PPT - UCLA Head and Neck Surgery
advertisement
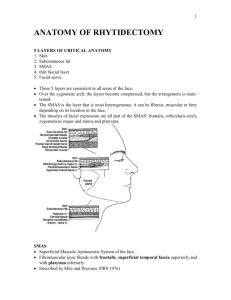
Rhytidectomy Marc Cohen, M.D. David Geffen School of Medicine at UCLA Division of Head & Neck Surgery The Aging Face Soft tissue changes Skin changes Soft Tissue Changes Jowl Deepened nasolabial folds and perioral jowling Platysmal banding and submental fullness Orbicularis oculi and malar fat pad ptosis Skin Changes Epidermis and subcutaneous fat thins Flattening of dermal-epidermal junction Elastosis: progressive loss of organization of elastic fibers and collagen Photodamaged skin – striking variability SMAS Superficial Musculoaponeurotic System 1976 Mitz and Pyronie Landmark paper Fibromuscular fascial extension of the platysmal muscle that arises superiorly from the fascia over the zygomatic arch and is continuous in the inferior cheek with the platysma Functions to transmit the activity of facial mimetic muscles to the facial skin SMAS Posteriorly, the SMAS fuses with the fascia overlying the sternocleidomastoid muscle, but it is a distinct layer superficial to the parotid fascia Anterosuperiorly, the SMAS invests the facial mimetic muscles of the mid-face (i.e., orbicularis oculi, zygomatic major/minor, levator labii superioris) Anteriorly, the SMAS invests the superficial portions of the orbicularis oris and gives off fibrous septae that insert into the dermis along the melolabial crease and upper lip Facial Nerve Protected by parotid tissue and lower branches are deep to masseter fascia Potential space exists between SMAS and masseter fascia in inferior cheek Important in deep/composite rhytidectomy techniques Innvervates midfacial mimetic muscles from undersurface Facial Nerve Temporal branch is most superficial Crosses junction of anterior 1/3 and posterior 2/3 of zygomatic arch Above the arch it travels in the temporoparietal fascia to innervate frontalis and orbicularis oculi SMAS & The Facial Nerve Facelifts Subperiosteal facelift Subperiosteal facelift Shortcomings Frontal branch at higher risk Significant facial edema lasting up to 6 weeks Deep plane facelift Addresses nasolabial folds Subcutaneous 2-3 cm in front of tragus Sub-SMAS To zygomaticus major Superficial to zygomaticus major Upper extent is malar eminence Inferior extent is jawline Deep plane facelift Composite facelift Addresses malar eminence Lower blepharoplasty incision used to elevate orbicularis oculi and malar fat pad Transition then made superficial to zygomaticus major Nasolabial Fold Nasolabial Fold Boundary between cheek and upper lip Laterally, thick subcutaneous layer Medially, dermis almost approaches orbicularis Cheek fat sags over time lateral to fold Upper third – insertion into LLSAN muscle Middle third – transition btw both muscles Lower third – insertion into OO Deep plane and periosteal lifts do not anatomically address this Controversial – SMAS or not Nasolabial Fold Management Direct excision (UCLA) ePTFE (gortex) Fillers SMAS Facelifts? Midface lifts? Botox (LLSAN) Botox Direct Excision Lift and Peel at same time? Concern for flap necrosis Retrospective studies show no increased incidence of flap necrosis or other complications Retaining Ligaments of the Face Osteocutaneous Orbital – centered at zygomaticofrontal suture Zygomatic Buccal-maxillary – arises from zygomaticomaxillary suture Mandibular (along with DAO makes up labiomandibular crease) Fasciocutaneous Masseteric (anterior border of masseter Parotidocutaneous Blood Supply ECA STA Transverse facial artery Zygomaticorbital artery Facial Submental Inferior labial Superior labial Angular Blood Supply Complications - Hematoma HTN is major risk factor (2.6x risk) Major – usually occur in first 12 hours reoperation and exploration Minor – occur during the first week Evacuated with 18 ga needle or small opening in incision line, pressure dressing, abx Complications – Flap necrosis Postauricular is most common site Preauricular is 2nd most common Deep-plane facelifts have a decreased incidence of necrosis Nicotine carries a 12.6x risk for flap necrosis Must stop at least 2 weeks prior Treat conservatively with with daily peroxide cleaning, limited debridement, and topical abx ointment Most heal nicely Complications – Nerve Damage Most commonly injured nerve is great auricular If injured, should be repaired with 9-0 nylon Temporal and Marginal are the most commonly injured motor nerves Studies differ on which is more commonly injured (which technique, etc.) Treatment First 4-8 hours, wait If prolonged, do NOT re-explore 85% will resolve with time Reconstruct after 1 year Patients with a hx of Bell’s palsy are at risk for recurrence after rhytidectomy Complications Hypertrophic scarring Occurs with excessive tension on flap closure More commonly with isolated subcutaneous flap dissections Treat with steroids Defer excision and primary closure until at least 6 months postoperatively Alopecia Wait 3-6 months, then excise or place grafts Complications Infection Common pathogens are staph and strep Usually respond to oral abx Rare for abscess to form Earlobe deformity (pixie ear) V-Y plasty performed 6 months after surgery Complications Parotid injury Sialocele or fistula Needle aspiration and pressure dressings