ppt
advertisement

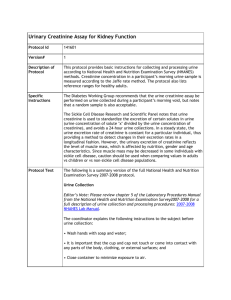
Chemical examination of urine, urinary sediment Pavla Balínová Kidney function • maintenance of ECF and ICF volume, osmolarity and pH of blood, electrolytes levels • elimination of wastes (urea, creatinine,…) Glomerular filtration, tubular resorption and secretion occur in nephron. Nephron as a functional unit of the kidney Figure was found at http://en.wikipedia.org/wiki/Renal_tubule#Renal_tubule Production of urine • glomerular filtration rate (GFR) is 2 mL of blood per one second = 120 mL/min → cca 160-180 liters of ultrafiltrate per day • an adult human produces 0.5 – 2.0 L of urine per day (in average 1.5 L) Composition of urine ● 95% of volume of normal urine is due to water Organic components: ● ● ● ● ● ● urea urobilinogen uric acid creatinine amino acids metabolites of hormones Inorganic components: ● ● cations: Na+, K+, Ca2+, NH4+ anions: Cl-, SO4 2-, HCO3-, HPO4- N-containing compounds in urine Urea is synthesized in the liver - it is transported by free diffusion through membrane Ammonia is released from Gln - buffer function in the urine Creatinine is a product of muscle metabolism -it is not reabsorbed by the tubules → creatinine clearance Uric acid is a final product of endogenous and dietary purine degradation Urobilinogen (UBG) is formed from bilirubin in a small intestine - can be oxidized to urobilin in urine N-containing compounds in urine creatinine uric acid Kidneys (and lungs) are the most important organs in maintenance of ABB Proximal tubule • reabsorption of HCO3- and secretion of H+ • enzyme carboanhydrase (CA) Distal tubule • H+ -ATPase catalyzes transport of H+ into lumen of distal tubule • aldosterone increases H+ secretion • H+ in urine: BUFFER – reacts with NH3 SYSTEMS – reacts with HPO42• urinary pH may range 4.5 – 8.0 Buffer systems in urine Kidneys in metabolism • tubular epithelia are the main metabolic active cells • ATP for active transports comes from aerobic oxidation of lactate, glutamine and FA • gluconeogenesis (Gln, lactate, glycerol, Fru) is an important source of Glc during starvation • kidneys take up glutamine from plasma ↓ glutaminase glutamate + NH3 URINE ↓ glutamate dehydrogenase 2-oxoglutarate + NH3 URINE ↓ citric acid cycle Note: glutaminase is located in the inner mitochondrial membrane and it is activated by cortisol and catecholamines. Determination of urine Physical determination: • volume, density, colour, smell, foam, pH Chemical determination: • ion composition: Na+, K+, Ca2+, Mg2+, Li+, Cl-, phosphates • N-containing metabolites: urea, creatinine, uric acid • proteins, glucose, ketone bodies, enzymes, hormones Functional test of kidney: • creatinine clearance Microscopic determination: • non-organ components (crystals of salts) and organ components (cells) Microbiological determination: ● apperance of bacteria, fungi or yeast Pathological components of urine • ↑ proteins → proteinuria (glomerulonephrititis, bacterial infection, pregnancy) • 150 mg of proteins are excreted daily ↑ glucose → glycosuria (diabetes mellitus, emotion stress) • renal threshold for Glc is around 10 mmol/L ● • ↑ ketone bodies → ketonuria (starvation, diabetes, pregnancy) • other pathological components: bilirubin, blood (ery, Hb),… Creatinine clearance test • is a useful measure for estimating the glomerular filtration rate (GFR) of the kidneys in mL/sec • is the volume of blood plasma (mL) that is cleared of creatinine per unit time (sec) Ccr (mL/s) = (cu/cs) x V/t cu = creatinine concentration in urine sample cs = creatinine concentration in serum sample V/t = urine flow (mL/s) Urinary sediment = microscopic examination of urine • examination of urinary sediment evaluates the presence and number of organ components – cells (ery, leu, epithelial cell, bacteria) and nonorgan components (crystals) • crystals are mostly composed of calcium oxalate or calcium phosphate • urate stones (from uric acid) - gout, acidic pH of urine oxalate crystals uric acid crystals Figures were assumed from http://mnof.cz/ sediment - Atlas močového sedimentu On-line