VACS - Yale School of Medicine
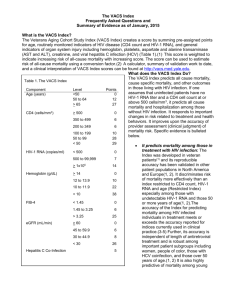
advertisement

*Correlations are shown as absolute values. Starred biomarkers demonstrated NEGATIVE correlations with the indicated biomarker of inflammation. Specifically, eGFR, hemoglobin, and CD4 count were all negatively correlated with all three biomarkers of inflammation. # 796 Biomarkers of Inflammation, Coagulation and Monocyte Activation Are Strongly Associated with the VACS Index among Veterans on cART Amy Justice*1,2, Matthew Freiberg3, Russell Tracy4, Janet Tate1,2, Matthew Goetz5, Adeel Butt3, Maria Rodriguez-Barradas6, Cynthia Gibert7, Kris Ann Oursler8, Kendall Bryant9, for the Veterans Aging Cohort Study (VACS) 1Yale University, New Haven, CT, US~ 2VA Connecticut Healthcare System, West Haven, CT, US~ 3University of Pittsburgh, Pittsburgh, PA, US~ 4University of Vermont, Burlington, VT, US~ 5VA Los Angeles Healthcare System, Los Angeles, CA, US~ 6Baylor College of Medicine, Houston, TX, US and Michael E. DeBakey VA Medical Center, Houston, TX, US~ 7VA Medical Center, Washington, DC, US and George Washington Univ., Washington, DC, US~ 8Univ. of Maryland-Baltimore, Baltimore, MD, US and Baltimore VA Medical Center, Baltimore, MD, US~ and 9National Institute on Alcohol Abuse and Alcoholism, Bethesda, MD, US BACKGROUND Everywhere ART available: Most patients achieve viral suppression Incident AIDS events are rare and variably associated with mortality Life expectancy is extended HIV Associated Non AIDS (HANA) Conditions determine disease burden We need a clinically accessible and reasonably standardized approach to tracking disease progression that: Integrates CD4 count, HIV-1 RNA, and age Includes measures of hematologic, liver, and renal disease BACKGROUND RESULTS continued METHODS Scoring For Indices* Component Value includes HIV infected Veterans and an age/race/site matched control group of uninfected Veterans in care. Age Tissue Samples: In 2005-2006 we collected and banked blood and DNA specimens on consenting subjects enrolled in VACS 8. 1532 HIV infected participants consented to provide blood specimens. Blood specimens were collected using serum separator and EDTA blood collection tubes. After collection, blood specimens were shipped to a central repository. CD4 Count <50 50-64 >65 >500 350-499 200-349 100-199 50-99 <50 <500 500 to 5 log >5 log >14 12-13.9 10-11.9 <10 <1.45 1.45-3.24 >3.25 The Veterans Aging Cohort Study (VACS): VACS has been well described and Clinical Laboratory Tests and Calculating the VACS Index: The VACS Index is composed of routinely collected laboratory tests of organ system functioning and age (Table 1). Since our initial publication, we have refined the VACS Index by omitting variables that are increasingly uncommon (AIDS defining Illnesses), variably associated with mortality (AIDS defining Illnesses), or inconsistently measured across cohorts (AIDS defining illnesses, diagnoses of substance abuse, hepatitis B co infection). The Index is based on age and laboratory tests recommended in current HIV care guidelines. Hepatitis C is considered present after a single sero positive test until a subsequent test demonstrates viral clearance. Markers of Inflammation: We selected soluble interleukin-6 (IL-6; systemic inflammation), fibrin fragment D-dimer (procoagulant activity), and soluble CD14 (sCD14; lipopolysaccharide-mediated monocyte activation) as sentinel markers of inflammation because prior work suggests that these represent important mechanisms for accelerated aging, end organ damage, and mortality among those aging with HIV infection. Biochemical analyses were performed at the Laboratory for Clinical Biochemistry Research at the University of Vermont under the supervision of Dr. Russell Tracy. (years) (mm3) HIV-1 RNA (copies/ml) Hemoglobin (g/dL) FIB 4 = (age*ALT/platelets *sqrt(ALT) eGFR = 186.3*creatinine-1.154 *age-0.203 Hepatitis C Sero Status >60 45-59.9 30-49.9 <30 Negative Positive VACS Index Restricted Index 0 12 27 0 6 6 10 28 29 0 7 14 0 10 22 38 0 6 25 0 23 44 0 10 10 19 40 46 0 11 25 0 6 8 26 0 5 *Points for each component are summed. Prognostic Model Sample Characteristics We have developed the Veterans Aging Cohort Study Risk Index (VACS Index) and demonstrated that it accurately predicts mortality among people initiating ART and those on ART for extended periods (see poster # 793). Here we explore whether these markers are associated with the Index and whether addition of these markers improves prediction of mortality. Total Gender Male Race White Black Other Age <50 50 to 64 > 65 CD4 >500 350 to 499 300 to 349 100 to 299 50 to 99 < 50 VL < 500 500 to < 5log > 5log Hgb >14 12 to 13.9 10 to 11.9 < 10 Fib 4 < 1.45 1.45 to 3.25 >3.25 eGFR >60 45 to 59.9 30 to 49.9 < 30 Hep C Yes N 1304 1265 251 892 114 489 740 73 434 297 279 155 69 68 915 317 70 664 483 139 16 714 460 128 1200 56 17 29 585 Discrimination* for 5 Year Mortality (%) (97.2) (19.3) (68.5) (8.8) (37.6) (56.8) (5.6) (33.3) (22.8) (21.4) (11.9) (5.3) (5.2) (70.3) (24.3) (5.4) (51.0) (37.1) (10.7) (1.2) (54.8) (35.3) (9.8) (92.2) (4.3) (1.3) (2.2) (44.9) Statistical Analyses: We compared the associations of the VACS Index, the Restricted Index and each of their components with IL-6, D-dimer, and sCD14. Because these markers of inflammation are not normally distributed, we used spearman rank correlation to measure association. In nested Cox models we estimated the unadjusted and the adjusted association of each marker of inflammation with mortality. Since we had complete data on 99.8% (1302/1304) of sampled subjects, we did not impute values. We then conducted nested Cox regression models to determine whether IL-6, D-dimer, or sCD14 added independent prognostic information to the VACS Index by improving the discrimination of the Index for all cause mortality. Biomarker VACS Index Restricted Index Alone n/a 0.80 0.75 +IL-6 0.74 0.81 0.80 +D-dimer 0.73 0.82 0.80 +sCD14 0.72 0.81 0.80 +all three 0.76 0.82 0.80 *Discrimination measured using c statistics. 1.8 1.6 1.4 Restricted Index Score 1.2 D-dimer Background: Composed of age and routine clinical data, the Veterans Aging Cohort Study (VACS) Index is more predictive of mortality among those with HIV infection than an index restricted to CD4 count, HIV-1 RNA, and age. We ask whether biomarkers of inflammation (IL-6), coagulation (D-dimer), and lipopolysaccharide-mediated monocyteactivation (sCD14) improve the prognostic discrimination of the VACS index. Methods: 1311 HIV infected subjects on cART from the VACS 8 Site Study had samples drawn and analyzed for IL-6, d-dimer, and sCD14. Using clinical tests performed closest to the date of sample collection, an HIV Restricted Index, composed of age, CD4 count, and HIV-1 RNA was compared to the VACS Index which also includes hemoglobin, AST, ALT, platelet count, HCV antibody, and creatinine. We tested association using Spearman correlation and predictive discrimination using C statistics calculated from proportional hazards models. Results: Among the 1311 patients on cART with samples, 77 died. The VACS Index was correlated with each biomarker (0.36-0.42) and these correlations were higher than for the HIV Restricted Index (0.24-0.29). In multivariate analyses, the VACS Index (C statistic 0.80) was more discriminating of mortality than any biomarker alone (C statistic 0.720.74), all three biomarkers together (C statistic 0.76) or the HIV Restricted Index (C statistic 0.75) (p for all comparisons<0.001). Addition of these biomarkers to the indices improved prediction for both indices but discrimination remained superior for the VACS Index compared to the Restricted Index (0.82 vs. 0.80. p<0.001). Results were similar when stratified by level of viral suppression and HCV serostatus. Conclusions: Biomarkers of inflammation, coagulation, and lipopolysaccharide-mediated monocyte activation were highly correlated with the VACS Index biomarkers Correlation with Biomarkers SUMMARY The VACS Index is more strongly correlated with biomarkers of inflammation, coagulation and monocyte activation than an index restricted to CD4 count, HIV-1 RNA, and age. The VACS Index is also more predictive of mortality than any of these markers (alone or in combination) or than the Restricted Index. Addition of D-dimer to the VACS Index improves discrimination of mortality as much as addition of all three. CONCLUSION: The VACS Index is more associated with markers of chronic inflammation and mortality than the Restricted Index, but can be improved by the addition of D dimer, a test that is routinely available in clinical settings. R² = 0.7748 1.0 0.8 0.6 0.4 0.2 0.0 0 20 40 60 80 100 1.8 1.6 1.4 VACS Risk Index score 1.2 D-dimer ABSTRACT R² = 0.961 1.0 0.8 0.6 0.4 0.2 0.0 0 20 40 60 80 100 SUPPORTING REFERENCES: D'Arminio MA, et al. The changing incidence of AIDS events in patients receiving HAART. Arch Intern Med 2005;165(4):416-423. Mocroft A, et al. Variable impact on mortality of AIDS-defining events diagnosed during cART. Clin Infect Dis 2009;48(8):1138-1151. Justice AC, et al. Towards a combined prognostic index for survival in HIV infection. HIV Med 2009. Sandler N, et al. Plasma Levels of Soluble CD14 Predict Mortality in HIV Infection. 17th CROI Abstract # 304. 2-16-0010. Kuller LH, et al. Inflammatory and coagulation biomarkers and mortality in patients with HIV infection. PLoS Med 2008;5(10):e203. Justice AC, et al. Veterans Aging Cohort Study (VACS). Med Care 2006;44(8 Suppl 2):S13-S24. Aberg JA , et al. Primary care guidelines for the management of persons infected with HIV... Clin Infect Dis 2009;49(5):651-681. Vallet-Pichard A, et al. FIB-4... Hepatology 2007;46(1):32-36. Ravasi G, et al. Comparison of glomerular filtration rate estimates vs. 24-h creatinine clearance in HIV…. HIV Med 2009;10(4):219-228. ACKNOWLEDGEMENT: supported by NIH: NIAAA (2U10AA13566) and NHLBI (3R01HL095136-03)