve times higher (1%-2.5% v. 0.2%). 34 Resumption of normal activities after abdominal hysterectomy takes two to three months versus two to three weeks for resection. Endometrial resection results in 13%-64% of women having no menstrual bleeding and 62%-77% having reduced menstrual loss. After endometrial resection 6%-23% of women require reoperation for continued bleeding, with the higher rates being reported in studies with a longer follow-up. 32,33 The probability of requiring a hysterectomy four years after endometrial resection has been estimated to be 12%. 35 Some form of sterilisation or contraception is needed after endometrial resection. Pregnancy is unlikely, but if it occurs the risk of complications is higher. Hysterectomy is preferable if the patient has a large uterus, severe endometriosis, a desire for amenorrhoea or certain cure, or there is an increased risk of uterine cancer (family history, marked obesity, polycystic ovaries and diabetes). Endometrial resection can be used if a woman is unfit for hysterectomy. It also avoids possible ovarian dysfunction and the psychological effects of hysterectomy. Endometrial resection has a 47% cost advantage over hysterectomy because of shorter theatre time and hospital stay, but the cost advantage diminishes with time to 29% because of the need for repeat surgery. 36 Myomectomy The number of abdominal myomectomies performed in Australia has been estimated at 1500 per year; most are for menorrhagia in women wishing to retain the uterus. 2 After myomectomy, recurrence rates of 5%-27%, retreatment rates of 10%, and fertility rates of 40%-59% have been reported. 37 Some abdominal myomectomies may be replaced by laparoscopic or laparoscopicminilaparotomy procedures, as fibroids up to 14 cm in diameter in uteri up to the size of a uterus in a 24 weeks' pregnant woman have been removed by these methods. 29,38 The safety of the laparoscopic technique has been established, with the only serious complication among 214 patients in three studies being one postoperative haemorrhage requiring reoperation. 29,38,39 Abdominal v. laparoscopic myomectomy The average hospital stay for abdominal myomectomy is four to five days, compared with one to three days for the laparoscopic procedure. 29,40 The cost of laparoscopic myomectomy ($2217) is lower than that of abdominal myomectomy ($3825). 2 Laparoscopic myomectomy involves a shorter hospital stay, with probable associated advantages of reduced pain, reduced risk of wound complications, earlier return to normal activity, and reduced costs. 40 Myoma reduction has been performed by laser or electro coagulation. A volume reduction varying from 10% to 80% has been achieved with fibromyoma up to 10 cm in diameter. Follow-up so far has been limited to three years and there has been little or no regrowth. 37,41 Results of further studies may establish its role in the treatment of menorrhagia. Hysterectomy Compared with abdominal hysterectomy, vaginal hysterectomy is associated with less pain and morbidity, shorter hospital stays and faster recovery periods. 42 However, analysis of Australian hospital morbidity data indicates that at least some of these benefits do not always accrue. 2 It is more difficult to perform and its use to date for menorrhagia and, in particular, myomas is limited. Only 25% of hysterectomies are performed vaginally in Australia. 2 Techniques for laparoscopic hysterectomy are still developing. 43,44 Results indicate that, compared with abdominal hysterectomy, postoperative pain is reduced and hospital stays (one to four days) and recovery periods (one to four weeks) are shorter. A meta-analysis of 29 reports involving 3189 patients having laparoscopic hysterectomy 45 showed lower febrile morbidity and incidence of blood transfusion, but similar serious complication rates, to both vaginal and abdominal hysterectomies. Seven controlled trials comparing laparoscopic with abdominal procedures showed reduced time in hospital, shorter convalescence and similar complication rates. 45,46 Like vaginal hysterectomy, laparoscopic hysterectomy, with its reduced recovery period, does benefit patients, their families and employers. In conclusion, the diversity of possible surgical treatments indicates the need for flexibility in choosing techniques to resolve an individual patient's problem, and the possible advantage for gynaecologists to learn the new hysteroscopic and laparoscopic techniques for removal of the endometrium, polyps, myomas, adenomyomas and the uterus (Box 4). References 1. Hallberg L, Hogdahl AM, Nilsson L, Rybo G. Menstrual blood loss -- a population study. Acta Obstet Gynecol Scand 1966; 45: 320-351. 2. Hirsch NA. Technologies for the treatment of menorrhagia and uterine myomas. Canberra: Australian Institute of Health and Welfare, 1993. (Health Technology Series No. 10.) 3. Deeny M, Davis JA. Assessment of menstrual blood loss in women referred for endometrial ablation. Eur J Obstet Gynaecol 1994; 57: 179-180. 4. Higham JM, O'Brien PMS, Shaw RW. Assessment of menstrual loss using a pictorial chart. Br J Obstet Gynaecol 1990; 97: 734-739. 5. Smith SK, Abel MH, Kelly RW, Baird DT. Prostaglandin synthesis in the endometrium of women with ovular dysfunctional uterine bleeding. Br J Obstet Gynaecol 1981; 88: 434-442. 6. Cameron IT, Leask R, Kelly RW, Baird DT. Endometrial prostaglandins in women with abnormal menstrual bleeding. Prostaglandins Leukot Med 1987; 29: 249-258. 7. Albrechtson OK. The fibrinolytic activity of the human endometrium. Acta Endocrinol 1956; 23: 219-229. 8. Ylikorkala O, Viinikka L. Comparison between antifibrinolytic and antiprostaglandin treatment in the reduction of increased blood loss in women with intrauterine contraceptive devices. Br J Obstet Gynaecol 1983; 90: 78-83. 9. Wood C. The association of psycho-social factors and gynaecological symptoms. Aust Fam Physician 1978; (7 April): 471-478. 10. Lumley J, Wood C. Female reproductive system. In: Krupinski J, Stoller W, editors. North west region health and social survey. Melbourne: Heinemann, 1971: 52-63. 11. Coulter A, Klassen A, MacKenzie IZ, McPherson K. Diagnostic dilatation and curettage: is it used appropriately? BMJ 1993; 306: 236-239. 12. MacKenzie IZ, Bibby JG. Critical assessment of dilatation and curettage of 1029 women. Lancet 1978; 2: 566-568. 13. Vessey M, Clarke J, MacKenzie I. Dilatation and curettage in young women. Health Bull 1979; 39: 59-62. 14. Strovall T, Solomon S, Ling F. Endometrial sampling before hysterectomy. Obstet Gynecol 1989; 73: 405-409. 15. Goldberg G, Tsalacopoulos G, Davey D. A comparison of endometrial sampling with the Accurette and Vabra aspirator and uterine curettage. S Afr Med J 1982; 61: 114-116. 16. MacKenzie I. Routine outpatient diagnostic uterine curettage using a flexible plastic aspiration curette. Br J Obstet Gynaecol 1985; 92: 1291-1296. 17. Gillespie A, Nichols A. The value of hysteroscopy. Aust N Z J Obstet Gynaecol 1994; 34: 85-87. 18. Wood C, Hurley VA, Leoni M. The value of vaginal ultrasound in the management of menorrhagia. Aust N Z J Obstet Gynaecol 1993; 33: 198. 19. Fraser IS, McCarron G. Randomised trial of 2 hormonal and 2 prostaglandininhibiting agents in women with a complaint of menorrhagia. Aust N Z J Obstet Gynaecol 1991; 31: 66-70. 20. Dockeray CJ, Sheppard BL, Bonnar J. Comparison between mefenamic acid and danazol in the treatment of established menorrhagia. Br J Obstet Gynaecol 1989; 96: 840-844. 21. Bonnar J. Dysfunctional uterine bleeding. Presention at the Royal Society of Medicine, London, Feb 1994. London: The Royal Society, 1994. 22. Rybo G. Tranexamic acid therapy effective treatment in heavy menstrual bleeding. Clinical update on safety. Ther Adv 1991; 4: 1-8. 23. Preston JT, Cameron IT, Adams EJ, Smith SK. Comparative study of tranexamic acid and norethisterone in the treatment of ovulatory menorrhagia. Br J Obstet Gynaecol 1995; 102: 401-406. 24. Vermylen J, Verhaegen-Declereq ML, Verstraete M, Fierens F. A double blind study of the effect of tranexamic acid in essential menorrhagia. Thromb Diath Haemorrh 1968; 20: 583-587. 25. Fraser IS. Treatment of menorrhagia. Baillieres Clin Obstet Gynaecol 1989; 3: 391-402. 26. Fraser IS. Prostaglandins, prostaglandin inhibitors and menstrual disorders part II: menorrhagia and premenstrual syndrome. Healthright 1988; 8: 31-35. 27. Fraser IS, McCarron G, Markham R. Objective measurement of menstrual blood loss in women with a complaint of menorrhagia associated with pelvic disease or coagulation disorder. Obstet Gynecol 1986; 68: 630-633. 28. Cameron IT, Leask R, Kelly RW, Baird DT. The effects of danazol, mefenamic acid, norethisterone and a progesterone-impregnated coil on endometrial prostaglandin concentrations in women with menorrhagia. Prostaglandins 1987; 34: 99-110. 29. Nezhat C, Nezhat F, Silfer SL, et al. Laparoscopic myomectomy. Int J Fertil 1991; 36: 275-280. 30. Milsom I, Anderson K, Andersch B, Rybo G. A comparison of flurbiprofen, tranexamic acid, and a levonorgestrel-releasing intrauterine contraceptive device in the treatment of idiopathic menorrhagia. Am J Obstet Gynecol 1991; 164: 879-883. 31. Bonnar J, Sheppard BL. Treatment of menorrhagia during menstruation: randomised controlled trial of ethamsylate, mefenamic acid, and tranexamic acid. BMJ 1996; 313: 579-582. 32. Gannon M, Holt E, Fairbank J, et al. A randomised trial comparing endometrial resection and abdominal hysterectomy for the treatment of menorrhagia. BMJ 1991; 303: 1362-1364. 33. Dwyer N, Hutton J, Stirrat G. Randomised controlled trial comparing endometrial resection with abdominal hysterectomy for the surgical treatment of menorrhagia. Br J Obstet Gynaecol 1993; 110: 237-243. 34. Macdonald R, Phipps J, Singer A. Endometrial ablation -- a safe procedure. Gynaecol Endosc 1992; 1: 7-9. 35. Broadbent M, Magos AL. Endometrial resection follow up: late onset of pain. Br J Obstet Gynaecol . In press. 36. Sculpher MJ, Bryan S, Dwyer N, et al. An economic evaluation of transcervical endometrial resection versus abdominal hysterectomy for the treatment of menorrhagia. Br J Obstet Gynaecol 1993; 100: 244-252. 37. Wood C, Maher P, Hill D. Myoma reduction by electrocautery. Gynaecol Endoscopy 1994; 3: 163-165. 38. 38. Wood C, Maher P. Removal of fibromyomata by laparoscopic surgery after preoperative GnRH analogue -- an alternative to abdominal hysterectomy and myomectomy. Aust N Z J Obstet Gynaecol 1996. In press. 39. Maher P, Wood C, Hill D. Endoscopic minilaparotomy. Aust N Z J Obstet Gynaecol 1995; 35: 76-78. 40. Tavmergan E, Tavmergan EN, Turker S. Preliminary results of 100 pelviscopic myomectomies. 4th Congress of the European Society for Gynaecological Endoscopy, Brussels. 6-9 December. Gynaecol Endosc 1995; 4 Suppl I: 68. 41. Goldfarb HA. Electrocoagulation of myomas [abstract]. Fourth Biennial Meeting of the International Society of Gynaecologic Endoscopists, London, Apr 26-29, 1995. London: ISGE, 1995. 42. Kovac SR, Christie SJ, Bindbeutel GA. Abdominal versus vaginal hysterectomy: a statistical model for determining physician decision making and patient outcome. Med Decis Making 1991; 11: 19-28. 43. Wood C, Maher P, Hill D. Replacement of abdominal hysterectomy by the laparo vaginal technique -- its success and limitations. Aust N Z J Obstet Gynaecol 1994; 34: 71-74. 44. Jones IS, Flynn M, Hall B, et al. Laparoscopic assisted vaginal hysterectomy - an audit plus a word of caution. J Obstet Gynaecol 1995; 21: 119-125. 45. Garry R, Phillips G. How safe is the laparoscopic approach to hysterectomy.? Gynaecol Endoscopy 1995; 4: 77-79. 46. Wood C, Maher P. Laparoscopic hysterectomy. In: Wood C, Maher P, editors. Hysterectomy. London: Bailliere Tyndall, 1996. In press. Author's details Melbourne Gynoscopy Centre, Melbourne, VIC. Carl E Wood, FRACOG, Professor, Department of Obstetrics and Gynaecology, Monash University. Reprints: Professor C E Wood, Melbourne Gynoscopy Centre, 284 High Street, Ashburton, VIC 3147.