Low Ant Resection
advertisement
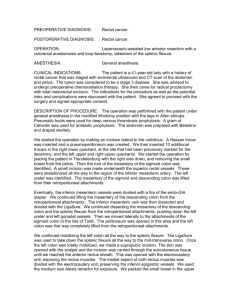
PREOPERATIVE DIAGNOSIS: Rectal cancer. POSTOPERATIVE DIAGNOSIS: Rectal cancer. OPERATION: Intraoperative ultrasound, low anterior resection with low colorectal anastomosis, diverting loop ileostomy, proctoscopy. ANESTHESIA: General anesthesia. CLINICAL INDICATIONS: The patient is a 57-year-old gentleman diagnosed with rectal cancer with possible liver metastases that has been treated with neoadjuvant chemoradiation therapy. He has been advised to undergo total mesorectal excision with a primary anastomosis. We discussed the rationale for the surgery as well as the potential risks and complications including the possibility of an anastomotic leak. We advised him to have a loop ileostomy that he accepted. We also decided to do an intraoperative liver ultrasound to better define potential lesions in the liver. Dr. Stanley Rogers performed a portion of the procedure and will dictate that as a separate operative report. PROCEDURE: The operation was performed with the patient under general anesthesia in a modified lithotomy position with the legs in Allen stirrups. We used a beanbag. Pneumo boots were used for deep venous thrombosis prophylaxis. A gram of cefoxitin was used for antibiotic prophylaxis. The abdomen was prepped with Betadine and draped sterilely. We started the operation by introducing the Veress needle through a small incision in the umbilicus. This helped to create a pneumoperitoneum. Then, Veress step 11-mm trocar was placed in the supraumbilical incision. Additional trocars were placed in the right lower quadrant and in the right upper quadrant. With the help of this trocar, Dr. Stanley Rogers performed an intraoperative liver ultrasound. He found 2 lesions in segments 5 and 7 of the liver. He will dictate this in a separate operative report. Then we made a small suprapubic incision that was carried through subcutaneous tissue until we reached the anterior rectus sheath. The sheath of the rectus muscle was split transversely. Flaps were raised in the upper and lower portions of the incision below the anterior rectus sheath. The rectus muscles were split in the midline, and the peritoneum was then entered. The GelPort device was then placed, and pneumoperitoneum was created again. We then identified the superior rectal vessels. They were skeletonized. The ureter was seen underneath the opening that was created posterior to the superior rectal vessels. This was kept out of harm's way. The superior rectal vessels were then divided with the LigaSure. The left colic vessels were preserved. His sigmoid colon was quite redundant. We started lifting the mesentery of the sigmoid colon from the retroperitoneum using blunt dissection. The gonadal vessels were placed posteriorly. The mesentery of the descending and sigmoid colon was completely lifted from the retroperitoneal attachments all of the way to the splenic flexure. We then started taking down the attachments of the sigmoid colon from the parietal peritoneum along the line of Toldt. These were taken down using Metzenbaum scissors until we connected with the plane of dissection that had been developed medially. The attachments of the entire descending colon all of the way out to the splenic flexure were taken down. At this point, we felt that we had mobilized enough of the colon to do a low colorectal anastomosis. For that reason, we removed the pneumoperitoneum, and through the low-transverse incision with an Alexis retractor we were able to able to exteriorize the colon. We divided the colon in the midtransverse and continued dividing the mesentery with the LigaSure toward the root of the mesentery. At this level where the superior rectal vessel had been already divided, all we had to do was divide the avascular portion of the mesentery. The upper portion of the colon was then packed in the abdomen along with the small bowel and the cecum. Then, we started dissection of the rectum by developing the areolar space behind the fascia propria of the rectum. The hypogastric nerves were identified and preserved. The dissection was carried distally as far as Waldeyer fascia. The peritoneum on both sides of the rectum was then opened with the electrocautery unit until we reached the lateral stalks. They were similarly divided with the electrocautery unit. Anteriorly, the plane between the rectum and the Denonvilliers fascia was developed. We stayed in this plane because the tumor was clearly located posteriorly. We continued dividing the attachments anteriorly between Denonvilliers fascia and the mesorectum as far as it was feasible. Laterally, the lateral stalks were divided all of the way to the levators. While the rectum had been fully mobilized to the pelvic floor, we used a TA-30 stapler to staple the rectum and transect it at the level of the pelvic floor. The specimen was checked by Pathology, who found an ulcerative lesion several centimeters from the distal end. At this point, we turned our attention to dividing the end of the descending colon. It was quite healthy, having good vascular supply, and we reached the floor of the pelvis without any difficulty. For that reason, we placed a pursestring and divided the end of the colon. The anvil was placed in the divided end of the colon, and the pursestring was tied around the smallest half of the anvil. Then, my assistant, Dr. Kim Rhoads, went to the perineum and inserted the main portion of the stapler into the short rectal cuff. Under my guidance, she had planned to spike through a transverse staple line. I then divided the spike and inserted the anvil in the main portion of the stapler. She closed the instrument while I kept the orientation to prevent any twisting or rotation. She fired the instrument, completing the colorectal anastomosis. Unfortunately, the anvil then became detached, and it would not come out through the anus. We felt that probably it was trapped by some staple from the transverse staple line in the rectal stump. I went to the perineum, and I inspected the area. I found that what had happened was that the cutter had not cut the colon. For that reason, I used a Lone Star retractor to expose the anus. This way, I was able to see the anvil very clearly. The tissue on the colon side of the anastomosis had not been divided by the stapler. For that reason, I divided it inside the staple line using the electrocautery unit. These released the doughnuts that were sent to Pathology. I then performed a proctoscopic exam that revealed an intact anastomosis. We performed an air-leak test that revealed no bubbling. Dr. Rhoads performed this again after I had changed gown and gloves and was in the abdomen. There was no air leak whatsoever, and the anastomosis was intact. We then changed gowns and gloves and proceeded to create the loop ileostomy. An opening was made in the right side of the abdomen at the site that had been previously marked by our stoma therapist. The loop of bowel was brought through this incision and kept oriented by passing a glove through the mesentery. The midline incision was then closed by approximating the peritoneum with running 2-0 Dexon. The anterior rectus sheath was approximated with running #1 Maxon. The subcutaneous tissue was irrigated with saline, and the skin was approximated with staples. The infraumbilical small incision used for the camera was closed with 2-0 Dexon stitch. The right lower quadrant trocar site was used to place a drain in the pelvis, and the right upper quadrant trocar site was closed by approximating the skin with staples. We then proceeded to open the ileostomy. This was matured with interrupted 4-0 Dexon stitches. Sponge and instrument counts were correct x2. The patient was transferred to the Postanesthesia Care Unit in stable condition. ASSISTANT SURGEON(S): Kim Rhoads, M.D. If the assistant surgeon is other than a qualified resident, I certify that the services were medically necessary and there was no qualified resident available to perform the services.