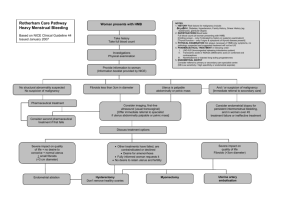
Post Menopausal Bleeding
Post Menopausal Bleeding
PMB
• Definition:
– An episode of bleeding 12 months or more after the
LMP.
• Common problem.
- Occurs in up to 10% women over 55yrs.
- Majority (about 90%) have a benign cause.
- No evidence of association with pattern of bleeding and malignancy eg: one off bleed vs regular bleeding.
• Main aim in primary care is to identify cause and exclude cancer:
• Start with detailed hx:
- identify risk factors
- drug hx HRT, tamoxifen, anticoagulants .
• Examination- abdominal for masses.
• PV- bimanual palpation to assess size, bulkiness uterus
• Speculum- to identify source- cervical malignancy or polyps, vaginal wall.
Causes PMB
• Endometrial carcinoma
• Cervical carcinoma
• Vaginal atrophy: decreased oestrogen leads to thinning of vaginal skin, thin pale vagina may bleed on contact
• Endometrial hyperplasia +/- polyp covers a wide range of changes in the endometrium, atypical hyperplasia is premalignant
• Cervical polyps: common in perimenopausal women, benign, pink protrusions from os.
• Hormone producing ovarian tumours- rare, produce oestrogen which causes hyperplasia.
Risk Factors for endometrial ca:
• Age
– peak incidence 65-75 yrs
– 93% diagnosed aged 50yrs and over
• PMH
– endometrial hyperplasia or polyps
– breast or ovarian ca
– DM
• Endogenous oestrogen excess
– obesity
– early menarche <12, late menopause >50
– nulliparity- pregnancy reduces risk by 30% after
1st birth and 25% after each subsequent
– PCOS
• Drug hx of exogenous oestrogen excess
– Unopposed oestrogen HRT
– Tamoxifen
• FH of HNPCC- patients have an 80% lifetime risk of developing endometrial ca
Making a Diagnosis:
• All women with PMB should be referred under 2ww .
• USS: TVUS is investigation of choice- can look at endometrial thickness, structural abnormalities, polyps, fibroids, exclude ovarian malignancy.
• Measuring endometrial thickness aims to identify those who are more likely to have underlying cancer
<4mm chance of cancer is 0.8%. SIGN guidelines recommend a thickness of <3mm can be used to exclude, locally guidelines are 4mm.
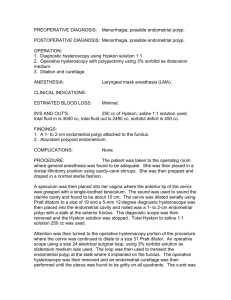
Investigations
• endometrial biopsy- effective screening for endometrial cancer. Blind sampling will miss some cancers.
• Hysteroscopy is the gold standard- allows direct visualisation of uterine cavity, assessment of structural abmormalities, directed biopsy of specific lesions. Indicated when sampling cannot be performed due to cervical stenosis or when bleeding persists after negative biopsy.
• One-stop gynae clinics.
Management of PMB
• Vaginal atrophy: oestrogen daily for 2 weeks, then once- twice weekly for maintenance.
• Polyps- removed as OP
• Endometrial hyperplasia- treated with IUS or progest
• Endometrial hyperplasia with atypia- should be treated as cancer.
Endometrial cancer treatment:
• Stage 1 TAH + BSO
• Stage 2 lymph node dissection, adjuvant chemo, radio.
Summary
• All women should be referred URGENTLY as endometrial cancer is present in approx 10% cases.
• Normal TVUSS with endometrial thickness
<4mm, with normal examination does not require further Ix providing bleeding has
STOPPED.