Peripheral venous cannula insertion and management Adults policy
advertisement
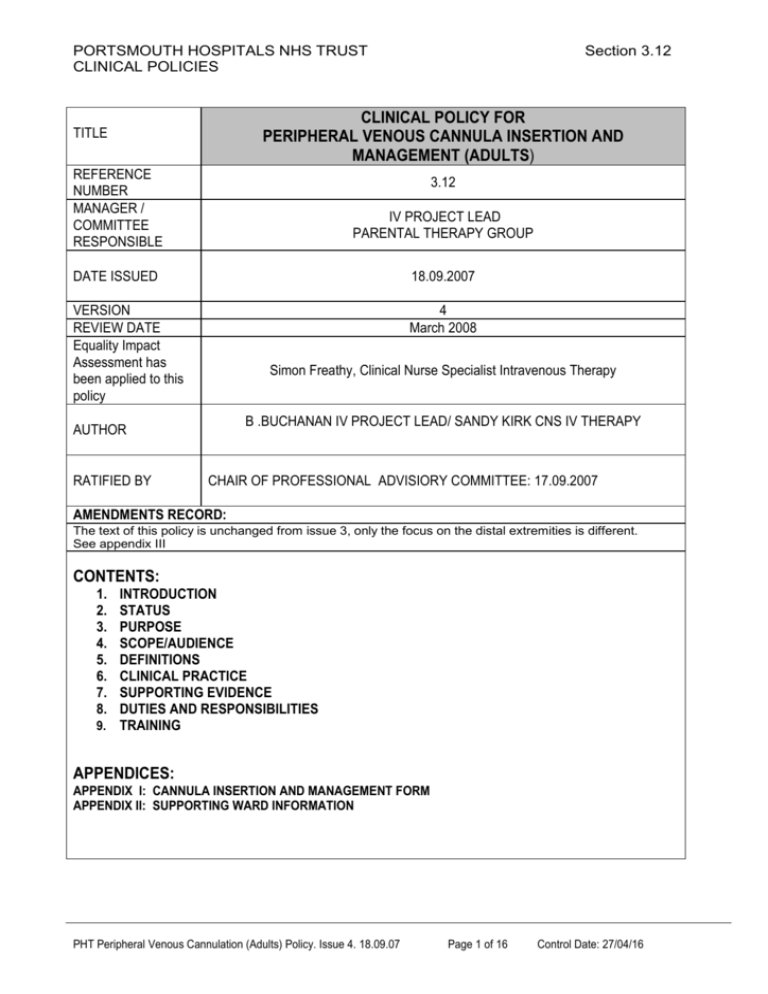
PORTSMOUTH HOSPITALS NHS TRUST CLINICAL POLICIES Section 3.12 CLINICAL POLICY FOR PERIPHERAL VENOUS CANNULA INSERTION AND MANAGEMENT (ADULTS) TITLE REFERENCE NUMBER MANAGER / COMMITTEE RESPONSIBLE 3.12 IV PROJECT LEAD PARENTAL THERAPY GROUP DATE ISSUED 18.09.2007 VERSION REVIEW DATE Equality Impact Assessment has been applied to this policy 4 March 2008 Simon Freathy, Clinical Nurse Specialist Intravenous Therapy B .BUCHANAN IV PROJECT LEAD/ SANDY KIRK CNS IV THERAPY AUTHOR RATIFIED BY CHAIR OF PROFESSIONAL ADVISIORY COMMITTEE: 17.09.2007 AMENDMENTS RECORD: The text of this policy is unchanged from issue 3, only the focus on the distal extremities is different. See appendix III CONTENTS: 1. 2. 3. 4. 5. 6. 7. 8. INTRODUCTION STATUS PURPOSE SCOPE/AUDIENCE DEFINITIONS CLINICAL PRACTICE SUPPORTING EVIDENCE DUTIES AND RESPONSIBILITIES 9. TRAINING APPENDICES: APPENDIX I: CANNULA INSERTION AND MANAGEMENT FORM APPENDIX II: SUPPORTING WARD INFORMATION PHT Peripheral Venous Cannulation (Adults) Policy. Issue 4. 18.09.07 Page 1 of 16 Control Date: 27/04/16 PORTSMOUTH HOSPITALS NHS TRUST Section 3.12 CLINICAL POLICIES 1. INTRODUCTION This policy will provide information about the correct technique for peripherally cannulating a vein aseptically and the subsequent care of the peripheral venous cannulae. By using this policy the user will act to reduce the risks to patients and staff associated with peripheral venous cannulation. These include thrombosis, pain, local or systemic infection; occupational sharps injury and inappropriate cannula insertion. Aseptic peripheral venous cannulation is undertaken to provide venous access for either diagnostic or therapeutic purposes: a) Short-term intravenous fluid therapy of usually less than 3-4 days (if intravenous access is needed for longer periods, other options should be considered). b) Administration of bolus injections in outpatients or in day case surgery c) Vascular access for fluids or drugs at time of particular procedure e.g. surgery, endoscopy The implementation of this policy will be monitored using clinical audit. !0 cannula audits monthly. (appendix I) 2. STATUS Clinical Policy 3. PURPOSE To inform best practice on the aseptic insertion of peripheral venous cannulation of adults. The implementation of this policy will reduce the risks associated with this procedure including thrombosis, pain, local or systemic infection; occupational sharps injury and inappropriate cannula insertion. 4. SCOPE/AUDIENCE This policy applies to all health care professionals performing cannulation in the Trust. For cannulation in paediatric areas, please refer to Infection Control. 5. DEFINITIONS Aseptic Technique Clinical practices used to protect the patient from micro-organisms by preventing contamination of wounds, manipulated devices and other susceptible sites. Aseptic technique involves the use of appropriate hand hygiene, use of sterile equipment, no touch technique and robust patient skin / site disinfection. Venous Cannulation Procedure for insertion of a hollow fine bore tube into the venous system Health care professional A registered or trained member of staff, including but not exclusively nurses, doctors and operating department practitioners. Infection Entry of a harmful microbe into the body and its multiplication in the tissues PHT Peripheral Venous Cannulation (Adults) Policy. Issue 4. 18.09.07 Page 2 of 16 Control Date: 27/04/16 PORTSMOUTH HOSPITALS NHS TRUST CLINICAL POLICIES Section 3.12 Peripheral cannula A specifically-designed flexible tube designed for insertion into a blood vessel, with a proximal connector to allow injection or infusion of liquids. Sizes range from blue 22g, pink 20g, green 18g, grey 16g and orange 14g. 22-20g are optimal for administration of intermittent medications. 16- 14g are routinely used to administer fluids in acute situations i.e. haemorrhage Phlebitis Inflammation of a vein Thrombosis Formation, development or existence of a blood clot within the vascular system 6. CLINICAL PRACTICE Action Identify clinical need for cannula insertion Identify patient by surname, first name and date of birth Explain the procedure to the patient, discuss the need for a cannula, obtaining verbal consent for procedure establishing whether patient has any known allergies Explain to the patient the importance of keeping the site clean and dry and advise of risks of infection Collect equipment needed including: Dressing trolley Sterile field with dressing pack or proprietary cannulation pack Single use tourniquet Sterile gloves Sharps box 2% Chlorhexidine and 70% alcohol (Deb) skin preparation Local anaesthetic (1% lidocaine) orange needle and 2ml syringe/ insulin syringe Cannulae - IV dressing Saline flush Wash hands with soap and water as per the Trust Hand Hygiene Policy Place opened dressing / cannulation pack onto clean dressing trolley. Open sterile packs and lay out equipment within the sterile field. Sanitise hands with alcohol gel or wash with soap and water Palpate potential sites these include: The hand - a lower risk of phlebitis The wrist or upper arm – increasing risk The lower limb has a higher risk than the upper limb When potential site is identified position patient comfortably with appropriate limb below the level of the heart. Removing excess hair (shaving is not recommended – clippers are better) Rationale To prevent inappropriate insertion and exposure to associated risks. To ensure correct identification of the patient To ensure patient is informed of procedure and the risk of allergic reaction is minimised To ensure patient compliance and reduce risk of infection To ensure procedure is performed without disruption Choice of cannula must be based on clinical need but the smallest cannula should be chosen to reduce risk of complications associated with larger bores. To reduce the risk of infection To reduce the risk of infection To reduce risk of arterial rather than venous cannulation, and reduce risk of infection. To allow dependent veins to fill with blood Local trauma can be caused by shaving, increasing risk of infection PHT Peripheral Venous Cannulation (Adults) Policy. Issue 4. 18.09.07 Page 3 of 16 Control Date: 27/04/16 PORTSMOUTH HOSPITALS NHS TRUST CLINICAL POLICIES Section 3.12 Action Apply proximal single use tourniquet, without obstructing arterial flow Optimal time for application is 3 to 5 mins – if additional time is needed release tourniquet as vein will tend to “disappear”. Encourage patient to exercise limb muscles (e.g. repeatedly making a fist and opening hand) Sanitise hands with alcohol gel or wash with soap and water and don sterile gloves Clean insertion site using a spiral motion from the proposed puncture site outwards with 2% chlorhexidine in 70% alcohol (from a bottle or pre-soaked wipe) for 30 seconds and then allow to dry Administer local anaesthetic (1% lidocaine) which should be encouraged in all but the most urgent of cases. Alternatively apply prescribed topical local anaesthetic cream 45mins prior to procedure Inserting the cannula: Gently pull on skin, distal and lateral to insertion site. Do not touch the cannula or the insertion site. Insert cannula (bevel uppermost) through the cleaned skin area at an angle of 20 degrees. Advance until just in the vein and then lower the cannula until it is parallel with the skin (a flashback of blood is usually but not always seen at this point) Rationale To distend veins Muscle pump forces blood into veins to distend them further To reduce the risk of infection To reduce risk of infection To ensure patient comfort To “fix” the skin and the superficial veins underlying it. To use the sharpened needle to introduce the plastic cannula into the vein. Then, either; a) Pull the needle back 1cm and push the cannula/needle into the vein up to the hilt Or; b) Hold the needle still and advance the cannula over the needle until the cannula is inserted up to the hilt To introduce the cannula fully into the vein In the event of unsuccessful cannulation of the vein withdraw the cannula from the puncture site and apply pressure with non woven swab To minimise haematoma formation and /or excessive bruising Prior to subsequent attempts at cannulation it is the responsibility of the individual practitioner to risk assess the difficulty of further attempts against their own registered competence and experience. If the practitioner anticipates the difficulty level to be beyond their scope of practice, then referral to more experienced, competent practitioners should be made Remove the tourniquet and apply pressure on the proximal vein, close to the tip of the cannula – a second person may be required for this Remove needle and dispose of immediately into sharps container, cap off cannula with a sterile cap or attach intravenous fluids as appropriate To ensure cannulation is always undertaken by competent practioners and minimise risks associated with failed attempts at gaining venous access To prevent excessive bleeding during needle-removal. To reduce risk of needle stick injury and prevent blood spillage. PHT Peripheral Venous Cannulation (Adults) Policy. Issue 4. 18.09.07 Page 4 of 16 Control Date: 27/04/16 PORTSMOUTH HOSPITALS NHS TRUST CLINICAL POLICIES Secure cannula with a recognised, sterile cannula dressing, ensuring it is applied correctly (non-sterile, sticky-tape fixation or bandage is NOT acceptable). Place ‘date for cannula review’ sticker to outside of dressing Flush cannula with 1-2 ml saline if not being attached to infusion. Document cannula insertion and removal by completing a Cannula insertion and management form for each separate cannula inserted. Once cannula has been removed this document is filed in the patients medical notes. DAY CASE patient’s cannula need only to be documented fully in the notes. A cannula insertion and management form is NOT required. Section 3.12 To reduce risk of infection and secure cannula in position To ensure timely review To ensure cannula patency To establish an audit trail and monitor management of cannula. Cannula insitu for short period of time and then removed. Ongoing cannula management: Decontaminate hands before and after each patient contact. Use correct hand hygiene procedure as per trust policy. Always access cannula by cleaning with 2% chlorhexidine and 70% isopropyl alcohol, and allow to dry before administering fluid or injections. Swanlocks (bungs) should NOT be applied directly onto the cannula; single or double lumen extensions should be applied. Cannula site should be inspected at least twice a day and documented on the form. Cannula dressing should be, intact, dry and adherent. A date and time of insertion must be applied at point of insertion. Remove cannula if there is no continuing clinical indication. Replace cannula in a new site after 72-96 hours, earlier if clinically indicated. Administration sets should be replaced immediately after blood and blood product administration, intermittent IV antibiotics and medicines. Heparin infusion lines should be replaced every 24 hours. All other fluid sets should be replaced after 72 hours. ALL giving sets should be labelled with date and time on commencement of use. To reduce the risk of infection To reduce the risk of infection To prevent unwanted movement of cannula in the vein. Thus causing phlebitis. Observe for signs of infection or phlebitis. To ensure that the cannula is replaced or removed on time, thus reducing the risk of infection. To reduce the risk of infection To reduce the risk of infection To reduce the risk of infection PHT Peripheral Venous Cannulation (Adults) Policy. Issue 4. 18.09.07 Page 5 of 16 Control Date: 27/04/16 PORTSMOUTH HOSPITALS NHS TRUST CLINICAL POLICIES 7. Section 3.12 SUPPORTING EVIDENCE Department of Health (2001) The epic Project: Developing National Evidence – based Policys for Preventing healthcare associated Infections Journal of Hospital Infection (2001) 47 (supplement) Donaldson I. (1999) Intravenous therapy in critically ill adults: developing a clinically and costeffective approach Intensive and Critical Care Nursing No 15, 338-345 Dougherty L, Mallett J (2001) The Royal Marsden Hospital Manual of Clinical Nursing Procedures Fifth edition. Blackwell Science Fletcher SJ; Bodenham A (1999) Catheter related sepsis: an overview – Part 1 British Journal of Intensive Care. March/April Infection Control Nurses Association (2001) Policys for preventing intravascular catheter related infection NICE (2003) (No. 4) Care of patients with central venous catheters Clinical policy 2 – Infection control, June 2003 Polderman KH; Girbes AR (2002) Central venous catheter use. Part 2: infectious complications Intensive Care medicine 2002, Jan; 28(1): 18-28 Portsmouth Hospitals NHS Trust Policys Infection Control Policys - Intravenous Cannulation and Infusion therapy Blood Transfusion Policy (Adult0 RCN (March 2004) Good practice in infection control – Guidance for nursing staff RCN (Oct 2003) Standards for infusion therapy DoH ( July 2006) winning ways high impact working together to reduce healthcare associated infection in England-intervention 2b 8. DUTIES AND RESPONSIBILITIES Supervisors of clinical practice will be responsible for monitoring compliance with the policys on an Ongoing basis. The IV therapy Nurses will audit compliance as part of the infection control clinical practice audit process. A snapshot audit to monitor clinical practice during cannula insertion and subsequent care will be undertaken annually. PHT Peripheral Venous Cannulation (Adults) Policy. Issue 4. 18.09.07 Page 6 of 16 Control Date: 27/04/16 PORTSMOUTH HOSPITALS NHS TRUST CLINICAL POLICIES Section 3.12 9. TRAINING Prior to undertaking any cannulation procedure, all staff must be able to demonstrate clinical competence and a clear understanding of the underlying principles of practice. This will be achieved by: Nursing and other health care staff; a) b) c) complete the Trust venous cannulation competency pack attend a cannulation study day complete a period of supervised clinical practice (Staff who have been trained and practised in a previous post may be allowed to demonstrate an equivalent level of competence through a period of supervised practice only). Medical staff; Post registration house officer (PRHO) induction will include training by Trust trainers on local policys and principles of practice. Senior House Officer’s and Registrars will be assumed competent unless identified otherwise by their supervisor. If problems are identified, the staff member will be required to: a) complete the Trust venous cannulation competency pack b) attend a cannulation study day c) complete a period of supervised clinical practice PHT Peripheral Venous Cannulation (Adults) Policy. Issue 4. 18.09.07 Page 7 of 16 Control Date: 27/04/16 PORTSMOUTH HOSPITALS NHS TRUST Section 3.12 CLINICAL POLICIES APPENDIX I: CANNULA INSERTION AND MANAGEMENT FORM FORM AVAILABLE FROM MEDICAL PHOTOGRAPHY (EXT3370). FORM NO: 08246 PHT Peripheral Venous Cannulation (Adults) Policy. Issue 4. 18.09.07 Page 8 of 16 Control Date: 27/04/16 PORTSMOUTH HOSPITALS NHS TRUST CLINICAL POLICIES Section 3.12 APPENDIX II: SUPPORTING INFORMATION FOR CLINICAL AREAS PHT Peripheral Venous Cannulation (Adults) Policy. Issue 4. 18.09.07 Page 9 of 16 Control Date: 27/04/16 PORTSMOUTH HOSPITALS NHS TRUST CLINICAL POLICIES Section 3.12 Abbreviated guide to peripheral venous cannulation (adult.) Clinical Practice Policy (abbreviated) Action Identify clinical need for cannula insertion Identify patient by surname, first name and date of birth Explain the procedure to the patient, discuss the need for a cannula, obtaining verbal consent for procedure establishing whether patient has any known allergies Explain to the patient the importance of keeping the site clean and dry and advise of risks of infection Collect equipment needed including: Dressing trolley Sterile field with dressing pack or proprietary cannulation pack Single use tourniquet Sterile gloves Sharps box 2% Chlorhexidine and 70% alcohol (Deb) skin preparation Local anaesthetic (1% lidocaine) orange needle and 2ml syringe Cannulae - IV dressing Saline flush Wash hands with soap and water as per the Trust Hand Hygiene Policy Place opened dressing / cannulation pack onto clean dressing trolley. Open sterile packs and lay out equipment within the sterile field. Sanitise hands with alcohol gel or wash with soap and water Palpate potential sites these include: The hand - a lower risk of phlebitis The wrist or upper arm – increasing risk The lower limb has a higher risk than the upper limb When potential site is identified position patient comfortably with appropriate limb below the level of the heart. Removing excess hair (shaving is not recommended – clippers are better) Apply proximal single use tourniquet, without obstructing arterial flow Optimal time for application is 3 to 5 mins – if additional time is needed release tourniquet as vein will tend to “disappear”. Encourage patient to exercise limb muscles (e.g. repeatedly making a fist and opening hand) Sanitise hands with alcohol gel or wash with soap and water and don sterile gloves Clean insertion site using a spiral motion from the proposed puncture site outwards with 2% chlorhexidine in 70% alcohol (from a bottle or pre-soaked wipe) for 30 seconds and then allow to dry Administer local anaesthetic (1% lidocaine) which should be encouraged in all but the most urgent of cases. Alternatively apply prescribed topical local anaesthetic cream 45mins prior to procedure Inserting the cannula: Gently pull on skin, distal and lateral to insertion site. Do not touch the cannula or the insertion site. Insert cannula (bevel uppermost) through the cleaned skin area at an angle of 20 degrees. Advance until just in the vein and then lower the cannula until it is parallel with the skin (a flashback of blood is usually but not always seen at this point) PHT Peripheral Venous Cannulation (Adults) Policy. Issue 4. 18.09.07 Page 10 of 16 Control Date: 27/04/16 PORTSMOUTH HOSPITALS NHS TRUST CLINICAL POLICIES Section 3.12 Then, either; b) Pull the needle back 1cm and push the cannula/needle into the vein up to the hilt Or; b) Hold the needle still and advance the cannula over the needle until the cannula is inserted up to the hilt In the event of unsuccessful cannulation of the vein withdraw the cannula from the puncture site and apply pressure with non woven swab Prior to subsequent attempts at cannulation it is the responsibility of the individual practitioner to risk assess the difficulty of further attempts against their own registered competence and experience. If the practitioner anticipates the difficulty level to be beyond their scope of practice, then referral to more experienced, competent practitioners should be made Remove the tourniquet and apply pressure on the proximal vein, close to the tip of the cannula – a second person may be required for this Remove needle and dispose of immediately into sharps container, cap off cannula with a sterile cap or attach intravenous fluids as appropriate Secure cannula with a recognised, sterile cannula dressing, ensuring it is applied correctly (non-sterile, sticky-tape fixation or bandage is NOT acceptable). Place ‘date for cannula review’ sticker to outside of dressing Flush cannula with 1-2 ml saline if not being attached to infusion. Document cannula insertion and removal by completing a Cannula insertion and management form for each separate cannula inserted. Once cannula has been removed this document is filed in the patients medical notes. DAY CASE patient’s cannula need only to be documented fully in the notes. A cannula insertion and management form is NOT required. Ongoing cannula management: Decontaminate hands before and after each patient contact. Use correct hand hygiene procedure as per trust policy. Always access cannula by cleaning with 2% chlorhexidine and 70% isopropyl alcohol, and allow to dry before administering fluid or injections. Swanlocks (bungs) should NOT be applied directly; single or double lumen extensions should be applied. Cannula site should be inspected at least twice a day and document on form Cannula dressing should be, intact, dry and adherent. A date and time of insertion must be applied at point of insertion. Remove cannula if there is no continuing clinical indication. Replace cannula in a new site after 72-96 hours, earlier if clinically indicated. Administration sets should be replaced immediately after blood and blood product administration, intermittent IV antibiotics and medicines. Heparin infusion lines should be replaced every 24 hours. All other fluid sets should be replaced after 72 hours. ALL giving sets should be labelled with date and time on commencement of use. PHT Peripheral Venous Cannulation (Adults) Policy. Issue 4. 18.09.07 Page 11 of 16 Control Date: 27/04/16 PORTSMOUTH HOSPITALS NHS TRUST CLINICAL POLICIES No needle free injectable bungs should be applied directly onto indwelling cannulae; these components are designed for use in long dwell central venous access devices only For further information please contact the: IV therapy team Infection control department Pathology Laboratory E Level Queen Alexandra Hospital Cosham (02392) 286000 Ext.1744 / Clinical lead bleep 1494 PHT Peripheral Venous Cannulation (Adults) Policy. Issue 4. 18.09.07 Section 3.12 Cannulae that are anticipated to be accessed intermittently should have a single access extension line deployed to minimise increased risks of mechanical phlebitis associated with direct cannulae access In cases of concurrent therapy a double lumen device should be deployed thus facilitating access to the closed IV circuit following appropriate decontamination Page 12 of 16 Control Date: 27/04/16 PORTSMOUTH HOSPITALS NHS TRUST CLINICAL POLICIES Section 3.12 1. Explain the procedure to the patient, discuss the need for a cannula, obtaining verbal consent for procedure. Establishing whether patient has any known allergies. Collect equipment needed 2. Clean insertion site using a spiral motion from the proposed puncture site outwards with 2% chlorhexidine in 70% alcohol (from a bottle or pre-soaked wipe) Apply tourniquet, perform hand hygiene and don latex free sterile gloves, a sterile field can be deployed as per individual practitioner preference 3. Administer intradermal local anaesthetic ( 1% lidocaine) PHT Peripheral Venous Cannulation (Adults) Policy. Issue 4. 18.09.07 4.Gently pull on skin, distal and lateral to insertion site. Do not touch the cannula or the insertion site. Insert cannula (bevel uppermost) through the cleaned skin area at an angle of 20 degrees Page 13 of 16 Control Date: 27/04/16 PORTSMOUTH HOSPITALS NHS TRUST CLINICAL POLICIES Section 3.12 a) Pull the needle back 1cm and push the cannula/needle into the vein up to the hilt Or; b) Hold the needle still and advance the cannula over the needle until the cannula is inserted up to the hilt 6. Remove the tourniquet and apply pressure on the proximal vein, close to the tip of the cannula – a second person may be required for this 8. Flush cannula with 1-2 ml saline if not being attached to infusion. 10. Place ‘date of insertion’ sticker to outside of dressing PHT Peripheral Venous Cannulation (Adults) Policy. Issue 4. 18.09.07 9. Secure cannula with a recognised, sterile cannula dressing, ensuring it is applied correctly (non-sterile, sticky-tape fixation or bandage is NOT acceptable). 11. Cannulae that are anticipated to be accessed intermittently should have a single access extension line deployed to minimise increased risks of mechanical phlebitis associated with direct cannulae access In cases of concurrent therapy a double lumen device should be deployed thus facilitating access to the closed IV circuit following appropriate decontamination Page 14 of 16 Control Date: 27/04/16 PORTSMOUTH HOSPITALS NHS TRUST CLINICAL POLICIES Section 3.12 order codes and product information The nitrile lilac polyfield patient pack Contents: 1 x pair nitrile sterile gloves 7 x 7cm x 7cm gauze swabs 1 x waterproof sheet 1 x sterile field 1 x sterile apron 1 x clinical waste bag Order code : small : Code EVD055 Medium : Code EVD056 Large : Code EVD057 Smith and Nephew IV 3000 hand Contents: 1 x semi-periable cannula dressing Product specification Order code: ELW032 Codan SWAN lock needle free adaptor Contents: 1 x swan lock adaptor Order code: FSW292 Codan SWAN lock single lumen needle free adaptor Contents: 1 x swan lock single lumen adaptor Order code: FSW286 Codan SWAN lock double lumen needle free adaptor (with antireflux valves) Contents: 1 x swan lock double lumen adaptor (theatre equivilant wescott double lumen adaptor) Order code 723162 (to be purchased non stock via IPROC) BD “ stretch” disposable tourniquet 1 x Box : contents 25 items order code: FWJ009 PHT Peripheral Venous Cannulation (Adults) Policy. Issue 4. 18.09.07 Page 15 of 16 Control Date: 27/04/16 PORTSMOUTH HOSPITALS NHS TRUST CLINICAL POLICIES PHT Peripheral Venous Cannulation (Adults) Policy. Issue 4. 18.09.07 Section 3.12 Page 16 of 16 Control Date: 27/04/16