ACCESS PowerPoint template, updated 5/2007
advertisement
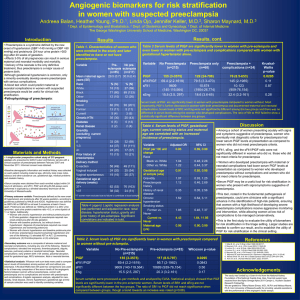
Screening and early detection of Preeclampsia Harshad Sanghvi Vice-President & Medical Director Jhpiego Africa meeting: Interventions For Impact in EONC Addis Ababa, 22 February 2011 Definitions Preeclampsia: Hypertension, proteinuria in pregnancy Mild: Diastolic 90-100, proteinuria1-2g/l Severe: diastolic 110+, proteinuria 3g/l Eclampsia: +convulsions 2 Why an additional Focus on PE/E Mortality associated with PE/E shows little decline in more than 75% of low resource countries Between 7-15% of pregnant women develop preeclampsia (high BP and proteinuria) Approximately 1-2% develop Eclampsia Contribute between 8-25% of maternal mortality Increased risk of perinatal mortality: PE : RR 1.7-3.7 E : RR 2.9-13.7 Nepal Maternal Mortality Study 1998 & 2009 1998 2009 MMR 539 247 PPH 37% 19% Eclampsia 14% 21% Source: Nepal maternal mortality study 2008-9 3 Prediction of Preeclampsia Risk factors not very useful: Primigravida are now about 50% of obstetric population ? A significant proportion of PE occurs postpartum No effective or affordable biochemical or biophysical predictor available Implication: All pregnant women potentially at risk need prevention or early detection of PE 4 Test No of studies No of women 2 BMI>34 8 BMI>29 9 BMI>24.2 7 BMI<19.8 12 AFP 2 Fibronectin cellular 3 Fibronectin total 3 Foetal DNA 16 HCG 3 Oestriol 5 Serum uric acid 4 Urinary calcium excretion Urinary calcium/creatinine ratio 6 4 Total proteinuria 2 Total albuminuria 2 Microalbuminuria 1 Microalbumin/creatinine ratio 1 Kallikreinuria 1 SDS Page proteinuria Doppler any/unilateral notching19 21 Doppler bilateral notching 8 Doppler other ratios 8 Doppler pulsatility index 29 Doppler resistance index Doppler combinations of FVW 25 16200 410823 440214 152720 137097 135 373 351 72732 26811 514 705 1345 2228 88 190 1422 307 153 14345 29331 2619 14697 7982 22896 Prediction of preeclampsia 0 20 40 60 Sensitivity 80 100 Sn (95% CI) Sp (95% CI) 18 (15 - 21) 23 (15 - 33) 41 (29 - 53) 11 (8 - 16) 9 (5 - 16) 50 (30 - 70) 65 (42 - 83) 50 (31 - 69) 24 (16 - 35) 26 (9 - 56) 36 (22 - 53) 57 (24 - 84) 50 (36 - 64) 35 (13 - 68) 70 (45 - 87) 62 (23 - 90) 19 (12 - 28) 83 (52 - 98) 100 (88 - 100) 63 (51 - 74) 48 (34 - 62) 55 (37 - 72) 48 (29 - 69) 66 (54 - 76) 64 (54 - 74) 93 (87 - 97) 88 (80 - 93) 75 (62 - 84) 80 (73 - 86) 96 (94 - 98) 96 (79 - 99) 94 (86 - 98) 88 (80 - 93) 89 (86 - 92) 82 (61 - 93) 83 (73 - 90) 74 (69 - 79) 80 (66 - 89) 89 (79 - 94) 89 (79 - 94) 68 (57 - 77) 75 (73 - 77) 98 (98 - 100) 69 (60 - 77) 82 (74 - 87) 92 (87 - 95) 80 (73 - 86) 87 (75 - 94) 80 (74 - 85) 86 (82 - 90) 0 20 40 60 80 Specificity Methods of prediction and prevention of pre-eclampsia: systematic reviews of accuracy and effectiveness literature with economic modelling CA Meads, et al 2008 100 Intervention No of RCTs No of women Ambulatory BP 0 0 Bed rest for high BP 1 228 0.98 (0.80, 1.20) Exercise 2 45 0.31 (0.01, 7.09) Rest alone for normal BP 1 32 0.05 (0.00, 0.83) Altered dietary salt 2 631 1.11 (0.46, 2.66) Antioxidants 7 6082 0.61 (0.50, 0.75) Calcium 12 15206 0.48 (0.33, 0.69) Nutritional advice 1 136 0.98 (0.42, 1.88) Balanced protein/energy intake 3 512 1.20 (0.77, 1.89) Isocaloric balanced protein supplementation 1 782 1.00 (0.57, 1.75) Energy/protein restriction 2 284 1.13 (0.59, 2.18) Garlic 1 100 0.78 (0.31, 1.93) Magnesium 2 474 0.87 (0.57, 1.32) Marine oils 4 1683 0.86 (0.59, 1.27) Antihypertensives v none 19 2402 0.99 (0.84, 1.18) Antiplatelets 43 33439 0.81 (0.75, 0.88) Diuretics 4 1391 0.68 (0.45, 1.03) Nitric oxide donors and precursors 4 170 0.83 (0.49, 1.41) Progesterone 1 128 0.21 (0.03, 1.77) Primary Prevention Of PE RR (95% CI) 0.01 0.1 0.2 0.5 1 2 5 10 Relative Risk (95% Confidence Interval) Cost per woman ( UK £ 2005) Comparing Cost and Effectiveness of Interventions for Preventing PE 500 450 400 350 300 250 200 150 100 50 0 No test, calcium to all 0.94 0.95 0.96 0.97 0.98 0.99 Effectiveness (proportion free of pre-eclampsia) Good Question: Are calcium supplements out of reach for low resource settings 7 Coverage of prenatal care: selected countries* At least 1 visit (%) 4+ visits (%) Kenya (2008-09) 91 47 Tanzania (2004-05) 97 62 Uganda (2006) 95 47 Zambia (2007) 97 60 Zimbabwe 94 71 (2004) 95 58 Nigeria (2008) 55 45 Ethiopia (2005) 28 12 Mozambique (2003) 84 53 Ghana (2008) 94 78 Rwanda 96 24 91 40 Malawi (2005-06) (2007-08) Senegal (2005) *Macro International, 2011. Measure DHS. Data representative of women who gave birth in the 5 years prior to the survey. 8 Massive unmet need for early detection of PE Source DHS Country % Unmet need for BP Check % Unmet need for Proteinuria Check Bangladesh 53.1% 70.5% Bolivia 24.5% 50.9% DRC 38.8% 57.8% India 52.5% 56.8% Indonesia 13.9% 63.0% Kenya 22.8% 38.9% Malawi 28.6% 81.3% Mozambique 48.7% 73.9% Nepal 43.8% 77.7% Zimbabwe 14.0% 39.8% 9 Detecting Preeclampsia Measuring BP: Significant training needed to do BP well Robust and maintained equipment • Aneroid BP machines require frequent recalibration Currently completely missing about 50% women who do not receive antenatal care, Also missing an additional 15-30% who attend ANC but do not have BP taken 10 Assessment of BP technology The absence of accurate, easily-obtainable, inexpensive devices for blood pressure measurement; The frequent marketing of non-validated blood pressure measuring devices; The relatively high cost of blood pressure devices given the limited resources available; Limited awareness of the problems associated with conventional blood pressure measurement techniques; A general lack of trained manpower and limited training of personnel. 11 How can we detect all the Preeclampsia before it becomes life threatening One approach: Take testing for hypertension and proteinuria to women in their homes rather than only depending on them reaching facilities Seeking simple, inexpensive and effective solutions that reach all pregnant women • • • • • Reliably detect diastolic BP > 90mmHg Low cost, low power, easy to manufacture ($5) For use by semi literate community workers Culturally compatible e.g. women in deeply conservative societies will not expose their upper arm for a typical blood pressure cuff. Robust in wide temperature ranges and in extreme dry and wet areas. Solution Modular Components • Manual inflatable pressure cuff applied to the wrist to restrict blood flow. • Self deflating cuff with digital pressure sensor to provide feedback to a microcontroller. This automates hypertension diagnosis set at 90 diastolic for community use devices • Hand Cranked generator with a super capacitor for power as well as batteries. • Binary LED panel to indicate sufficient power, inflation, and color codes for semi-literate volunteer to interpret. Procedure: Apply Cuff, Crank till Green LED light, inflate till LED yellow LED, wait as cuff automatically deflates, Red light and audible signal indicates hypertension Sanghvi, Lee, Jayaram, Trachtenberg, Acharya 13 Current Prototype Secondary Prevention: Detecting Preeclampsia Measuring Urine Protein Urine dipstick tests quite pricy: Test reagent is not what makes it pricy. Boiling not feasible in high-volume sites, not suitable for home testing Alternatives e.g., PATHstrips developed for clinic/lab setting dependant on central manufacture of test strips 15 Extremely Affordable Point of Care Diagnostics: Prototype Protein Test Sanghvi, Crocker, Mongale 16 Diagnostic Platform Reagent Solution Purpose Chemical Protein Indicator Tetrabromophenol Blue Acid Buffer Citric Acid, Sodium Citrate Liquid Vehicle Isopropyl Alcohol, DI H2O 17 Solution Reagent modified to yield sharp color change when there is 0.7g/l protein: The test strip prepared by marking an end of a piece of filter paper with the reagent. Use: Pregnant woman who is instructed to void urine on the test area of the strip and report if a color change from yellow to blue occurs. Blue Color indicates pathological proteinuria Sanghvi, Crocker, Mongale 18 Performance standards: Severe PE/E Performance standard Verification n criteria The provider correctly describes signs and symptoms of Severe PE and E 7 The provider describes correct management of Severe PE and E 12 The provider correctly describes follow up actions 12 Example of Verification criteria: Administer 4 gm of Magnesium Sulphate IV over 5 minutes ( 20 ml of 20% Magnesium Sulphate) 19 SBMR: Nepal Experience in improving quality of PEE care Intervention: 1 day on site whole facility orientation by NESOG Review of standards, practice of skills Baseline assessment, gap analysis, action plan Re-assess at 2, 4 months Baseline % facilities meeting standards 14% % facilities where no standard met 27% Average score 26% facility % reaching standard 87% 2 months 4 months 36% 59% SBA training sites 50% 0% Govt Hosp Private hospitals 17% Med school 38% PHCC 33% 0% 60% 63% 20 Achieving maximum impact of reducing mortality from PE: From Household to Hospital Predict preeclampsia •Risk factors not very useful: Primigravida are now about 50% of obstetric population and a significant proportion of PE occurs postpartum •No effective or affordable biochemical or biophysical predictor available Primary prevention √ Calcium, √ Aspirin Secondary Prevention •Detect Hypertension •Detect Proteinuria •Timely delivery •BP: Not available for women not reaching prenatal care (50%) : Missing an additional 15-30% who attend ANC but do not have BP taken •Protein test offered to less than 20%( SPA, 6 countries) Tertiary Prevention√ Magnesium Sulphate, Antihypertensives Urgent delivery 21