to view the abstract for Dr. Jafri`s presentation - Custom
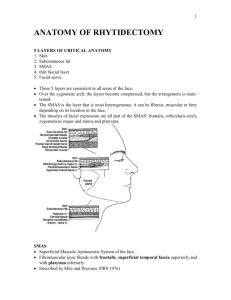
advertisement

Custom-Lift: technical modification of the MACS / Short Scar Facelift technique incorporating cranial suspension with anterior SMASectomy/plication techniques KS Jafri, MD Objective: to evaluate the clinical efficacy of a modified facial rejuvenation / rhytidectomy surgical technique (Custom-Lift) in addressing the subjective and objective concerns of the aging face patient. Design: retrospective clinical case study review Patients: 10 patients (8 female, 2 male) ranging in age from 42 to 65. Patients had mild to moderate aging face changes (jowls, inferior descent of facial soft tissues, rhytids, skin laxity). Patients with excessive skin laxity or moderate to severe facial aging changes were excluded from the study. Patients with any medical condition contraindicating the use of local anesthesia or undergoing elective surgery were excluded from the study. Materials & Methods: 10 patients electively underwent a modified MACS / Short Scar facelift (Custom-Lift) between November 2007 and March 2008. Patients presented for clinical examination, review of past medical / surgical history, review of objective and subjective concerns and review of the informed consent documents prior to undergoing the procedure. Patients admitted to the study were limited to those with mild-moderate aging face changes and overall good skin elasticity. Preoperative photos and surgical markings were made prior to prepping and draping the patient in a sterile manner. Tumescent anesthesia (1% xylocaine, 1:100,000 epinephrine, normal saline and sodium bicarbonate) was injected in a sterile manner with 10cc syringes and 27gauge needles to provide effective anesthetic comfort for the patients during the procedure. The surgical procedure (Custom-Lift) incorporated a variable length pre-auricular incision based on the MACS / Short Scar Facelift technique. A variable length skin flap was elevated to expose the SMAS from the inferior temporal fascia to the superior platysma and to the anterior border of the parotid fascia. A 1cm pocket was created anterior to the superior helix and superior to the zygomatic arch. The pocket was created to the depth of the deep temporal fascia. A 2.0 PDS suture (females) or 0.0 PDS suture (males) was then used to create a “purse string” suture anchored to the deep temporal fascia and temporal periosteum and incorporating the SMAS from the temporal fascia to the platysma muscle. The “purse string” suture was U-shaped and the width and length of the U were customized to each individual patient’s anatomic needs in order to optimize the clinical results achieved. The PDS suture was secured with several knots which were buried by suturing the overlying tissues together with a 4.0 Vicryl suture. Next, an anterior SMASectomy was performed at the anterior / inferior border of the parotid fascia. The length and orientation of the SMASectomy maneuver was again customized to each individual patient’s clinical needs. In patients with thin faces or gaunt facial tissues, a SMAS plication was performed in lieu of SMASectomy in order to help provide volume replacement / restoration in a desired location. Skin excision and closure were done in accordance with the well described MACS /Short Scar Facelift techniques. Antibiotic dressings and facial support wrap were used for 24 hours postop. Oral antibiotics were given for one week postop and oral analgesics were prescribed on a PRN basis. Patients were seen for follow up at 24 hours, 1 week, 3 weeks, 3 months and one year after surgery. At each visit objective and subjective exams were performed and documented in order to analyze clinical effectiveness of the described procedure in addressing the aging face concerns of the patients. Results: All patients reported overall subjective and objective satisfaction with the results of their procedure at the one year mark. 60% of patients reported they were “extremely satisfied”, 30% “very satisfied” and 10% “satisfied”. There were no reports of excessive pain, swelling, bruising, facial weakness, facial asymmetry, infections, skin loss, hematoma, seroma or other major or minor complications. At one year after their individual procedure, patients reported the greatest satisfaction with the appearance of their jaw line / jowls (70% “extremely satisfied”, 30% “very satisfied”), facial volume (30% “extremely satisfied”, 60% “very satisfied”, 10% “satisfied”), softening of the prejowl sulcus (50% “extremely satisfied”, 40% “very satisfied”, 10% “satisfied”) and softening of the inferior nasolabial-fold (20% “extremely satisfied”, 50% “very satisfied”, 30% satisfied) at one year after their individual procedures. Physical exam and comparison of pre-operative photos to post-operative photos provided compelling and objective support for subjective findings. Conclusions: the advent and efficacy of “minimally invasive” rhytidectomy procedures has been well documented in the medical literature in specific regards to the MACS / Short Scar Facelift procedures. The author has employed these techniques in his private practice with great success but felt that a modification of these existing techniques would provide a more effective way of addressing variations in individual patient anatomy. The modifications incorporated included the use of a variable size to the U-shaped “purse string” as originally described in the MACS / Short Scar Facelift. The major modification employed was to utilize an anterior SMASectomy (or SMAS plication) as opposed to the O-shaped “purse string” suture described in the MACS / Short Scar Facelift techniques. It was the author’s perspective and experience that the anterior SMASectomy would provide a more effective way of addressing the pre-jowl sulcus and inferior nasolabial fold than the existing maneuvers present in the MACS / Short Scar Facelift techniques. It has been the author’s experience and clinical findings that these modifications have provided a safe, effective and highly customizable approach to facial rejuvenation in patients with mild to moderate aging face changes and concerns. Further clinical studies with a larger patient population and long term follow up (5 years) will be needed to further assess the clinical impact of the Custom-Lift facial rejuvenation procedure.