Transport of carbon dioxide
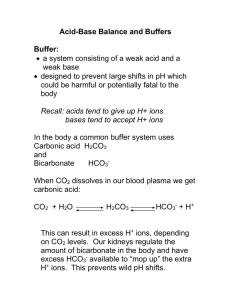
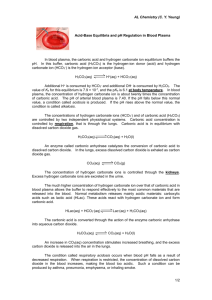
advertisement

Review exam questions http://www.youtube.com/watch?v=Qrvrs6R XxwY Starter - Key Word Revision Erythrocyte (RBC) Dissociation Partial pressure Oxyhaemoglobin (Hb + 4O2 HbO8) Biconcave Oxygen Dissociation Curve Diffusion Plasma Saturated Platelets Bone Marrow Blood Oxygen Association Carbon Dioxide Bohr Effect Leukocyte (WBC) Alveoli Haemoglobin Transport of carbon dioxide H+ OBJECTIVES Describe the 3 ways in which carbon dioxide is carried in the blood Describe the importance of the formation of hydrogen carbonate in the carrying of carbon dioxide in the blood. Describe and explain the Chloride shift. KEY TERMS Haemoglobin Carbamino-haemoglobin Carbonic Acid Carbonic anhydrase Haemoglobinic acid (HHb) Buffer Chloride Shift • Carbon dioxide is transported through the circulatory system in 3 ways: 1. Dissolved in plasma (5%) 2. Associated with Hb to form carbaminohaemoglobin (10%) (Changes shape of haemoglobin and encourages oxygen dissociation) Sequence of events in which hydrogen carbonate is formed is significant for a number of reasons 85% of CO2 is transported as hydrogen carbonate ions • CO2 dissolves in water to form carbonic acid (via carbonic anhydrase catalyst in RBC) CO2 + H2O H2CO3 • Carbonic acid releases H+ protons (acid dissociation – chemistry) H2CO3 HCO3- + H+ Question 1: What will happen to the nvironment within the erythrocyte? • H+ ions bind to Hb to form haemoglobinic acid Question 2: If Hb is absorbing H+ ions, what can we say Hb is acting as? Sequence of events in which hydrogen carbonate is formed is significant for a number of reasons 85% of CO2 is transported as hydrogen carbonate ions • H+ ions lower blood pH and combine with Hb to make haemoglobinic acid (HHb) decreasing Hb O2 affinity (Bohr) H+ + HB HHb • HCO3- ions diffuse out of erythrocyte. • Cl- diffuse into the cell to balance the charge CHLORIDE SHIFT Conclusion: • In a CO2-rich environment (i.e. at respiring tissue), more oxygen dissociates from oxyhaemoglobin • Oxygen dissociation curve shifts to the right (requires higher pO2 to saturate Hb due to H+ competition) • This is known as the Bohr effect Sequence of events in which hydrogen carbonate is formed is significant for a number of reasons 85% of CO2 is transported as hydrogen carbonate ions • CO2 dissolves in water to form carbonic acid (via carbonic anhydrase catalyst in RBC) CO2 + H2O H2CO3 • Carbonic acid releases H+ protons (acid dissociation – chemistry) H2CO3 HCO3- + H+ • H+ lower blood pH and combine with Hb to make haemoglobinic acid decreasing Hb O2 affinity (Bohr) H+ + HB HHb HCO3- ions diffuse out of the erythrocyte. • • • Cl- diffuse into the cell to balance the charge CHLORIDE SHIFT TASK: Write equations for the following steps CO2 dissolves in water to form carbonic acid (via carbonic anhydrase catalyst in RBC) 2. Carbonic acid releases H+ protons (acid dissociation – chemistry) 3. H+ lower blood pH and combine with Hb to make haemoglobinic acid decreasing Hb O2 affinity (Bohr) 4. HCO3- ions diffuse out of the erythrocyte & Cldiffuse into the cell to balance the charge CHLORIDE SHIFT 1. EXT – Link these equations into a sequence (in a red blood cell so you can show what is & isn't inside the cell) CO2 CO2 + H2OH2CO3H+ + HCO3Carbonic anhydrase Conformational change Decreased affintiy for O2 We know that oxygen dissociates from oxyhaemoglobin where the pO2 is low (i.e. in respiring tissue). • If H+ ions can bind with Hb, they must compete with oxygen • In respiring tissue: - More CO2 produced - More Carbonic acid formed - More H+ dissociated - More competition for Hb - More oxygen dissociation Formation of hydrogen carbonate Build up of hydrogen carbonate ions causes them to diffuse out of RBC leaving inside of RBC positively charged. To balance electric charge Cl- ions diffuse into the RBC from plasma – this is known as the chloride shift. In this reaction Hb is acting as a buffer http://www.youtube.com/watch?feature=player_embedded&v=x26TWL3VKMg http://www.youtube.com/watch?feature=player_embedded&v=bklrcFuiH-8 Breakdown of hydrogen carbonate When blood gets to the lungs, all the reactions are reversed The hydrogen carbonate and hydrogen ions recombine releasing CO2 The chloride shift is reversed Carbamino-haemoglobin breaks down to release CO2 CO2 + H2OH2CO3H+ + HCO3H+ + HCO3- H2CO3 CO2 + H2O Transport of carbon dioxide In tissue : plasma CO2 + H2O enzyme H+ + HCO3-