IC-17_Colin_ Handout
advertisement

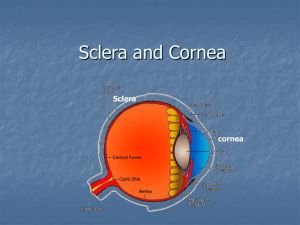
IC17: Intracorneal rings for Keratoconus and post-LASIK ectasia INTRODUCTION Keratoconus is a progressive ectatic disorder of the cornea that generally affects younger individuals. As the disease progresses, the central cornea thins and the cornea assumes a conical, rather than spherical, shape. The apex of the cone is usually decentered inferiorly. This leads to progressive myopia and astigmatism, usually irregular, leading to a loss of best spectacle-corrected visual acuity. Treatment of early keratoconus includes the use of glasses or soft contact lenses to improve visual acuity. When irregular astigmatism precludes adequate correction with glasses or soft lenses, rigid gas permeable contact lenses, which mask the surface irregularities, can often restore vision. Some patients, however, cannot be comfortably fit with a rigid lens, and as the disease progresses, the cornea may become too steep to maintain a contact lens on the eye. In addition, central corneal scarring can limit vision despite the use of any optical device. Traditionally, when patients could not get adequate vision with either glasses or contact lenses, the only surgical option has been penetrating keratoplasty (PK). Recently, new advances have added to the surgical options for keratoconus. In addition, they also can be applied to two closely related diseases, pellucid marginal degeneration and post-LASIK ectasia. Intracorneal ring segments can improve uncorrected and best corrected visual acuity, or allow for successful contact lens fitting in a previously unfittable patient, avoiding the need for keratoplasty. Collagen cross linking (CXL) can increase the biomechanical rigidity of the cornea, flatten the cornea, and prevent progression of the disease. While laser remodeling of the cornea would threaten to worsen the disease in an untreated cornea, it might be successfully and safely performed in a cross-linked cornea. PK has generally been a very successful technique for restoring vision in patients with advanced disease. Graft rejections, however, are common, and threaten graft survival. Recent advances in lamellar surgery techniques that enable near-equivalent visual outcomes to PK have made deep anterior lamellar keratoplasty (DALK) a viable option to PK, sparing the risk of endothelial graft rejection. INTRACORNEAL RING SEGMENTS Intracorneal rings affect the keratoconic cornea in two ways. First, the ring effectively adds tissue and elevates the anterior surface of the cornea overlying the ring. Since the central cornea flattens in the direction of an elevated area, the 360o placement of the ring causes a generalized flattening of the central cornea, reducing the amount of myopia. The flattening effect of the ring segments is proportional to the thickness of the ring, and inversely proportional to the diameter of the ring segments. Asymmetric placement of rings of different thicknesses can reduce astigmatism and centralize an eccentric cone. Secondly, in keratoconus, the corneal elastic modulus is reduced due to pathology in the corneal stroma. This causes the cornea to be more deformable in response to stress, leading to thinning and protrusion (increased curvature), which are the hallmarks of keratoconus. By shortening the path length of the collagen lamellae central to the segments, there is a redistribution of corneal stress, interrupting the biomechanical cycle of keratoconus disease progression and in some cases, reversing the process. The goal of ring segment surgery is to reduce the degree of myopia and astigmatism, improving uncorrected and best corrected visual acuity. Shifting the position of the cone more centrally within the cornea may also improve higher order aberrations, such as coma. Unlike purely refractive procedures, however, the goal is not emmetropia; rather, a successful prodecure is one that improves vision enough that the patient can be comfortably corrected to an adequate level of vision with spectacles or contact lenses, avoiding riskier procedures such as keratoplasty. Intacs Ring Segments While there are a variety of intracorneal rings used worldwide, including the Keraring, and the Ferrara Ring Segment, the most widely used, and only ring segment used in the U.S., is the Intacs® Ring Segment (Addition Technology Inc, Sunnyvale, California). The Intacs segments consist of a pair of PMMA semicircular pieces, each having an arc length of 150o and a hexagonal cross-sectional shape. When implanted surgically, the Intacs rings have an external diameter of 8.10 mm and an internal diameter of 6.77 mm. The refractive effect is determined by the ring thickness. In the U.S., the FDA-approved rings are available in sizes ranging from 0.21 mm to 4.5 mm. Current designs have a predicted myopic range of correction from -1.00 D to -4.10 D. Recently a new Intacs design (Intacs SK®) with an inner diameter of 6 mm and an oval cross-sectional shape has been introduced. Indications Intacs can be used in patients with keratoconus, pellucid marginal degeneration, and post-LASIK ectasia who are not adequately and comfortably corrected with gas-permeable rigid contact lenses. They should not be used in patients with significant central corneal scarring. They should also not be used in patients with untreated atopic disease or evidence of local or systemic infection. While there are no absolute guidelines for the maximum corneal steepness to be treated with Intacs, some surgeons in the US have suggested 58D as an upper limit. Surgical Technique Intacs procedures are generally performed using topical anesthesia. Surgery is performed around the geometric center of the cornea, which is marked with ink. The incision axis is determined, and, using a specially designed marker, the incision site and location of the rings is delineated. In the US, the steep axis technique (placing the incision at the topographic steep axis of the cornea) is the most popular, but a temporal incision can also be used. After measuring the corneal thickness at the incision site (minimum cornea thickness is 480µ), a guarded diamond knife is used to make the incision at approximately 70% cornea depth. After initiating a stromal channel at the base of the incision, a complete circular stromal channel is created with a stromal spreader. The Intacs segments are then inserted. The choice of Intacs segments, and whether done symmetrically or with different sized segments, is based on mean refractive error, amount of astigmatism, and location of the cone. After correct placement of the Intacs segments, the incision is closed with tight 10-0 nylon sutures with the knots buried. Patients are treated with antibiotic and steroid eyedrops and oral analgesics. The incision and stromal tracks can also be created with most of the different femtosecond lasers currently on the market .With this technology , it is very simple to select the inner and outer diameter of the channel dissection , its depth and to perform the radial incision on the selected axis in less than 15 seconds .Great care should be taken to the centration of the procedure because of the frequent shift of the central cornea due to the applanation of the laser . Results Several studies have reported the results of the implantation of intracorneal rings for keratoconus , pellucid marginal degeneration and post-LASIK ectasia . Using the mechanical dissection method, Colin et al reported that 78% of eyes gained uncorrected visual acuity (UCVA) with improvement in the mean refractive spherical equivalent (MRSE) and mean keratometry (K) value of 3.1 ± 2.5 D and 4.3 ± 2.8 D , respectively. Alio et al. found that best corrected visual acuity (BCVA) improved from 20/50 to 20/30 and remained constant at 36 and 48 months, and MRSE improved from -5.40 D to -3.95 D . Although they found fluctuation in K-values, refraction remained constant at 36 and 48 months. Complications Implantation of intracorneal ring segments is generally a very safe surgical procedure. Most significant intraoperative complications occur while dissecting the channel for the rings. These can include creating too shallow a channel or uneven channel depth, anterior or posterior perforations, and decentration of the channels. These complications might be avoided with the use of the femtosecond laser to create the channels. Postoperatively, infections are rare but do occur. In addition, sutures can loosen and lead to secondary infection. Segments can migrate, especially if patients rub their eyes, leading to unwanted optical effects. Overlapping segments can cause pressure necrosis of the cornea and corneal ulceration. In the event the ring segments cause significant unwanted effects, they are easily removed with the cornea reverting to very near the pre-operative topography. One advantage of ring segment surgery is that the central cornea is not violated. Later keratoplasty can be performed, either after ring segment removal, or around the ring segments. COMBINED COLLAGEN CROSS LINKING AND INTRASTROMAL RINGS CXL and intracorneal rings have complementary effects on the corneal biomechanics and refractive parameters. CXL has its effect mainly on the anterior cornea, and intracorneal ring segments provide flattening effects and redistribution of stress on deeper layers Sequential or simultaneous treatment with both ICRs and CXL appears to have an additive effect over either procedure alone. Combined treatment results in greater improvement of UCVA and BCVA, more reduction of myopia and astigmatism, and a greater than two fold reduction of mean and steepest keratometry readings. Postulated explanations for the additional effects include: 1) a simple addition of the effect of the two procedures, 2) coupling from cross-linking of collagen around the ring segments, and 3) greater effect of crosslinking due to pooling and concentration of riboflavin in the channel around the ring segments.