PREOPERATIVE DIAGNOSIS:
advertisement

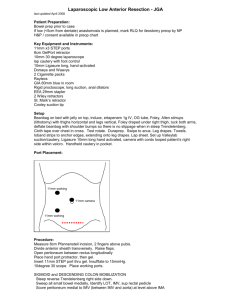
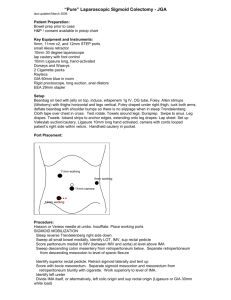
PREOPERATIVE DIAGNOSIS: Rectal cancer. POSTOPERATIVE DIAGNOSIS: Rectal cancer. OPERATION: Laparoscopic-assisted low anterior resection with a colorectal anastomosis and loop ileostomy; takedown of the splenic flexure. ANESTHESIA: General anesthesia. CLINICAL INDICATIONS: The patient is a 41-year-old lady with a history of rectal cancer that was staged with endorectal ultrasound and CT scan of the abdomen and pelvis. The tumor was considered to be a stage 3 disease. She was advised to undergo preoperative chemoradiation therapy. She then came for radical proctectomy with total mesorectal excision. The indications for the procedure as well as the potential risks and complications were discussed with the patient. She agreed to proceed with the surgery and signed appropriate consent. DESCRIPTION OF PROCEDURE: The operation was performed with the patient under general anesthesia in the modified lithotomy position with the legs in Allen stirrups. Pneumatic boots were used for deep venous thrombosis prophylaxis. A gram of Cefoxitin was used for antibiotic prophylaxis. The abdomen was prepared with Betadine and draped sterilely. We started the operation by making an incision lateral to the umbilicus. A Hassan trocar was inserted and a pneumoperitoneum was created. We then inserted 10 additional trocars in the right lower quadrant, at the site that had been previously marked for the ileostomy, and the left upper and right upper quadrants. We started the operation by placing the patient in Trendelenburg with the right side down, and removing the small bowel from the pelvis. Then the root of the mesentery of the sigmoid colon was identified. A small incision was made underneath the superior rectal vessels. These were skeletonized all the way to the region of the inferior mesenteric artery. The left ureter was identified. The mesentery of the sigmoid and descending colon was lifted from their retroperitoneal attachments. Eventually, the inferior mesenteric vessels were divided with a fire of the endo-GIA stapler. We continued lifting the mesentery of the descending colon from the retroperitoneal attachments. The inferior mesenteric vein was then dissected and divided with the LigaSure. We continued dissecting the mesentery of the descending colon and the splenic flexure from the retroperitoneal attachments, pushing down the left ureter and left gonadal vessels. Then we moved laterally to the attachments of the sigmoid colon to the line of Toldt. The peritoneum was opened in this area and the left colon was that way completely lifted from the retroperitoneal attachments. We continued mobilizing the left colon all the way to the splenic flexure. The LigaSure was used to take down the splenic flexure all the way to the mid-transverse colon. Once the left colon was totally mobilized, we made a suprapubic incision. The skin was opened with the scalpel and the incision was carried through the subcutaneous tissue until we reached the anterior rectus sheath. This was opened with the electrocautery unit, exposing the rectus muscles. The medial aspect of both rectus muscles was divided with the electrocautery unit, preserving the inferior epigastric vessels. We used the medium size Alexis retractor for exposure. We packed the small bowel in the upper part of the abdomen and exteriorized junction of the sigmoid and descending colon. The bowel was skeletonized and divided with a fire of the GIA stapler. The marginal vessels were divided with the LigaSure. The proximal portion of the colon was returned to the abdominal cavity and we continued dissecting the rectum, entering the areolar space behind the fascia propria of the rectum at the level of the promontory. The peritoneum on both sides of the rectum was divided with the electrocautery unit and we continued dissecting the areolar space behind the fascia propria of the rectum and the presacral space. This plane was dissected all the way down to the Waldeyer fascia. Laterally, the lateral stalks were divided with the electrocautery unit, taking care to preserve the hypogastric plexuses and the pelvic plexuses. Anteriorly, the peritoneum in the cul-de-sac was opened and the dissection was carried immediately posterior to the posterior wall of the vagina. Posteriorly, the dissection was carried all the way down to the pelvic floor and laterally. The levator muscles were identified. Anteriorly, we carried out our dissection until we reached the lower portion of the rectovaginal septum. At this point, I performed a proctoscopic examination to visualize the tumor because it was difficult to palpate through the rectal wall. It had been reduced to an ulcer that was located in the anterior wall of the rectum and was already way above the area that had been dissected. For that reason, we used the TA stapler to staple the rectum a couple of cm above the levators. We used the TA-30 with green staples. The rectum was then transected proximal to the staple line. The specimen was sent to Pathology for inspection. They opened it and __________. The distal margin was at least 3 or 4 cm. The circumferential margins appeared negative. We then turned our attention to the closed end of the descending colon. We had enough length to perform the anastomosis without any degree of tension. The staple line at the divided end of the colon was removed and the anvil of the 31 CEEA stapler was inserted into the colon. The spike of the anvil was brought through a small counterincision in the antimesenteric portion of the colon, approximately 8 cm from the end. A small pursestring was placed around the spike of the anvil. Then the open end of the colon was closed with another fire of the TA stapler. We then inserted the main portion of the stapler into the short rectal cuff. My assistant, Dr. Elizabeth Wick, advanced a spike of the main portion of the stapler through the rectal wall at the level of the transverse staple line. I then removed the spike and inserted the anvil in the main portion of the stapler. She closed the instrument, performing a side-to-end colorectal anastomosis while I kept the orientation of the bowel. The anastomotic rings were intact. We then checked the integrity of the anastomosis by performing a proctoscopic exam and insufflated air while the pelvis was filled with water. No air leaks were identified. There was no bleeding at the level of the anastomosis. A 10 flat French Jackson-Pratt drain was left in the pelvis and brought through a counterincision in the left lower quadrant. We then chose a loop of small bowel, approximately 20 cm from the ileocecal valve to perform a loop ileostomy. An opening that was created in the right lower quadrant for the 12 mm trocar was then enlarged, and a disc of skin was removed. The opening in the anterior rectus sheath and the muscle was enlarged, and the ileum was brought out through this incision. The umbilical incision used for the Hassan trocar was closed with 2-0 Dexon stitches. Then the skin in the umbilical trocar site and right upper quadrant trocar site was closed with a subcuticular 4-0 Biosyn and Indermil. The peritoneum in the suprapubic incision was closed with running Maxon. The wound was irrigated with saline and the anterior rectus sheath was closed with #1 Maxon. The Waldeyer fascia was approximated with interrupted 4-0 Dexon stitches and the skin was closed with a subcuticular 4-0 Biosyn and Indermil. The ileostomy was then matured in a Brooke fashion with interrupted 4-0 Dexon stitches. ESTIMATED BLOOD LOSS: Less than 100 mL. COUNTS: two. Sponge and instrument counts were correct times DISPOSITION: The patient tolerated the procedure well and was transferred to the Post-Anesthesia Care Unit in a stable condition. ASSISTANT SURGEON(S): Elizabeth Wick, M.D. If the assistant surgeon is other than a qualified resident, I certify that the services were medically necessary and there was no qualified resident available to perform the services.