Summary of Evidence Supporting Veterans Aging Cohort Study Index as of February 2016
advertisement

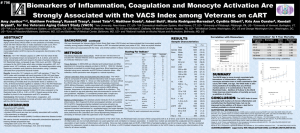
The VACS Index Frequently Asked Questions and Summary of Evidence as of February, 2016 What is the VACS Index? The Veterans Aging Cohort Study Index (VACS Index) creates a score by summing pre-assigned points for age, routinely monitored indicators of HIV disease (CD4 count and HIV-1 RNA), and general indicators of organ system injury including hemoglobin, platelets, aspartate and alanine transaminase (AST and ALT), creatinine, and viral hepatitis C infection (HCV) (Table 1) (1).. The score is weighted to indicate increasing risk of all-cause mortality with increasing score. The score can be used to estimate risk of all-cause mortality using a conversion factor.(2). A calculator, summary of validation work to date, and a clinical interpretation of VACS Index scores can be found at http://vacs.med.yale.edu. Table 1. The VACS Index Component Age (years) Level <50 50 to 64 > 65 CD4 (cells/mm3) > 500 350 to 499 200 to 349 100 to 199 50 to 99 < 50 0 6 6 10 28 29 HIV-1 RNA (copies/ml) < 500 500 to 99,999 > 1x105 0 7 14 Hemoglobin (g/dL) > 14 12 to 13.9 10 to 11.9 < 10 0 10 22 38 FIB-4 < 1.45 1.45 to 3.25 > 3.25 0 6 25 eGFR (mL/min) > 60 45 to 59.9 30 to 44.9 < 30 0 6 8 26 Hepatitis C Co-Infection Points 0 12 27 5 What does the VACS Index Do? The VACS Index predicts all-cause mortality, cause-specific mortality, and other outcomes in those living with HIV infection. If one assumes that uninfected patients have no HIV-1 RNA titer and a CD4 cell count at or above 500 cells/mm3, it also predicts all-cause mortality and hospitalization among those without HIV infection. The index responds to important changes in risk related to treatment and health behaviors. It improves accuracy of provider assessment (clinical judgment) of mortality risk. Specific evidence is bulleted below. It predicts mortality among those with HIV infection The Index was developed in veteran patients(1) and its accuracy has been validated in other patient populations in North America and Europe(1, 2). It discriminates risk of mortality more effectively than an index restricted to CD4 count, HIV-1 RNA and age (Restricted Index) especially among those with undetectable HIV-1 RNA and those 50 or more years of age(1, 2).The accuracy of the Index for predicting mortality among HIV infected individuals in treatment meets or exceeds the accuracy reported for indices currently used in clinical practice(3-5). Further, its accuracy is independent of length of time on antiretroviral treatment and is robust among important patient subgroups including women, people of color, those with HCV coinfection, and those over 50 years of age(1, 2). It is also predicts mortality among young active duty military, relatively free of comorbid disease(6) and among those initiating salvage antiretroviral therapy after becoming resistant to at least two classes of antiretroviral therapy(7). It predicts mortality among uninfected individuals If you assume that those without HIV infection have no HIV-1 RNA (i.e. 0 points) and a CD4 cell count above 500 cells/mm3 (i.e. 0 points), the VACS Index also predicts mortality among those without HIV infection. This has been shown for 30-day mortality from MICU admission(8) and for long term (median of 5 years) mortality(9). It predicts outcomes after admission for bacterial pneumonia Among HIV infected and uninfected (age 50+ years) veterans the index predicts 30-day mortality, length of stay, and readmission(10). It is associated with frailty Frailty is defined as decreased ability to recover from additional injury(11). The index is associated with increased risk for a number of adverse outcomes including mortality, hospitalization, geriatric syndromes (falls, fragility fractures, and cognitive decline) and is strongly associated with chronic inflammation. The VACS Index is correlated with markers of chronic inflammation, microbial translocation, and hypercoagulability (cystatin C, TNF alpha, IL-6, soluble CD14, soluble CD163, and D-dimer)(12-14), with measures of functional performance(15) and sarcopenia(16), and with multiple measures of neuro-cognitive performance(17). The VACS Index predicts morbidity including hospitalization, medical intensive care unit admission(18), and fragility fractures(19). It is also associated with autonomic neuropathy(20). It is an effective measure of physiologic frailty (21, 22). Few individuals demonstrated frailty based on the adapted frailty related phenotype(23).When compared with an adapted version of the frailty related phenotype, the VACS Index more accurately predicted both all-cause mortality and hospitalization among HIV infected and uninfected individuals. Of note, the approach to frailty employed by the VACS Index is more attuned to the Rockwood conceptualization(24) of frailty as accumulation of deficits than that of Fried(25) which describes a clinical syndrome. It responds to important changes in health and health behaviors VACS Index scores change in response to antiretroviral initiation(26) and interruption(6), and discriminate among levels of ART adherence(26). VACS Index scores differ by level of smoking, alcohol consumption and hypertension(27, 28). VACS Index scores predict weight gain in the first 12 months after ART initiation(29). When levels of alcohol consumption change among HIV infected subjects, the index score also changes. Similarly, when HIV infected subjects in treatment for substance abuse have positive urine toxicology screens, their scores are higher than when the same subjects have negative toxicology screens. (Papers reporting responsiveness of the VACS Index to changes in alcohol and substance use are in preparation). It is accurate in a wide range of patient populations VACS Index predicts all-cause mortality in a wide range of HIV infected populations including those first initiating ART(30), after the first year of ART(1, 2), among highly treatment experienced patients(7) and among young military recruits(6). It predicts well among men and women, older and younger subjects, those with and without HCV coinfection, and those with and without HIV-1 viral suppression(1, 2, 7). It predicts cause-specific mortality VACS Index predicts both HIV and non-HIV associated mortality better than an index restricted to CD4 count, HIV-1 RNA, and age(1). It predicts cardiovascular mortality as accurately as it predicts all-cause mortality(31). It improves accuracy of provider assessment of risk Although providers have results of routine clinical biomarkers included in the VACS Index available at the time of assessment, provider assessments may not accurately incorporate the implications of these tests for risk of mortality. For both veterans with and without HIV infection, provider assessments of severity of illness (“How sick is this patient?”) and risk of 10 year mortality were substantially less accurate than estimates based on the VACS Index and were considerably improved when combined with the VACS Index(32). Thus, the VACS Index adds important insight to provider assessment of severity of illness and risk of mortality. How modifiable is the VACS Index? Over the course of the first 12 months of ART, CD4 and HIV-1 RNA change dramatically, but so do level of hemoglobin, FIB 4, and, to a lesser extent, eGFR. Values also differ by level of adherence to ART, by smoking, by alcohol, by HCV status, by number of non-ARV medications, and by physical function. As mentioned above under responsiveness to changes in health and health behaviors, VACS Index scores rise during negative health behaviors (alcohol and substance use) and fall when these behaviors are diminished or extinguished. It is likely that successful interventions in any or all of these domains would alter the VACS Index Score. (A paper summarizing how VACS Index scores change over the first 12 months of ART using data from NA-ACCORD and ART-CC combined is under review.) Why is this useful? Potential applications of the VACS Index include mechanistic and clinical research as well as clinical care. Translational Research The VACS Index can inform mechanistic studies focused on long term pathophysiologic effects of aging with HIV. We have demonstrated the stronger association of the VACS Index to markers of chronic inflammation and hypercoagulability compared with an Index restricted to age, CD4 count and HIV-1 RNA(12) and when compared with the Framingham Index(14). Of note, hemoglobin was the single index component most associated with D-dimer(12). The strong and independent association of liver injury (measured by FIB 4) and of anemia (measured by hemoglobin) with health outcomes among HIV infected individuals on ART is consistent with the theory that early changes after HIV infection undermine the gut mucosa and expose the liver to a greater burden of microbial products contributing to progressive liver dysfunction and chronic inflammation(33). Clinical Research Observational studies frequently struggle with issues around confounding by indication when studying post marketing treatment effects. The VACS Index could be used as a powerful adjustment either directly or as part of a propensity score. Randomized trials often need to insure that the arms of the trial are equally at risk for the observed outcome (i.e., that randomization worked).The VACS Index offers a means of making this determination, accounting for a number of important predictors of major clinical outcomes. Conversely, randomization could be stratified by VACS Index score. Finally, change in VACS Index score could be used as a response measure for a number of diverse interventions, thereby allowing assessment of their comparative effectiveness. Clinical Care Potential applications include estimating short and long term risk of morbidity and mortality, estimating life expectancy, quantifying response to interventions, and detecting HIV and non-HIV treatment toxicity. The index may also be useful in motivating behavior change and prioritizing treatment. For example, the VACS Index might help inform medical decision making regarding hospitalization, admission to the Medical Intensive Care Unit, timing of discharge, and discharge planning. The index might also inform decisions regarding frequency of clinical followup, elective surgical procedures, nursing home placement, and other case management issues. While the index does not include all potentially important targets for intervention (smoking, CVD risk factors, alcohol intake, ART adherence, etc.), it responds to differences in these factors and therefore reflects their effects. We are currently developing an extension of the VACS Index Calculator app (http://vacs.med.yale.edu) that would support use of the index to motivate health behavior change. How are others using the VACS Index? Research Two NIH funded, alcohol intervention trials are underway which include the VACS Index as an outcome. The AIDS Clinical Trials Group has begun to use the VACS Index in randomized trials (34) Independent groups have begun to use the VACS Index as a measure of frailty or severity of illness(13, 14, 17, 20, 21, 35-41). Clinical Care As of February 2016, the VACS Index Risk Calculator (link above) has been accessed 76,000 times since March of 2013 and most of these represent repeated use (first time visitors 5,400). Fenway Healthcare System in Boston is exploring using the VACS Index to identify patients for intensive case management. The San Francisco General Hospital HIV clinic has incorporated the VACS Index scoring into its electronic medical record and is using it in patient management. In Italy, the VACS Index is calculated on every patient seen at the University of Modena Metabolic Clinic (a clinic of over 4000 patients) using an automated application. A group in Italy (FB Communication) is developing an Italian language app for the VACS Index for use in Italy. References 1. 2. 3. 4. 5. 6. 7. 8. 9. 10. 11. 12. 13. 14. Tate JP, Justice AC, Hughes MD, Bonnet F, Reiss P, Mocroft A, et al. An internationally generalizable risk index for mortality after one year of antiretroviral therapy. AIDS. 2013;27(4):563-72. Justice AC, Modur SP, Tate JP, Althoff KN, Jacobson LP, Gebo KA, et al. Predictive accuracy of the Veterans Aging Cohort Study index for mortality with HIV infection: a North American cross cohort analysis. J. Acquir. Immune. Defic. Syndr. 2013;62(2):149-63. Vasan RS. Biomarkers of cardiovascular disease: molecular basis and practical considerations. Circulation. 2006;113(19):2335-62. D'Agostino RB, Sr., Grundy S, Sullivan LM, Wilson P. Validation of the Framingham coronary heart disease prediction scores: results of a multiple ethnic groups investigation. JAMA. 2001;286(2):180-7. Yourman LC, Lee SJ, Schonberg MA, Widera EW, Smith AK. Prognostic indices for older adults: a systematic review. JAMA. 2012;307(2):182-92. Bebu I, Tate J, Rimland D, Mesner O, Macalino GE, Ganesan A, et al. The VACS Index Predicts Mortality in a Young, Healthy HIV Population Starting Highly Active Antiretroviral Therapy. J. Acquir. Immune. Defic. Syndr. 2014;65(2):226-30. Brown ST, Tate JP, Kyriakides TC, Kirkwood KA, Holodniy M, Goulet JL, et al. The VACS index accurately predicts mortality and treatment response among multi-drug resistant HIV infected patients participating in the options in management with antiretrovirals (OPTIMA) study. PLoS One. 2014;9(3):e92606. Akgun KM, Tate JP, Pisani M, Fried T, Butt AA, Gibert CL, et al. Medical ICU admission diagnoses and outcomes in human immunodeficiency virus-infected and virus-uninfected veterans in the combination antiretroviral era. Crit. Care. Med. 2013;41(6):1458-67. Tate JP, Brown ST, Rimland D, Rodriguez-Barradas M, Justice AC, Team VP. Comparison of VACS Index Performance in HIV-Infected and Uninfected Veterans from 2000 to 2010. 18th International Workshop on HIV Observational Databases Sitges, IWHOD, 2014/03/27 2014. Spain. Poster. Barakat LA, Juthani-Mehta M, Allore H, Trentalange M, Tate J, Rimland D, et al. Comparing clinical outcomes in HIV-infected and uninfected older men hospitalized with communityacquired pneumonia. HIV Med. 2015;16(7):421-30. Walston J, Hadley EC, Ferrucci L, Guralnik JM, Newman AB, Studenski SA, et al. Research agenda for frailty in older adults: toward a better understanding of physiology and etiology: summary from the American Geriatrics Society/National Institute on Aging Research Conference on Frailty in Older Adults. J.Am.Geriatr.Soc. 2006;54(6):991-1001. Justice AC, Freiberg MS, Tracy R, Kuller L, Tate JP, Goetz MB, et al. Does an index composed of clinical data reflect effects of inflammation, coagulation, and monocyte activation on mortality among those aging with HIV? Clin. Infect. Dis. 2012;54(7):984-94. Williams B, Livak B, Bahk M, Keating SM, Adeyemi OM. SCD14 and SCD163 Levels Are Correlated with VACS Index Scores: Initial Data from the Blunted Immune Recovery in CORE Patients with HIV (BIRCH) Cohort. AIDS Res Hum Retroviruses. 2015;Epub. Mooney S, Tracy R, Osler T, Grace C. Elevated Biomarkers of Inflammation and Coagulation in Patients with HIV Are Associated with Higher Framingham and VACS Risk Index Scores. PLoS One. 2015;10(12):e0144312. 15. 16. 17. 18. 19. 20. 21. 22. 23. 24. 25. 26. 27. 28. 29. 30. 31. Erlandson KM, Allshouse AA, Jankowski C, Duong S, Mawhinney S, Kohrt WM, et al. Comparison of functional status instruments in HIV-infected adults on effective antiretroviral therapy. HIV.Clin.Trials. 2012;13(6):324-34. Oursler KK, Tate JP, Gill TM, Crothers K, Brown TT, Crystal S, et al. Association of the veterans aging cohort study index with exercise capacity in HIV-infected adults. AIDS Res Hum Retroviruses. 2013;29(9):1218-23. Marquine MJ, Umlauf A, Rooney AS, Fazeli PL, Gouaux BD, Paul WS, et al. The Veterans Aging Cohort Study Index is Associated With Concurrent Risk for Neurocognitive Impairment. J. Acquir. Immune. Defic. Syndr. 2014;65(2):190-7. Akgun KM, Gordon K, Pisani M, Fried T, McGinnis KA, Tate JP, et al. Risk factors for hospitalization and medical intensive care unit (MICU) admission among HIV infected Veterans. J. Acquir. Immune. Defic. Syndr. 2013;62(1):52-9. Womack JA, Goulet JL, Gibert C, Brandt CA, Skanderson M, Gulanski B, et al. Physiologic frailty and fragility fracture in HIV-infected male veterans. Clin. Infect. Dis. 2013;56(10):1498-504. Robinson-Papp J, Sharma SK. Autonomic neuropathy in HIV is unrecognized and associated with medical morbidity. AIDS Patient Care STDS. 2013;27(10):539-43. Escota G, Patel P, Brooks JT, Bush T, Conley L, Baker J, et al. The VACS Index is an effective tool to assess baseline frailty status in a contemporary cohort of HIV-infected persons. AIDS Res Hum Retroviruses;31(3):313-7. Justice AC, McGinnis KA, Tate JP, Braithwaite RS, Bryant KJ, Cook RL, et al. Risk of Mortality and Physiologic Injury Evident with Lower Alcohol Exposure Among HIV Infected Compared with Uninfected Men. Drug Alcohol Depend. In press. Akgun KM, Tate JP, Crothers K, Crystal S, Leaf DA, Womack JA, et al. An adapted frailtyrelated phenotype and the VACS index as predictors of hospitalization and mortality in HIVinfected and uninfected individuals. J. Acquir. Immune. Defic. Syndr. 2014;67(4):397-404. Rockwood K, Bergman H. FRAILTY: A Report from the 3(rd) Joint Workshop of IAGG/WHO/SFGG, Athens, January 2012. Can.Geriatr.J. 2012;15(2):31-6. Fried LP, Ferrucci L, Darer J, Williamson JD, Anderson G. Untangling the concepts of disability, frailty, and comorbidity: implications for improved targeting and care. J.Gerontol.A Biol.Sci.Med.Sci. 2004;59(3):255-63. Tate JP, Justice AC, Team ftVP. Change in a prognostic index for survival in HIV infection after one year on cART by level of adherence. 48th Annual Meeting of the Infectious Disease Society of America. 2010;Vancouver, British Columbia. Tate J, Freiberg M, AC J. Do Risk Factors for Cardiovascular Disease Improve VACS Index Prediction of All Cause Mortality? 16th International Workshop on HIV Observational Databases (IWHOD), 3/29/2012 2012. Athens, Greece. 2012. Bryant K, McGinnis KA, Tate JP, Fiellin D, Justice AC. The VACS Index Score Varies By Alcohol Level In Those With HIV. Research Society on Alcoholism (RSA) Annual Conference, 2013 2013. Orlando, Florida. Yuh B, Tate J, Butt AA, Crothers K, Freiberg M, Leaf D, et al. Weight change after antiretroviral therapy and mortality. Clin Infect Dis. 2015;60(12):1852-9. Justice AC, McGinnis KA, Skanderson M, Chang CC, Gibert CL, Goetz MB, et al. Towards a combined prognostic index for survival in HIV infection: the role of 'non-HIV' biomarkers. HIV.Med. 2009;11(2):143-51. Justice AC, Tate JP, Freiberg MS, Rodriguez-Barradas MC, Tracy R. Reply to Chow et al. Clin. Infect. Dis. 2012;55(5):751-2. 32. 33. 34. 35. 36. 37. 38. 39. 40. 41. Justice AC, Tate JP, Brown ST, Gibert C, Rodriguez-Barradas M, Rimland D, et al. Can the Veterans Aging Cohort Study Index Improve Clinical Judgement for Both HIV Infected and Uninfected Veterans? Society of General Medicine (SGIM) 36th Annual Meeting. 2013. Deeks SG, Tracy R, Douek DC. Systemic Effects of Inflammation on Health during Chronic HIV Infection. Immunity. 2013;39(4):633-45. Tashima KT, Smeaton L, Klingman KL, Andrade A, Eron JJ, Fichtenbaum CJ, et al. Mortality among HIV+ Participants Randomized to Omit NRTIs vs. Add NRTIs in OPTIONS (ACTG A5241). 21st Conference on Retroviruses and Opportunistic Infections (CROI). 2014. Adeyemi O, Livak B. Higher Veterans Aging Cohort Study (VACS) index scores in HIVpositive adults with CD4 counts <200 cells/mm3 despite viral suppression. J. Acquir. Immune. Defic. Syndr. 2013;63(2):e78-81. Furuya-Kanamori L, Kelly MD, McKenzie SJ. Co-morbidity, ageing and predicted mortality in antiretroviral treated Australian men: a quantitative analysis. PLoS. One. 2013;8(10):e78403. Huggan PJ, Foo RM, Olszyna D, Chew NS, Smitasen N, Mukhopadhyay A, et al. Presentation and outcome amongst older Singaporeans living with human immunodeficiency virus/acquired immunodeficiency syndrome (HIV/AIDS): does age alone drive excess mortality? Ann. Acad. Med. Singapore. 2012;41(12):581-6. Marquine MJ, Sakamoto M, Dufour C, Rooney A, Fazeli P, Umlauf A, et al. The impact of ethnicity/race on the association between the Veterans Aging Cohort Study (VACS) Index and neurocognitive function among HIV-infected persons. J Neurovirol. 2015;Epub. Cohen MH, Hotton AL, Hershow RC, Levine A, Bacchetti P, Golub ET, et al. Gender-Related Risk Factors Improve Mortality Predictive Ability of VACS Index Among HIV-Infected Women. J Acquir Immune Defic Syndr. 2015;70(5):538-44. Erlandson KM, Allshouse AA, Jankowski CM, MaWhinney S, Kohrt WM, Campbell TB. Functional impairment is associated with low bone and muscle mass among persons aging with HIV infection. J.Acquir.Immune.Defic.Syndr. 2013;63(2):209-15. Erlandson KM, Allshouse AA, Jankowski CM, Mawhinney S, Kohrt WM, Campbell TB. Relationship of physical function and quality of life among persons aging with HIV infection. AIDS. 2014;28(13):1939-43.