Anesthesia Chart: Documentation & Malpractice
advertisement

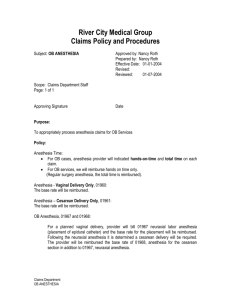
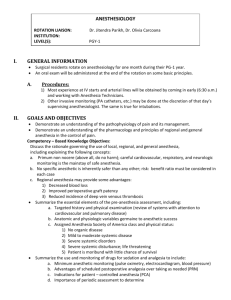
The Anesthesia Chart Marianne Cosgrove, CRNA, DNAP, APRN The Anesthesia Chart • Varies from institution to institution – May have different records within the same institution • Must all have the same basic core of info that is to be documented – Includes: • Preanesthetic evaluation/informed consent • Intraoperative anesthetic care/data • Immediate postanesthesia VS/care Basic Data • • • • • • • • • • • • Patient ID Provider information Equipment checks SOC Monitors VS (baseline and intraoperative) Line placements Medications (rationale and response where applicable) Techniques I/O (fluids, EBL, U/O) Pt. positioning and interventions Start/stop times Procedures performed The Anesthesia Chart • Records information in a sequential manner – Usually in a grid format – Allows for frequent chronological charting • Events must correlate to each other on a vertical axis – Will have 2 parts • Original for the pt’s chart • Copy for anesthesia group’s records – Utilized for QA, M & M, chart reviews The Anesthesia Chart • There may be overlap re: pt identification, time out, positioning, certain types of equipment, locals, antibiotics, etc. with the OR record • During a malpractice case, the chart will be evidence—may be expanded to poster size for the jury to see The Anesthesia Chart • 90% of medical malpractice cases are won based on the contents of the anesthesia chart • Coffee break, lunches, other provider turnovers and handoffs are the most dangerous points of any case secondary to inadequate communication Pt’s “blue plate” stamped here; note DOB and insurance codes Insurance codes: Q, M = Medicare R (rare) = Railroad Medicare D, J, Y = Medicaid (state welfare) E = City welfare N, K, B = Commercial insurance Pre-op assessment found on the back of the chart You may need to refer back to the pt’s chart to complete the note i.e. labs, etc Make sure that an attending has signed before going to the OR These sections should be completed during initial chart review before you enter the OR Start time is always on the quarter hour just before time of stamp Stamp in and correlate start times on chart Small lines = 5 mins Medium lines = 15 mins Dark lines = 1 hour 5/31 0730 ● 0730 ● 0800 ● Δ ● 0900 ● Δ ● 1000 ● Δ ● 1100 ● Δ 0800 Δ ● 0900 ● Δ ● 1000 ● Δ ● 1100 ● Δ ● 0733 Military time is preferred CRNAs and MDAs sign or cosign here SRNAs sign where CRNAs do Wait to fill in post-op diagnosis and procedure until the end of the case Both of these attributes are very important according to JCAHO and Medicare Part B Done with the anesthesia team, surgeon, and circulator in attendance preincision New charts say “patient identification” here Should be documented as given pre-incision unless surgeon requests otherwise (listed as a Medicare P4P measure) Eyes—OK to circle; put Teethchart “intact” or “as pre-op” IV/A-line— chart gauge/ location, “in situ” if applicable Note type of airway, blade size (if used), attributes of laryngoscopy, breath sounds May add “+ ETCO2” Note any difficulties in “remarks” section Note anesthetic agents here i.e. IV induction meds, narcotics, benzos, gases, muscle relaxants May add pressors like neo and ephedrine When charting meds, use qualifiers such as mg, mcg, NOT cc or ml 6 AIR sevoflurane midazolam fentanyl glyco/SCh propofol rocuronium ephedrine 2 1 1 2% 1.5 50 150 0.2/100 120 5 10 25 2 X 1 6 0.8 X 50 10 50 10 Note anesthetic agents here i.e. IV induction meds, narcotics, benzos, gases, muscle relaxants May add pressors like neo and ephedrine These are entered approximately q 15 mins ECG labels— SR, SB, SR/PVC, AF, Paced, AS TempCº FiO2, ETCO2actual values if intubated; (+), NC if MAC SaO2, BISactual values PA/CVP, C.O. actual values FluidsList type, i.e. LR, 0.9 ns, PRBC, hespan or albumin here May chart vasoactive gtts either here or in a lower “agent” row Fluidslist type and volume, i.e. LR 1000, 0.9 ns 250, PRBC, hespan or albumin here 50/50 LR 1000 #1 Hextend 500 PRBC #2 25/75 #3 +/-150 10/85 +/-400 X #1 X label totals in ml! U/O done q 1/2º; amount emptied over total amount Blood loss (EBL) entered when applicable and totaled at end VS are charted q5 min throughout the case Write in “Resp” here SV= spontaneous ventilation A=assisted 72/23; HR 129 V V ● ● ● V V V Resp SV A C Vent V C=controlled V=ventilator 161/100; HR 121 122/48; HR 80 codes used are listed on the L side of the VS area Remarks include normal and untoward events, meds administered other than anesthetic agents and ABX Chart in detail but be succinct May use “number system” or simply chart times Symbol for incision = Symbol for end of case = “Time of remarks” is utilized if using the number system to correlate remark times and to mark incision and end of case New charts have position listed here Use check boxes for pt position; expand on or further explain in the “remarks” section LLD L3-4 #22g Betadine X 3 Bupivacaine 0.5% 3 ml @1325 No heme, paresthesia Regional anesthetics charted here using check boxes; enter time, type and volume of local used under “medication” Attending anesthesiologist must sign all 3 to fulfill Medicare Part A requirements; may write in N/A for emergence if case is a MAC Totals must always be filled in at the end of the case; random spot checks done by QA committees Pg 2 of 2 Start time should correspond to the last time entered on the previous sheet 1130 1130 ● ● 1200 ● 1200 ● See pg one Δ etc… Δ etc… See pg one If the case runs longer than 4 hours, you will need to start another record Totals and post-op disposition should be entered on pg 1 New anesthesia chart— Essentially the same with the addition of 1) “transfer to PACU” box, 2 2) change of Pt ID for time out, and 3) new position area 3 1 Delineates end of the case; pt disposition (i.e. PACU, unit, etc); times and VS PLEASE STAMP OUT; time clocks in both PACUs Write in manually if you are in the unit, OTF, etc. “The White Card” It’d better be right!!! This is sent to the billing office; most important to have everything legible and correct! AANH torture chamber “Weren’t you told to write legibly on the white cards?” I wrote down the wrong diagnosis— what’d you do? Do not use the following abbreviations: • < or > • 1.0 (do not use trailing zero) • .5 (do not omit a zero before a decimal point) • U or μg (write out “units” or mcg for micrograms) • MgSO4 (write out magnesium sulfate) • Mso4 or MS (write out morphine) • cc (use ml) • These and others are found at the bottom of HSR Progress notes and on the hospital web site Major problems associated with charting • • • • • Failure to document emergence Failure to date, time and sign entries Failure to document positioning Failure to tally drugs, fluids, output Use of unapproved abbreviations (use of preprinted entries is best) • Unexplained entries (should provide a rationale as to why a medication was given if not obvious) • Illegibility • Incompleteness (errors of omission) Other problem areas associated with charting… • Mechanical ventilation • Antibiotic administration (particularly pre-incision timing) • Provider changeovers • 7 TEFRA requirements • Unexplained gaps • Inclusion of pt ID and "time outs" • Erasures, gaps, and alterations to the record (these raise inferences of errors, inattention, and falsification of data) Remember: • Write legibly; check spelling • Black ink may be mandatory in some institutions – Blue ink now thought to be OK; easily delineates the original record from a copy • Document events briefly but comprehensively • Cross out errors with a single line and write “error” next to it; add your initials • Do not go back and add to or alter the original chart – Additions may be made in the progress notes • Add up totals (meds, fluids) at the end of the case and record them • Pay attention to detail • Always use labels • Write N/A through areas that are not used • DON’T FORGET TO STAMP OUT; write in the end time if you are off of the floor (in OB, the unit, Specials, MRI, etc) EPIC is here!! • Basic concepts remain the same however: – VS will be automatically charted – Capability to go into EPIC to change VS errors 2° artifact (i.e. Bovie, transducer near floor…) • Each change is documented by the computer! • ? Setup for error in obtaining history – Template is present (basic note) which allows for 1-click history/physical! Remember: • Don’t focus on the chart/EPIC – Focus on the pt! – VS are recorded on the monitors • Go back into trends/VS when time allows • Have patience – Everyone has their own way of charting • Be flexible • Learn a bit from each person