Mr James Campbell FRCOG
Background - Menstrual disorders
1 in 20 women aged 30-49 present to their
GP per year
£ 7 million (!) is spent per year on primary
care prescriptions
One of the most common reasons for
specialist referral
Accounting for a third of gynaecological
outpatient workload
Heavy menstrual bleeding (HMB)
Major impact on health-related quality of life
Major problem in public health
22% of otherwise healthy women
significant cost
invasive treatments
12% of all specialist referrals
Main presenting symptom for half of the
hysterectomies performed in the UK
Vessey M et al. The epidemiology of hysterectomy: findings of a large cohort study.
Br J Obstet Gynaecol 1992; 99; 402-407.
Increasing prevalence
More periods per lifetime
Earlier menarche
Increased life expectancy
Ability to regulate fertility
Less time spent breastfeeding
More demanding lifestyles and reduced
tolerance of troublesome periods
Menstruation
Shedding of the superficial layers
of the endometrium
following the withdrawal
of ovarian steroids
Normal menstruation
Menarche
Menopause
Regular cycles
Menstrual loss
Pelvic discomfort
- 13 years
- 51 years
– 5 / 28
– 40ml (<80ml)
Menstrual disorders
Heavy menstrual bleeding (HMB)
Intermenstrual / Postcoital bleeding
Dysmenorrhoea = ‘painful periods’
Premenstrual tension (PMT)
Post-menopausal bleeding
Oligo- or Amenorrhoea
HMB - Etiology
Endometrial origin
Uterine / pelvic pathology
Fibroids / Polyps
Pelvic infection (Chlamydia)
Endometrial or cervical malignancy
Medical disorders
Increased fibrinolysis and prostaglandins
Coagulopathy / Thyroid disease / Endocrine disorders
Iatrogenic (anti-coagulation / copper IUCDs)
Clinical evaluation
& management
Patient presenting
with
heavy menstrual bleeding
TAKE A HISTORY
Relevant history
Frequency and intensity of bleeding –
Menstrual diary
Pelvic pain / Pressure symptoms
Abnormal vaginal discharge
Sexual and contraceptive history
Obstetric history
Smear history
History of coagulation disorder
Examination
Clinical examination
General appearance (? Pallor)
Abdominal examination (?Pelvic mass)
Speculum examination
Assess
vulva, vagina and cervix
Bimanual examination
Elicit
tenderness
Elicit uterine / adnexal enlargement
Investigations
Indicated if age > 40 years
or failed medical treatment
FBC / Coagulation screen
Thyroid function (only if clinically indicated)
Smear / Endocervical swabs / High vaginal swabs
Pelvic ultrasound (USS)
Saline hysterosonography (?Polyps)
Hysteroscopy
Endometrial biopsy (Pipelle / D&C)
Hysteroscopy
Endometrial biopsy
Endometrial Hyperplasia
WHO Classification
Simple hyperplasia
No risk of malignant transformation
Complex hyperplasia
Low risk (~5%)
Simple atypical hyperplasia
Unknown risk
Complex atypical hyperplasia
Significant risk (at least 30%)
Endometrium: simple hyperplasia
Complex non-atypical hyperplasia
Complex atypical hyperplasia
Causes of HMB
Endometrial origin
“Dysfunctional uterine bleeding”
Anovulatory Cycles
Reasons for heavy menstrual bleeding
Endometrium develops
Corpus luteum fails to develop
under the influence of oestrogen
absence of progesterone
Spiral arteries do not develop properly and are
unable to undergo vasoconstriction at the time
of shedding
Endometrium supplied by thin-walled vessels
Result – prolonged heavy bleeding
Persistent Anovulation
Infertility
Endometrial hyperplasia
Increased risk of endometrial carcinoma
Management of HMB
Anti-fibrinolytics
Prostaglandin synthetase inhibitor
Tranexamic acid (Cyclokapron®)
Mefenamic acid (Ponstan®)
Combined oral contraceptive pill (COC)
Progestogens
GnRH analogues
Endometrial ablation
Hysterectomy
Management - Progestogens
Luteal phase progestogens
(only useful if anovulatory)
Long-acting progestogens
(Depoprovera / Implanon)
Mirena IUS
Mirena IUS
Endometrial ablation
Day-case procedure or out-patient setting
1st generation
2nd generation
Trans-cervical resection
Thermal balloon
Microwave
Impedance controlled
Similar outcome to Mirena IUS
Hysterectomy
“Treatment of choice for cancer,
but a choice of treatment for menorrhagia”
Lilford RJ (1997) BMJ 314; 160 - 161
Surgical access
Total versus subtotal hysterectomy
Removal versus conservation of ovaries
and use of HRT
Abdominal hysterectomy
Vaginal hysterectomy
Uterine pathology
Evaluation & Management
Polyps and Fibroids
Endometrial polyps
Localised overgrowths of endometrium projecting into
uterine cavity
Common in peri- and postmenopausal women
(10 – 24% of women undergoing hysterectomy)
Account for 25% of abnormal bleeding in both pre- and
postmenopausal women
Typically benign, but malignant change can rarely occur
Non-neoplastic lesions of endometrium containing
glands, stroma and thick-walled vessels
Glands may be inactive, functional or hyperplastic
Association with tamoxifen use
Endometrial Polyp
Endometrial polyps
Diagnosis
Pelvic USS / Saline hysterosonography
Hysteroscopy
Management
Operative removal with polyp forceps / curette
or hysteroscopic resection
Uterine Fibroids
(Leiomyomata)
Occur in 20 – 30% of women over 30 years
Usually multiple
Almost invariably benign
Variable sizes, up to 20 cm or more
Sex steroid-dependent – regress after the
menopause
Submucosal uterine fibroid
Leiomyoma with central degeneration
Leiomyoma
Uterine fibroids
Symptoms
50% asymptomatic
HMB / Dysmenorrhoea
Pressure effects
Infertility
Pregnancy complications
Diagnosis
Clinically enlarged uterus
Pelvic USS
Hysteroscopy / Laparoscopy
Uterine fibroids - Management
Conservative
Medical
Ensure Dx of fibroids and R/O adnexal mass
Tranexamic acid / NSAIDs
Mirena IUS
GnRH agonists
Surgical
Myomectomy
(hysteroscopic / laparascopic / by laparotomy)
Hysterectomy
Uterine artery embolization
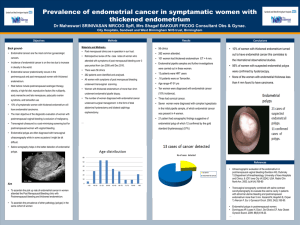
Postmenopausal bleeding
Evaluation
Postmenopausal bleeding (PMB)
ALL WOMEN WITH PMB
MUST BE INVESTIGATED
Purpose of investigation:
Exclude malignancy of endometrium and cervix
Endometrial Ca in up to 4% of women with PMB
Precursors of endometrial Ca
(complex hyperplasia +/- atypia)
PMB – Exclude malignancy
History and assessment of risk factors
Clinical Examination (!)
R/O cervical carcinoma
Trans-vaginal USS
Use of HRT / Tamoxifen / BMI / Family Hx
Assessment of endometrial thickness (<3mm)
Endometrial sampling (+/- uterine evaluation)
Treatment for endometrial Ca
Hysterectomy +/- radiotherapy
Endometrial Carcinoma
Type I
Oestrogen dependent
80%
Low grade
Endometrioid histology
Assoc with obesity (40%), nulliparity, late menopause, tamoxifen
Type II
Non-oestrogen dependent
Older postmenopausal women
High grade
Serous, clear cell and mixed histology
Tamoxifen; no association with hyperoestrogenism or hyperplasia
Aggressive behaviour
Endometrioid carcinoma
Endometrioid Carcinoma
Endometrial Carcinoma
Prognostic Factors
Histological type
Histological grade
Depth of myometrial invasion
Lymphovascular space invasion
FIGO stage
Case 1
43 year old, para 2 + 0, company executive
Presenting complaint
History
excessive menstrual blood loss
requirement for contraception
Menarche aged 13 years
Used OC pill until 35 years
Smokes 15 / day
Examination
Normal sized uterus and normal adnexae
Case 2
38 year old, para 0 + 0, primary school teacher
Presenting complaint
History
excessive menstrual blood loss and dysmenorrhoea
Menarche aged 12 years
Used OC pill until 25 years
Currently using tranexamic acid with unsatisfactory effect
Examination
Uterus appears enlarged to 18/40 size
Case 3
59 year old, para 0 + 0, retired
Presenting complaint
vaginal bleeding on two occasions over last 3 months
History
Menopause aged 49 years
Polycystic ovarian syndrome
Infertility
BMI = 38 / Overweight for many years
How would you evaluate this case?
Would you carry out any investigations?
What management options would you
discuss and recommend?