File - AMHOP
advertisement

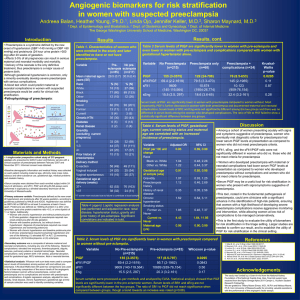
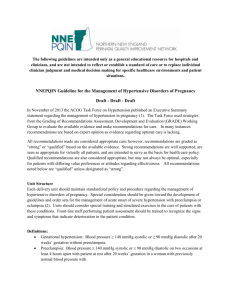
HYPERTENSIVE DISORDERS IN PREGNANCY Betha Fe Manaois-Castillo M.D. FPOGS,FPCS,FPSUOG 25 July 2013 HYPERTENSIVE DISORDERS • Most common medical complication in pregnancy • 5-10% incidence • Major cause of maternal and perinatal morbidity worldwide Report of the National High Blood Pressure Education Program. Working group report on high blood pressure. Am J Obstet Gynecol. 2000;183:S1.; Sibai BM. Diagnosis and management of gestational hypertension and preeclampsia. Obstet Gynecol. 2003; 102:181. HYPERTENSION • BP > 140 mm Hg systolic OR 90 mm Hg diastolic • Present on at least 2 occasions, at least 6 hours apart, but within a maximum of a 1week period Hypertensive Disorders Related To Pregnancy 1. 2. 3. 4. 5. 6. Gestational hypertension Preeclampsia Eclampsia HELLP syndrome Chronic/preexisting hypertension Preeclampsia superimposed upon chronic/preexisting hypertension Gestational Hypertension • systolic blood pressure ≥140 mHg and/or diastolic blood pressure ≥90 mmHg in a previously normotensive pregnant woman who is ≥20 weeks of gestation and has no proteinuria • BP returns to normal within 12 weeks after delivery Gestational HTN: DIAGNOSIS • Determine the severity of hypertension • Measure protein excretion • 24-hour urine collection • Evaluate for signs/symptoms of severe preeclampsia • Perform laboratory evaluation • +/- end - organ involvement Gestational HTN: DIAGNOSIS CRITERIA FOR MILD GESTATIONAL HYPERTENSION Blood Pressure > 140 to < 160 mm Hg, systolic > 90 to < 110 mm Hg, diastolic Proteinuria < 300 mg per 24-hr collection Platelet count > 100,000/mm3 Liver enzymes Normal Maternal symptoms Absent IUGR / Oligohydramnios (UTZ) Absent Gestational HTN: MANAGEMENT • Mild Gestational HTN • • • • • • • Managed as outpatients (weekly antepartum visits) Daily fetal movement/kick counting NST + AFI OR BPS Fetal growth monitoring every 3-4 weeks No antihypertensive therapy No antenatal corticosteroids Deliver patients no later than their EDD Gestational HTN: MANAGEMENT • Severe Gestational HTN • SBP ≥160 mmHg or DBP ≥105 mmHg is treated with antihypertensive agents • > 34 wks AOG DELIVER! • < 34 wks AOG give steroids Gestational HTN: Risk of Progression to Preeclampsia • 15-25% risk • Women with early onset of gestational hypertension are more likely to progress to preeclampsia than women with late onset Gestational HTN: RECURRENCE • Prevalence: 22 - 47 % (2nd pregnancy) • tends to recur with subsequent pregnancies Gestational HTN: LONG-TERM PROGNOSIS • associated with development of HTN later in life • associated with development of diseases related to hypertension (CVD, CKD,DM) PREECLAMPSIA • Is a multi - system disorder characterized by new onset of hypertension and proteinuria after 20 weeks of gestation in a previously normotensive woman • increased risk for maternal and/or fetal mortality or serious morbidity •Sibai BM, Caritis S, Hauth J, National Institute of Child Health and Human Development Maternal-Fetal Medicine Units Network. What we have learned about preeclampsia. Semin Perinatol 2003; 27:239.; Hutcheon JA, Lisonkova S, Joseph KS. Epidemiology of pre-eclampsia and the other hypertensive disorders of pregnancy. Best Pract Res Clin Obstet Gynaecol 2011; 25:391. www.uptodate.com ©2013 UpToDate® Preeclampsia “ A 2 – stage disease? “ 1. Asymptomatic Placental Stage 2. Symptomatic Maternal Stage Preeclampsia: PATHOGENESIS • • • • • • Immunologic Factors Systemic Endothelial Dysfunction Diet Genetic Factors Increased sensitivity to Angiotensin II Inflammation/Infection Preeclampsia: RISK FACTORS • Associated with the pregnant woman • • • • • • • • • • Nulliparity Preeclampsia in a previous pregnancy Age >40 years or <18 years Family history of preeclampsia (mother or sister) Chronic hypertension Chronic renal disease; APAS or inherited thrombophilia; Vascular or connective tissue disease; DM (pregestational and gestational) High body mass index Black race / Filipino Woman herself was small for gestational age Prolonged interpregnancy interval Preeclampsia: RISK FACTORS • Associated with the pregnant woman’s husband or partner • First time father • Male partner whose mother or previous partner had preeclampsia • Partner related factors (new partner, limited sperm exposure [eg, previous use of barrier contraception]) Preeclampsia: RISK FACTORS • Associated with the fetus • • • • Multifetal gestation Hydrops fetalis / Triploidy Unexplained fetal growth restriction Fetal growth restriction, abruptio placentae, or fetal demise in a previous pregnancy • Hydatidiform mole MEAN ARTERIAL PRESSURE MAP = DBP + 1/3 (SBPDBP) ● MAP – 2 > 90 mmHg or a MAP3> 105 mmHg increased PIH and perinatal deaths ● Absence of a mid – trimester drop in BP may predict future PIH based on the absence of arteriolar vasodilatation Early Screening for PE (11-13 weeks) • Ultrasound Screening • Uterine arteries (PI) • Abnormal UA can identify 50% of those who will develop preeclampsia and 30% of those who will develop IUGR. Nicolaides, Placental and Fetal Doppler, Diploma in Fetal Medicine Series, 2000. • Maternal Serum Markers • VEGF, PlGF, sFlt1 • Endoglin Courtesy of WWS Clinical Features and Pathophysiology • Cardiopulmonary • Hypertension • Intravascular volume and edema • Cardiac function - high afterload assoc w/ inc. cardiac filling pressures • Pulmonary edema – pulmo vascular hydrostatic P > plasma oncotic P – Capillary leak, left HF, iatrogenic volume overload Clinical Features and Pathophysiology • Renal • Proteinuria – ≥0.3 grams protein in a 24-hour urine specimen or persistent 1+ (30 mg/dL) on dipstick – random protein:creatinine ratio >30 mg/mmol – ≥5 grams of protein in a 24-hour urine collection (SEVERE) • Renal Function – GFR (30-40%), renal plasma flow – Rising creatinine and oliguria (UO<500mL/24h) PES (sec to renal vasoconstriction and Na retention) Clinical Features and Pathophysiology • Renal • Hyperuricemia / Hypocalciuria – inc proximal Na resorption; urate reabsorption sec to renal ischemia • Urine sediment – benign • Histology – Glomerular Endotheliosis Light micrograph in preeclampsia showing glomerular endotheliosis. The primary changes are swelling of damaged endothelial cells, leading to partial closure of many of the capillary lumens (large arrows). Mitosis within an endothelial cell (small arrow) is a sign of cellular repair. Courtesy of Helmut Rennke, MD. Clinical Features and Pathophysiology • Hematologic • Thrombocytopenia – – • PT, aPTT, Fibrinogen – • accelerated plt consumption <100,000/uL PES not affected Microangiopathic hemolysis – – + schistocytes / helmet cells (PBS) Inc LDH; hemoconcentration Clinical Features and Pathophysiology • Hepatic • Periportal and sinusoidal fibrin deposition and microvesicular fat deposition • RUQ pain, inc transaminase levels, coagulopathy, subcapsular hemorrhage or hepatic rupture • Epigastric pain sec to stretching of Glisson’s capsule due to hepatic swelling or bleeding Clinical Features and Pathophysiology • CNS and eye • headache • visual symptoms – constriction of retinal arteries » Photopsia (flashing lights); scotomata (dark areas/gaps); diplopia or amaurosis fugax (unilat blindness) • generalized hyperreflexia • sustained ankle clonus • Stroke Clinical Features and Pathophysiology • Fetus and placenta • FGR • Oligohydramnios • Fetal hydrops (mirror or Ballantyne syndrome) PE: MANAGEMENT • Definitive treatment: DELIVERY! • Based on the ff: • AOG • Severity of PE • Maternal / Fetal condition PES: MANAGEMENT • Deliver regardless of gestational age • if proteinuria ( ≥5 grams) is the only criteria for severe diseasemanaged as mild PE • mild fetal growth restriction with reassuring Doppler velocimetry treat conservatively * • severe hypertension treat conservatively * NOTE: * remote from term MILD PE: MANAGEMENT • Deliver at ≥37 weeks of gestation • Labor induction encouraged EXPECTANT ANTEPARTUM MANAGEMENT OF MILD PREECLAMPSIA • Inpatient vs outpatient care • Close maternal monitoring upon diagnosis of preeclampsia is important to establish disease severity and the rate of progression • Hospitalization is useful for making these assessments and facilitates rapid intervention in the event of rapid progression • Outpatient care is a cost-effective option for women with stable mild preeclampsia after initial dx evaluation EXPECTANT ANTEPARTUM MANAGEMENT OF MILD PREECLAMPSIA • Laboratory follow – up • platelet count, serum creatinine, serum AST » 1-2x/wk, assess disease progression • Assessment of fetal well-being • • • • daily fetal movement count twice weekly fetal NST with AFI or twice weekly BPS UMA Doppler indices evaluation EXPECTANT ANTEPARTUM MANAGEMENT OF MILD PREECLAMPSIA • Assessment of fetal growth • sonographic estimation of fetal weight done to look for growth restriction and oligohydramnios at the time of diagnosis of PE , repeated every 3 weeks if the initial examination is normal • Antenatal corticosteroids • < 34 weeks AOG INTRAPARTUM MANAGEMENT • Intrapartum monitoring • Fluids • monitored closely to avoid excessive administration, since women with severe disease are at risk of pulmonary edema and significant third-spacing Acute Management of PES • Labetalol • first-line therapy (rapid onset of action, good safety profile) • 20 mg IV over 2 minutes followed at 10-minute intervals by doses of 20 to 80 mg – up to a maximum total cumulative dose of 300 mg – E.g. Give 20 mg, then 40 mg, then 80 mg, then 80 mg, then 80 mg Acute Management of PES • Hydralazine • 5 mg IV over 1 to 2 minutes • if BP goal is not achieved within 20 minutes, give a 5 to 10 mg bolus depending upon the initial response » The maximum bolus dose is 20 mg » If a total dose of 30 mg does not achieve optimal blood pressure control, another agent should be used. » The fall in blood pressure begins within 10 to 30 minutes and lasts from 2 to 4 hours. Target BP • 130 to 150 mm Hg systolic and 80 to 100 mm Hg diastolic OR reduce MAP by no more than 25% over 2hrs • Cerebral or myocardial ischemia or infarction can be induced by aggressive antihypertensive therapy if the blood pressure falls below the range at which tissue perfusion can be maintained by autoregulation • Seizure Prophylaxis • MgS04 given to mild / severe PE » Loading dose: 4-6 g, slow IV push, over 15-20 mins » Continuous infusion: 1-2 g/hr OR 5g IM into each buttock (total 10 g) followed by 5 g IM, alternate buttocks ever 4h • continued for 24 hours postpartum MgS04 Toxicity • loss of DTRs: 9.6 to 12.0mg/dL(4.0 -5.0 mmol/L) • respiratory paralysis: 12.0 to 18.0 mg/dL (5-7.5 mmol/L) • cardiac arrest: 24 to 30 mg/dL (10 to 12.5 mmol/L) * Calcium gluconate (1 gram intravenously over 5 to 10 minutes) • should be administered only to counteract life-threatening symptoms of magnesium toxicity (such as cardiorespiratory compromise) Postpartum Management • NSAIDs • for pain control should be avoided in women with poorly controlled hypertension, oliguria, renal insufficiency, or thrombocytopenia • Monitor VS q 2h while on MgS04 • Treat PES Prevention of Recurrence • Prepregnancy • Weight loss to ideal BMI • Control of glucose in diabetes • Control of BP in CHTN (diet, exercise) • Low dose aspirin in select patients (from 12 wks) • Not recommended • Vitamins C & E • Dietary salt restriction • Anti-HTN therapy to prevent preeclampsia ECLAMPSIA • development of grand mal seizures in a woman with preeclampsia, in the absence of other neurologic conditions that could account for the seizure • occurs in 2 to 3 percent of severely preeclamptic women not receiving antiseizure prophylaxis Pathogenesis of Seizures 1. Cerebral overregulation in response to high systemic blood pressure • • • • vasospasm of cerebral arteries underperfusion of the brain localizedischemia/infarction cytotoxic (intracellular) edema Pathogenesis of Seizures 2. Loss of autoregulation of cerebral blood flow in response to high systemic pressure • • • • E.g., hypertensive encephalopathy Hyperperfusion endothelial damage vasogenic (extracellular) edema Management • Iinitial Mx: Maintenance of airway patency and prevention of aspiration • Gravida rolled onto her left side • Protect from trauma • Supplemental O2 (8-10L/min via face mask) • Management of severe hypertension, if present • Prevention of recurrent seizures • Evaluation for prompt delivery • definitive treatment of eclampsia is delivery, irrespective of gestational age Management of Persistent Convulsions • additional bolus of 2 grams MgS04 over 15 to 20 minutes • with careful monitoring for signs of magnesium toxicity HELLP Syndrome • Hemolysis • Elevated Liver enzymes • Low Platelets • severe form of preeclampsia or an independent D/O HELLP Syndrome Initiate IV Dexamethasone EARLY: • Always when PLTS <100,000/uL • Selectively when Class 3 plus – (a) Eclampsia; (b) Severe Epigastric Pain; (c) Fulminant Disease; (d) Severe HTN • Antepartum: Dex 10mg q12 hrs • Postpartum: Dex 10+10+5+5 @ 0,12,24,36 hrs CHRONIC / PREEXISTING HYPERTENSION • SBP ≥140 mmHg and/or DBP ≥90 mmHg that antedates pregnancy or is present before the 20th week of pregnancy (on at least two occasions) or persists longer than 12 weeks postpartum PREECLAMPSIA SUPERIMPOSED UPON CHRONIC / PREEXISTING HYPERTENSION • the new onset of proteinuria after 20 weeks of gestation in a woman with chronic/preexisting hypertension • Hypertensive Disorders particularly PREECLAMPSIA… • Major life-threatening morbidity • Leading reason for preterm labor and birth • RISK factor for FUTURE maternal cardiovascular and metabolic DISEASE • Affects long term maternal survival GOALS • Development of effective strategies for the prevention and/or treatment of preeclampsia • Prolong the pregnancy and improve maternal and neonatal health Key Points • • • • • • • Identify Risk Factors Prediction Diagnosis (Classify) Ambulatory or In Patient Management Tertiary Care Postpartum care Prevention Thank you…