Homeostasis – Chapter 1
advertisement
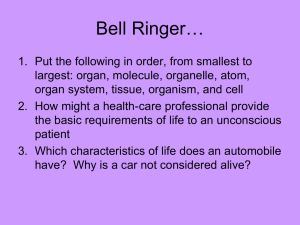
Chapter 01 Lecture Outline* Homeostasis: A Framework for Human Physiology Eric P. Widmaier Boston University Hershel Raff Medical College of Wisconsin Kevin T. Strang University of Wisconsin - Madison *See PowerPoint Image Slides for all figures and tables pre-inserted into PowerPoint without notes. 1 Copyright © The McGraw-Hill Companies, Inc. Permission required for reproduction or display. Chapter 1 Homeostasis: A framework for human physiology 1. Cells, the fundamental units of life, exchange nutrients and wastes with their surroundings: The intracellular fluid is “conditioned by”… the interstitial fluid, which is “conditioned by” … the plasma, which is “conditioned by” … the organ systems it passes through. 2 Homeostasis: A framework for human physiology Homeostasis refers to the dynamic mechanisms that detect and respond to deviations in physiological variables from their “set point” values by initiating effector responses that restore the variables to the optimal physiological range. 3 Homeostasis • Most of the common physiological variables of the body are maintained within a predictable range. • Examples of such physiological variables: – Blood pressure – Body temperature – Blood glucose levels 4 Figure 1-1 5 Muscle Cells and Tissues • There are 3 types of muscle cells in the human body: Cardiac, Skeletal and Smooth. • Control of the cardiac and smooth muscle is involuntary, while skeletal is voluntary. • Muscle cells with be covered in depth in Chapter 9. 6 Neurons and Nervous Tissue • A neuron is a cell of the nervous system that is specialized to initiate, integrate and conduct electrical signals to other cells. • A collection of neurons forms nervous tissue (brain or spinal cord). • Axons from many neurons are packaged together along with connective tissue to form a nerve. • Neurons, nervous tissue, and the nervous system will be covered in Chapter 6. 7 Epithelial cells and epithelial tissue • Epithelial cells are specialized for the selective secretion and absorption of ions and organic molecules, and for protection. • These cells are characterized and named according to their unique shapes, including cuboidal (cube-shaped), columnar (elongated), squamous (flattened) and ciliated. • Epithelial tissue (known as an epithelium) may form from any type of epithelial cell. Epithelia may be arranged in single-cell thick tissue, called a simple epithelium, or a thicker tissue consisting of numerous layers of cells, called a stratified epithelium. • The type of epithelium that forms in a given region of the body reflects the function of that particular epithelium. For example, the epithelium that lines the inner surface of the main airway, the trachea, consists of ciliated epithelial cells (see Chapter 13). 8 Epithelial cells and epithelial tissue • Epithelia are located at the surfaces that cover the body or individual organs, and they line the inner surfaces of the tubular and hollow structures within the body. • Epithelial cells rest on an extracellular protein layer called the basement membrane. The side of the cell anchored to the basement membrane is called the basolateral side; the opposite side, which typically faces the interior, is called the apical side. • A defining feature of many epithelia is that the two sides of all the epithelial cells in the tissue may perform different physiological functions. • In addition, the cells are held together along their lateral surfaces by extracellular barriers called tight junctions Tight junctions enable epithelia to form boundaries between body compartments and to function as selective barriers regulating the exchange of molecules. 9 Figure 1-2 10 Connective tissue cells and connective tissue • Connective tissue cells connect, anchor, and support the structures of the body. • • • • • • Types of connective tissues include: Loose Connective Dense Connective Blood Cartilage Adipose 11 What surrounds the cells? • The immediate environment that surrounds each individual cell in the body is the extracellular fluid and extracellular matrix (ECM). • ECM consists of a mixture of proteins, polysaccharides, and in some cases, minerals. • The matrix serves two general functions: (1) It provides a scaffold for cellular attachments, and (2) it transmits information, in the form of chemical messengers, to the cells to help regulate their activity, migration, growth, and differentiation. • The proteins of the extracellular matrix consist of fibers—ropelike collagen fibers and rubberband-like elastin fibers—and a mixture of nonfibrous proteins that contain carbohydrate. 12 Organs and Organ Systems • Organs are composed of multiple tissue types (example: blood vessels have layers of smooth muscle cells, endothelial cells and fibroblasts). • Organ systems contain multiple organs that work together (example: the urinary system has the kidney, ureters, urethra, bladder). 13 Table 1-1, on page 5 in the text, outlines the structural components and functions of the major organ systems in the body. 14 15 Body Fluids and Compartments • The term “body fluids,” is used to refer to the watery solution of dissolved substances (oxygen, nutrients, etc.) present in the body. • The fluid in the blood and surrounding cells is called extracellular fluid (i.e., outside the cell). • About 20–25 percent is in the fluid portion of blood (plasma) and the remaining 75–80 percent of the extracellular fluid lies around and between cells and is known as the interstitial fluid. • The space containing interstitial fluid is called the interstitium. Therefore, the total volume of extracellular fluid is the sum of the plasma and interstitial volumes. 16 Body Fluids and Compartments • Intracellular fluid is the fluid located inside the cells. • The composition of the extracellular fluid is very different from that of the intracellular fluid. • Maintaining differences in fluid composition across the cell membrane is an important way in which cells regulate their own activity. 17 Figure 1-3 ICF ISF plasma organs internal environment external environment Exchange and communication are key concepts for understanding physiological homeostasis. 18 Homeostasis • Homeostasis is a dynamic, not a static, process. • Physiological variables can change dramatically over a 24-hr. period, but the system is still in overall balance. • When homeostasis is maintained, we refer to physiology; when it is not, we refer to pathophysiology. 19 Figure 1-4 Blood glucose levels increase after eating. Levels return to their set point via homeostasis. This is an example of dynamic constancy. Levels change over short periods of time, but remain relatively constant over long periods of time. 20 Figure 1-5 Interpret the arrows in textbook’s flow charts as “leads to” or “causes.” (e.g., decreased room temperature causes increased heat loss from the body, which leads to a decrease in body temperature, etc.) 21 System Controls • Feedback loops or systems are a common mechanism to control physiological processes. • A positive feedback system (also called a feed forward) enhances the production of the product. • A negative feedback system shuts the system off once the set point has been reached. 22 Figure 1-6 Negative Feedback “Active product” controls the sequence of chemical reactions by inhibiting the sequence’s rate-limiting enzyme, “Enzyme A.” 23 A strategy for exploring homeostasis (see Tables 1-2 & 1-3) • Identify the internal environmental variable. example: concentration of glucose in the blood • Establish the “set point” value for that variable. example: 70 to 110 mg glucose/dL of blood • Identify the inputs and outputs affecting the variable. example: diet and energy metabolism 24 A strategy for exploring homeostasis (see Tables 1-2 & 1-3) • Examine the balance between the inputs and outputs. example: resting versus exercising • Determine how the body monitors/senses the variable. example: certain endocrine cells in the pancreas “sense” changes in glucose levels • Identify effectors that restore the variable to its set point. example: a hormone that increases glucose synthesis by the liver Many homeostatic mechanisms utilize neural communication. 25 26 27 Reflexes • A reflex is a specific involuntary, unpremeditated, unlearned “built-in” response to a particular stimulus. • Example: pulling your hand away from a hot object or shutting your eyes as an object rapidly approaches your face. 28 Reflexes • The pathway mediating a reflex is known as the reflex arc. • An arc has several components: stimulus, receptor, afferent (incoming) pathway, integration center, efferent (outgoing) pathway, and effector. • A stimulus is defined as a detectable change in the internal or external environment. A receptor detects the change. The pathway the signal travels between the receptor and the integrating center is known as the afferent pathway. The pathway along which information travels away from the integration center to the effector is known as the efferent pathway • An integrating center often receives signals from many receptors, some of which may respond to quite different types of stimuli. Thus, the output of an integrating center reflects the net effect of the total afferent input; that is, it represents an integration of numerous bits of information. 29 Figure 1-7 Afferent and efferent pathways in temperature homeostasis. 30 Figure 1-8 Communication systems use signals that bind to receptors. 31 Non-nerve Reflexes • Almost all body cells can act as effectors in homeostatic reflexes. • There are, however, two specialized classes of tissues—muscle and gland—that are the major effectors of biological control systems. • In the case of glands, the effector may be a hormone secreted into the blood. • A hormone is a type of chemical messenger secreted into the blood by cells of the endocrine system (see Table 1–1). Hormones may act on many different cells simultaneously because they circulate throughout the body. 32 Types of Signals • Hormones are produced in and secreted from endocrine glands or in scattered cells that are distributed throughout another organ. • Neurotransmitters are chemical messengers that are released from the endings of neurons onto other neurons, muscle cells, or gland cells. 33 Chemical Messengers • Chemical messengers participate not only in reflexes, but also in local responses. • Communication signals in three categories: Endocrine: signal reaches often-distant targets after transport in blood. Paracrine: signal reaches neighboring cells via the ISF. Autocrine: signal affects the cell that synthesized the signal. 34 Points to Remember • A neuron, endocrine gland cell, and other cell types may all secrete the same chemical messenger. • In some cases, a particular messenger may function as a neurotransmitter, as a hormone, or as a paracrine/autocrine substance. • Example: Norepinephrine is a neurotransmitter in the brain and is also produced as a hormone by cells of the adrenal glands. 35 Figure 1-9 A given signal can fit into all 3 categories: (e.g., the steroid hormone cortisol affects the very cells in which it is made, the nearby cells that produce other hormones, and many distant targets, including muscles and liver.) Multi-factorial control of signal release adds more complexity. 36 Other Types of Cell Communication • There are two important types of chemical communication between cells that do not require secretion of a chemical messenger. 1. Gap junctions (physical linkages connecting the cytosol between two cells) allow molecules to move from one cell to an adjacent cell without entering the extracellular fluid. 2. Juxtacrine signaling is the chemical messenger not actually being released from the cell producing it, but rather is located in the plasma membrane of that cell. When the cell encounters another cell type capable of responding to the message, the two cells link up via the membrane-bound messenger. 37 Adaptation and Acclimatization • The term adaptation denotes a characteristic that favors survival in specific environments. • Acclimatization refers to the improved functioning of an already existing homeostatic system based on an environmental stress. • In an individual, acclimatizations are reversible; adaptations are not. 38 Biological Rhythms • Many body functions are rhythmical changes. • Example: circadian rhythm, which cycles approximately once every 24 h. • Waking and sleeping, body temperature, hormone concentrations in the blood, the excretion of ions into the urine, and many other functions undergo circadian variation. 39 Figure 1-10 asleep asleep A full analysis of the hormone cortisol requires not only knowledge of the signals that cause its synthesis and secretion but also consideration of biological rhythms. 40 What have biological rhythms to do with homeostasis? • They add an anticipatory component to homeostatic control systems and in effect are a feed-forward system operating without detectors. • The negative-feedback homeostatic responses are corrective responses. They are initiated after the steady state of the individual has been perturbed. • Biological rhythms enable homeostatic mechanisms to be utilized immediately and automatically by activating them at times when a challenge is likely to occur but before it actually does occur. 41 Balance in the Homeostasis of Chemical Substances in the Body • Many homeostatic systems regulate the balance between addition and removal of a chemical substance from the body. • Two important generalizations concerning the balance concept: (1) During any period of time, total-body balance depends upon the relative rates of net gain and net loss to the body; and (2) the pool concentration depends not only upon the total amount of the substance in the body, but also upon exchanges of the substance within the body. 42 Figure 1-11 Some of the potential inputs and outputs that can affect the “pool” of a material (like glucose) that is a dynamically regulated physiological variable. 43 Figure 1-12 Sodium homeostasis: Consuming greater amounts of dietary sodium initiates a set of dynamic responses that include greater excretion of sodium in the urine. Though not shown here, the amount excreted would likely exceed the amount ingested until the “set point” is restored. 44 Clinical Correlation • A 64-year-old, fair-skinned man in good overall health spent a very hot, humid summer day gardening in his backyard. After several hours in the sun, he began to feel dizzy and confused as he knelt over his vegetable garden. Although he had earlier been perspiring profusely, his sweating had eventually stopped. Because he also felt confused and disoriented, he could not recall for how long he had not been perspiring, or even how long it had been since he had taken a drink of water. He called to his wife, who was alarmed to see that his skin had turned a pale blue color. She asked her husband to come indoors, but he fainted as soon as he tried to stand. The wife called for an ambulance, and the man was taken to a hospital and diagnosed with a condition called heat stroke. What happened to this man that would explain his condition, and how does it relate to homeostasis? 45 You don’t have a figure for this but it would be really helpful to have a flow chart diagram here with the information for the clinical correlation 46 The End. 47