ptosis
advertisement

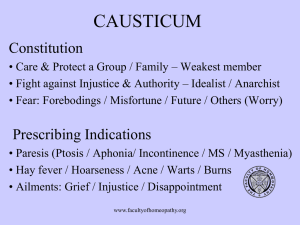
Lip Teh December 2005 BLEPHAROPTOSIS History of the Procedure: Treatment of ptosis dates back well before 200 years. Until the early 1800s, management was limited to simple excision of skin from the upper lid. Von Graefe- resected a strip of orbicularis muscle with the skin excision. Bowman (1859) described a transconjunctival resection of the levator. Fansella and Servat (1961) reported resection and plication of the conjunctiva, tarsus, and levator to address mild ptosis with good levator function. Beard (1969) proposed a modification that used a continuous running suture rather than interrupted horizontal sutures. The use of fascial slings to suspend the upper lid from the frontalis muscle was originated by Payer (1928) and Lexer (1923) and later adapted by Risdon (1945). Tillett and Tillett (1966) and McCord and Shore (1982) suspended the ptotic lid in a similar fashion but employed silastic strips rather than fascia. Anterior approaches to the levator using a blepharoplasty-type incision allow resection of a portion of the levator aponeurosis and tightening. Further evolution has led to techniques that use adjustable suture plication either alone or in conjunction with aesthetic blepharoplasty. Classification 40-50% acquired cases are involutional (myopathic) and 30% post-traumatic PSEUDOPTOSIS Causes: 1. Insufficient posterior support of eyelid – enopthalmos, micropthalmos, enucleation 2. Vertical muscle imbalance – ptosis on the side of hypotropic non-fixating eye 3. Brow ptosis (excess skin brow) 4. Dermatochalasis (excess skin eyelid) 5. Contralateral lid retraction CONGENITAL 70% unilateral Causes: 1. Congenital myogenic ptosis main cause of congenital ptosis anomalous levator – a localized myogenic dysgenesis. fibrous and fatty infiltration in the muscle belly, diminishing the ability of the levator to contract and relax. In downgaze, ptotic lid sits higher as lid cannot relax. Lagophthalmos in down gaze is a sign of congenital ptosis. Lip Teh December 2005 Affected children show a high incidence of coexistent strabismus, amblyopia, and anisometropia. Usually idiopathic, rarely inherited as Blepharophimosis (BPES) syndrome: Consists of 1. blepharophimosis - short palpebral fissures (horizontal) 2. congenital ptosis 3. epicanthus inversus (skin fold from lower lid) 4. telecanthus with normal interpupullary distance Treatment o Early (age weeks-month), Indicated for 1. Amblyopia from visual axis occlusion (unilateral ptosis) 2. Developing chin-up head posture 3. Induced astigmatism – eyelid pressure on cornea changes its shape o Late – indication: cosmetic - most agree should be done around age 5 or before begins regular school 1. Severe ptosis(<5mm excursion) – frontalis sling 2. Moderate – levator muscle resection a. levator function 5mm - levator resection of greater than or equal to 22 mm is recommended. b. 6-8 mm, a levator resection of 16-18 mm c. >8 mm, a levator resection of 10-13 mm 3. Mild – conservative or Fasanella Servat procedure (excises the tarsus, conjunctiva, Müller muscle, and perhaps levator tendon) 2. Neurogenic anomalies a. Marcus Gunn jaw-winking syndrome Usually unilateral ptosis at rest. Wink phenomenon may be elicited by opening the mouth, thrusting the jaw to the contralateral side, jaw protrusion, chewing, or sucking. It often is discovered early, as the infant is bottlefeeding or breastfeeding Due to aberrant connection between superior division of CN III and motor branch of CN V. momentary upper eyelid retraction with stimulation of ipsilateral lateral pterygoid rarely involve medial pterygoid synkinesis. Treatment: Address deprivational amblyopia early. Before treating ptosis, associated strabismus should be addressed. If jaw winking significant, then ablation of the levator and resuspension of the eyelid to the brow are necessary. For symmetry, may need to do the same operation on the other (normal) side. Others suture the divided levator to the arcus marginalis to allow for reversal at a later date b. Horner’s syndrome May be associated with brachial plexus palsy Mild ptosis, miosis, and anhidrosis. Ipsilateral lower eyelid may be elevated. Lip Teh December 2005 Heterochromia may develop due to the lack of sympathetic innervation to the iris melanocyte development 3. Mechanical a. Congenital periorbital tumors - Plexiform neuromas, lymphomas, leukemias, rhabdomyosarcomas, neuromas, neurofibromas ACQUIRED 1. Neurogenic a. 3rd CN palsy (down and out gaze) b. Horner's syndrome i. mullerectomy (Putterman procedure) ii. levator aponeurosis reinsertion iii. Fasanella-Servat procedure c. Third nerve misdirection (usually following trauma) – levator excision and sling d. Multiple sclerosis Usually requires frontalis sling 2. Myogenic a. Myasthenia gravis acquired autoimmune disorder (B cell) characterized clinically by weakness of skeletal muscles and fatigability on exertion. Antibodies against acetylcholine receptor on postsynaptic membrane 50% present with eye signs, usually ptosis – usually asymmetric Diagnosis: 1. fatigue test – open/close several times 2. Simpson test – gaze upwards for an extended time 3. Lid twitch sign – look down for 10s and quickly to primary gaze. Will see upward overshoot of the lid with several twitches, followed by repositioning of the lid to the original ptotic state. 4. pharmacological – Tensilon (edrophonium – a short-acting AChE inhibitor) – 10mg IV (beware cardio-resp side effects) 5. Ice pack test - applied to the affected eyelid for about two minutes and ptosis improves since neuromuscular transmission improves at lower temperatures. Also improves after sleep (sleep test) 6. blood - anti-AChR antibody, Antistriated muscle (anti-SM) Ab, TFTs 7. EMG - single-fiber electromyography and repetitive nerve stimulation 8. CT/CXR – for thymoma (20%) Treatment: medical, with surgery reserved for stable ptosis, which has failed to respond to medical therapy for MG. Techniques include external levator advancement, frontalis suspension sling, or tarsomyectomy. Complications include worsened diplopia and exposure keratopathy b. Chronic progressive opthalmoplegia – young male, initially can’t move eyes then develops ptosis c. Myotonic dystrophy Lip Teh December 2005 d. botox injection for corrugators – avoid by injecting 0.1 to 0.2 cc of Botox (2.5 to 5 units) immediately above the eyebrow, 2 cm from the midline. e. Treat underlying disease first, then consider levator plication/resection 3. Mechanical a. Eyelid, orbital tumor b. Cysts – chalazion c. Ptotic lacrimal gland Treat mass and combine with blepharoplasty and levator reinsertion if aponeurosis stretched 4. Traumatic a. accidental injury b. iatrogenic c. Scarring May be due to levator damage (myogenic), nerve damage or mechanical (scarring) Treatment: i. if neurogenic, often best to wait 6-12months for some recovery as often also involves superior rectus palsy (same superior division nerve supply). Early correction may lead to lagopthalmos in the presence of absent/weak Bells phenomenon. ii. if has levator function, then reinsert to the tarsal plate. Otherwise sling. 5. Aponeurotic (disinsertion, dehiscence, attenuation of insertion) a. Involutional (age-related/senile) b. Complete dehiscence is rare, usually attenuated c. Post pregnancy (oedema) Clinically: good levator function, high or absent supratarsal crease, thin lid skin, slow inversion of the lid following manual eversion, and increased ptosis on downward gaze. Treatment: Levator reinsertion Hering’s Law of equal innervation 1) Originally described for extraocular muscles but applies for levator and frontalis 2) The 2 sides are supplied from a single central caudal subnucleus of the oculomotor complex, 3) Help predict whether the repair of unilateral ptosis may lead to increased ptosis, or unmasking of ptosis, on the contralateral side 4) A patient's attempt to overcome ptosis in one eye will induce an increased innervation in both levators, with resulting contralateral lid retraction. Lip Teh December 2005 5) This retraction may not always be noticeable because of synchronous disinhibition of the orbicularis oculi, sympathetic inhibition of Mueller's muscle, or coexisting mild ptosis in the other eye. 6) Hering's test (enhanced ptosis). Immobilise the eyebrow with a finger while the more ptotic eyelid is retracted to a normal position with a finger or a cotton swab for at least 5s. May also be unmasked by paralyzing Mullers with phenylephrine 7) A positive test is when ptosis develops in the contralateral eye 8) Recommend repair of both eyelids when any degree of ptosis is detected on the least ptotic side with Hering's test Procedures Operation Conjuctivomullerectomy (Putterman) Fasanella-Servat Aponeurosis Reinsertion Aponeurosis Plication Levator resection/advancement Frontalis sling Or Frontalis muscle flap Indication Mild ptosis with normal levator excursion Positive response to phenylephrine test Mild ptosis with good levator function Horner’s syndrome Mild to moderate ptosis with levator function Senile ptosis Traumatic disruption Mild ptosis Generally better to do levator advancement Ptosis with at least moderate levator function Congenital ptosis Poor or absent levator function Neurogenic ptosis Congenital ptosis Non Surgical option Crutch glasses May be considered in cases in which the patient refuses surgery or is at a very high operative risk because of concomitant disease. Also in geographic regions where medical and surgical facilities are not readily available. Lip Teh December 2005 Müller's Muscle Conjunctival Resection (without tarsal excision) Reserved for patients with minimal ptosis (2 mm or less) with normal levator excursion and a positive phenylephrine test. When Müller's muscle is advanced, it strengthens the posterior lamella and appears to plicate the levator aponeurosis with healing and subsequent scarring in the posterior lamella Use LA with no adrenaline (will stimulate Mullers) Resection marked on conjuctival surface Using 3 traction sutures placed through the conjunctiva and Müller's muscle to elevate the required amount of conjunctiva and Müller's muscle to be resected. A clamp is applied and the clamped tissues resected. FasaneIla-Servat Procedure (with tarsal excision) reserved for patients with minimal ptosis, intact levator and a negative phenylephrine test who do not require blepharoplasty Anterior approach is known as the Mustarde procedure – more invasive Correction of more than 2mm of ptosis is not recommended because of the need to excise large amounts of tarsus Involves resection of tarsus, conjunctiva and Muller’s muscle. One millimeter of tarsus should be resected for each millimeter of ptosis. Lip Teh December 2005 The tissues are elevated via the two traction sutures and the clamp is placed over the tarsus and conjunctiva Useful even in patients with Horners syndrome Complications include undercorrection, overcorrection, and rarely, corneal epithelial defect. Overcorrections can usually be treated by early removal of the suture and by digital massage. Undercorrections will need a levator aponeurotic repair. Aponeurosis Reinsertion For moderate ptosis especially when concomitant blepharoplasty is desired. LA preferred o allows documentation of levator function at the time of surgery o allows the patient to cooperate with the surgeon in setting the proper height and contour of the lid o subcutaneous injection 1ml 2% lignocaine. Avoid injecting deep to septum as this will paralyse the levator. May need to overcorrect by 1mm Anterior approach If fully dehisced, the levator rolls superiorly thus Mullers muscle is encountered first after going thru orbicularis. Identify Mullers by its red color and a large marginal vessel overlying the retrotarsal margin. Need to dissect superiorly to look for levator. Resuture the tendon to the upper mid portion of the tarsus, but slightly nasal to the pupil in the primary position, using a nonabsorbable suture. Can be further augmented by excising additional amounts of tarsus to elevate the eyelid margin. Generally aim for 1 to 1.5 mm overcorrection as orbicularis is paralyzed by local anesthetic Generally no Frost suture required Aponeurotic Plication Mild ptosis, good levator function where concomitant bleph required does not require the patient to be awake or upright (GA as part of cosmetic procedure) Anterior approach Plicate only the aponeurosis, 6/0 clear nylon - superior portion of the suture is placed in the aponeurosis 4 to 8 mm above the superior tarsus, depending on the severity of the ptosis. The inferior portion of suture is placed in the aponeurosis just above the tarsal plate. Levator Resection/Advancement For >4mm levator function LA preferred anterior approach resect the desired amount of skin orbital septum opened identify transverse ligament of Whitnall (don’t suture this to tarsus otherwise will not fix ptosis) dissect Mullers muscle off levator. In milder cases, dissect to origin of Mullers. In severe cases, the origin of Mullers should be divided from levator and resutured later. Lip Teh December 2005 Whitnalls ligament may need to be divided as it acts as a check ligament on the levator Temporarily tie horizontal mattress sutures to the antero-inferior 1/3rd of tarsus and to the levator . Adjust the amount of lift required and only then resect. Generally 1:4 ratio ie 3mm ptosis needs 12mm advancement Frost suture required for lagopthalmos Fascial Slings/Suspension Indicated for severe ptosis with poor levator function (<5cm) Caution in patients with poor Bell's phenomenon, decreased tear production with a history of dry eyes, and limited ocular motility- at increased risk for complications following frontalis suspension techniques due to lagophthalmos and corneal exposure. Disadvantage: o Preseptal placement – so vector is upwards rather than upwards and inwards o Depend on the structural durability and permanency in position of the implanted material for the longevity of results. Will cause cosmetic blemish on downward gaze because the motion of the lid is restricted Options: 1) autologous fascia lata, tendon graft o must be at least 3 years of age (height >100cm) to have adequate leg length to provide suitable fascia lata o resoption contribute to long term failure o deep temporal fascia is another option 2) allograft - preserved fascia lata, umbilical vein o higher rate of resorption – 28% risk of recurrence 3) alloplastic most commonly used are silicone rods, Gore-Tex and mersilene mesh. Also catgut, collagen, Prolene, stainless steel, silk, Supramid and tantalum. complication – granulomas, infection, failure due to absorption, stretching, fracture, or cheese wiring. Indications: postop adjustment is desirable (dry eyes) where recovery is expected o placed as a double rhomboid, single rhomboid, or triangular sling from the frontalis to the lid produces the best result. Stab incisions crease incision o Lower stab incisions are placed in line with medial and lateral limbus Multiple designs described o Pentagonal most common (Crawford 1971) o Either place over tarsus or suture directly to tarsus o Passed thru preaponeurotic space, under orbicularis and attached above brow to frontalis muscle (deep surface). Some pass it deep to Whitnalls ligament (Pearl PRS 2001) Whitnall’s sling procedure o Whitnall’s ligament is sutured to the superior portion of the tarsal plate. o Advantages: can be used as a unilateral procedure Lip Teh December 2005 preserves the muscular elevating structures of the eyelid is an anatomic procedure with some dynamic eyelid function produces an esthetically pleasing eyelid crease Pentagonal and double pentagonal Frost suture recommended. Lagopthalmos common post op and eye drops required until this settles. Frontalis Flap From Park PRS 1998 The thick line indicates the superiorly based muscle flaps. Lip Teh December 2005 (Above, left) The superiorly based orbicularis oculi muscle flap. (Above, right) The superiorly based U-shaped orbicularis oculi muscle flap with interdigitated portion of the orbicularis oculi-frontalis muscle at the eyebrow region (Below, left) The U-shaped superiorly based frontalis muscle flap with interdigitated portion of the orbicularis oculifrontalis muscle at the eyebrow region (Below, right) the L-shaped superiorly based frontalis muscle flap o GA for small children, preference in adult is to perform the operation with the patient under light intravenous sedation and local anesthesia Superiorly based orbicularis oculi muscle flap Biplanar dissection raising the orbicularis flap muscle flap is sutured to the anterior surface of the tarsus with three permanent 5-0 silk sutures through the central, medial, and lateral portions of the muscle flap and the tarsus. High risk of recurrence (Park PRS 2005) Superiorly based frontalis flap Described by Song 1982 Blepharoplasty and suprabrow incision Divide interdigitating fibres between frontalis and orbicularis L-shaped frontalis flap with a caudal limb of 2 to 2.5 cm (at the level of the eyebrow) and a vertical limb of 2.5 to 3.5 cm along this medial margin Transposed to suture to tarsus To create a better vector Ramirez (PRS 2004) creates a semirigid pulley based on the orbital septum by detaching it from its bony supraorbital origin for 2.5cm, through which the frontalis muscle is passed to run behind and under the orbital septum to reach the plane of the levator system. Initially he performed through a bleph and suprabrow incision, later – just bleph incision He also did a levator resection/advancement or attaches it to the posterior surface of the frontalis flap. If the levator is fibrotic and inelastic, it is better to ignore it; otherwise, lagophthalmus will result postoperatively. Lip Teh December 2005 (Left) Sagittal diagram of normal anatomy. (Right) Frontalis muscle advancement to the orbital eyelid area. 1, Frontalis muscle; 2, orbicularis oculi muscle; 3, septum orbitale; 4, levator aponeurosis; 5, Müller's muscle. Summary Levator function >8mm o Putterman conjunctivomullerectory with active Mullers o Fansanella Servat if mild ptosis with inactive Mullers o Levator reinsertion for dehiscence Levator function 5-8 o Levator resection and advancement 4:1 ratio Levator function <5mm o Frontalis slings or Frontalis flaps Complications 1. Undercorrection The most common complication Due to poor planning ( wrong operation or under resection) or excessive hemorrhage and the resultant scarring Treatment – if early , readjust sutures, otherwise perform another ptosis operation. 2. Overcorrection Lip Teh December 2005 Overcorrection in moderate or severe congenital ptosis is rare - very difficult to produce by any reasonable amount of levator resection. However easy to occur if perform levator resection for involutional ptosis. Due usually to lid being unintentionally sutured to the Whitnall ligament or to an excessively shortened orbital septum Treatment: o Massage, stretching o Undo sutures if early o Levator recession is required if persists – usually no spacers required but if so, preserved sclera and fascia lata have been used to lengthen the levator muscle (amount of recession is equal to the amount of lid retraction) 3. Poor or improperly positioned lid crease If too high, then reexcise If too low, difficult to treat. Best option may be to lower the contralateral side 4. Lid peaking Uneven placement of sutures in tarsus or uneven tarsal resection 5. Lagopthalmos Exposure keratitis frequently noted for the first few weeks after surgery, usually resolves treat with temporary tear replacement, ointments, and lid closure at night. If persists, consider temporary punctual plugs 6. Corneal abrasion Inadequate globe protection (eye shields recommended) or from suture irritation 7. Lid Lag 8. Hematoma 9. Chemosis Treatment with steroid eye drops and stop other types of drops 10. Asymmetry 11. Blindness – retrobulbar hemorrhage or traction on postseptal fat 12. Diplopia due to direct damage to the superior rectus muscle and sometimes the superior oblique muscle; rarely, it is due to direct nerve damage.