Document
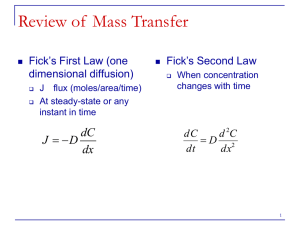
advertisement

IMPLANTABLE CONTROLLED DRUG DELIVERY SYSTEMS Implants are very small pellets composed of drug substance only without excipients. They are normally about 2-3 mm in diameter and are prepared in an aseptic manner to be sterile. Implants are inserted into a superficial plane beneath the skin of the upper arm by surgical procedures, where they are very slowly absorbed over a period of time. Implant pellets are used for the administration of hormones such as testosterone. The capsules may be removed by surgical procedures at the end of the treatment period. Biocompatibility need to be investigated, such as the formation of a fibrous capsule around the implant and, in the case of erosion-based devices there is the possible toxicity or immunogenicity of the byproducts of polymer degradation. The Implantable controlled drug delivery system achieved with two major challenges. 1) by sustained zero-order release of a therapeutic agent over a prolonged period of time. This goal has been met by a wide range of techniques, including: Osmotically driven pumps Matrices with controllable swelling diffusion or erosion rates 2) By the controlled delivery of drugs in a pulsatile or activation fashion. These systems alter their rate of drug delivery in response to stimuli including the presence or absence of a specific molecule, magnetic fields, ultrasound, electric fields, temperature, light, and mechanical forces. Such systems are suitable for release of therapeutics in non-constant plasma concentrations as in diabetes. This goal has been met by two different methodologies: A delivery system that releases the drug at a predetermined time or in pulses of a predetermined sequence. A system that can respond to changes in the local environment. IMPLANTABLE CONTROLLED DRUG DELIVERY SYSTEMS IN A PULSATILE FASHION Theoretical pulsatile release from a triggered-system . IMPLANTABLE CONTROLLED DRUG DELIVERY SYSTEMS IN A SUSTAINED ZERO-ORDER CONTINUOUS RELEASE In membrane permeation-type controlled drug delivery, the drug is encapsulated within a compartment that is enclosed by a rate-limiting polymeric membrane. The drug reservoir may contain either drug particles or a dispersion of solid drug in a liquid or a solid type dispersing medium. The polymeric membrane may be made-up from a homogeneous or a heterogeneous nonporous polymeric material or a microporous or semipermeable membrane. The drug release by diffusion (dQ/dt) from this type of implantable therapeutic systems should be constant and defined by: Where: dQ = dt CR 1 1 Pm Pd CR is the drug concentration in the reservoir compartment and Pm are the permeability coefficients of the rate-controlling membrane Pd the permeability coefficients of the diffusion layer existing on the surface of the membrane, respectively. Pm and Pd depend on the partition coefficients for the interfacial partitioning of drug molecules from the reservoir to the membrane and from the membrane to the aqueous diffusion layer, respectively. Example Levonorgestrel Implants These are a set of six flexible, closed capsules of a dimethylsiloxane/methylvinylsiloxane copolymer, each containing 36 mg of the progestin levonorgestrel. They are inserted through a 2 mm incision in the mid- portion of the upper arm in a fan-like pattern. This system provides long-term (up to 5 years) reversible contraception. Diffusion of the levonorgestrel through the wall of each capsule provides a continuous low dose of progestin. Pre-programmed Delivery Systems A technique that depend on sequential release of drugs which fabricated as polymer matrix with multilayer alternating drug-containing and spacer layers. The polymer matrix is commonly surrounding impermeable shell, which permitting release of the entrapped drug only after degradation of this polymer matrix. For degradation of this polymer matrix to occur, the polymer matrix must be susceptible to hydrolysis or biodegradation by a component in the surrounding media. )A) Schematic of a multilayered pulsatile delivery system with one face exposed to the local environment. (B) Schematic of a cylindrical multilayered delivery system with two open faces. I.System that controlling drug release by environmental pH Using polyanhydrides as the spacer layers and the drug containing layer as poly[(ethyl glycinate)(benzly amino acethydroxamate)phosphazene] (PEBP) The polyanhydrides and PEBP layers were compression molded to form a multilayered cylindrical core, which was then coated with a poly(lactide-co-1,3-trimethylene carbonate) film over all surfaces except for one face of the device. The hydrolysis of PEBP is highly dependent on the pH of the surrounding media, dissolving much more rapidly (1.5 days) under neutral and basic conditions (pH 7.4) but in acidic conditions (pH 5.0) digradad over 20 days. The degradation products of polyanhydrides create an acidic environment within the delivery device, preventing the rapid hydrolysis of the PEBP and result in slow drug release until all of the polyanhydride layer has been eroded. II. System that controlling drug release by environmental enzymes Using hydrogels that have differing susceptibilities to enzymatic degradation. Pulsatile release can be achieved with a model system that uses the enzymatic degradation of dextran by dextranase to release insulin in a controlled manner. A delivery vehicle can be fabricated by covering poly(ethylene glycol)-grafted (embedded) dextran (PEG-gDex) and unmodified dextran layers in a silicone tube. The drug is loaded into the PEG-g-Dex layers while dextran is material for the spacer layer. The introduction of PEG into a dextran solution containing a drug causes the formation of a two-phase polymer when the dextran is cross-linked. The drug is partitioned into the PEG phase, resulting in drug release that is erosion-limited instead of diffusionlimited. Closed-loop delivery systems Closed-loop delivery systems are those that are selfregulating. They are similar to the programmed delivery devices in that they do not depend on an external signal to initiate drug delivery. However, they are not restricted to releasing their contents at predetermined times. Instead, they respond to changes in the local environment, such as the presence or absence of a specific molecule. Glucose-Sensitive Systems Several strategies are used for glucose-responsive drug delivery. 1. pH Dependent systems for glucose-stimulated drug delivery 2. Competitive binding 1. pH Dependent systems for glucose-stimulated drug delivery As insulin is more soluble under acidic conditions, Incorporating glucose oxidase into a pH-responsive polymeric hydrogel enclosing insulin solution will result in a decrease in the pH of the environment immediately surrounding the polymeric hydrogel in the presence of glucose as a result of the enzymatic conversion of glucose to gluconic acid. )A) Diagram of a glucose-sensitive dual-membrane system. (B) The membrane bordering the release media responds to increased glucose levels by increasing the permeability of the membrane bordering the insulin reservoir . A copolymer of ethylene vinyl acetate (EVAc) containing g glucose oxidase immobilized on cross-linked poly- acrylamide. and insulin solution . the insulin release rate will be altered in response to changes in the local glucose concentration. The release rate of insulin returned to a baseline level when the glucose was remove. A dual-membrane system sensing membrane is placed in contact with the release media, while a PH barrier membrane is positioned between the sensing membrane and the insulin reservoir. As glucose diffuses into the hydrogel , glucose oxidase catalyzes its transport to gluconic acid, thereby lowering the pH in the microenvironment of the PH membrane and causing swelling . Gluconic acid is formed by the interaction of glucose and glucose oxidase, causing the tertiary amine groups in the PHmembrane to protonated and induce a swelling response in the membrane. Insulin in the reservoir is able to diffuse across the swollen barrier membrane. Decreasing the glucose concentration allows the pH of barrier membrane to increase, returning it to a more collapsed and impermeable state . 2. Competitive binding methodology depending on the fact that concanavalin A (Con A) a glucose-binding lectin, can bind both glycosylated insulin and glucose. Glycosylated insulin (G-insulin) bound to Con A can be displaced by glucose, thus release the drug from system. In this systems immobilized Con A -Glycosylated insulin encapsulated with a polymer (sepharose beads ) , release only occurs at sufficiently high glucose concentration . as Con A immobilized has a lower binding affinity for glucose than for G-insulin, preventing release at low glucose levels. Hydrogels formed by mixing Con A and (G-insulin) with copolymers as acrylamide . hydrogel will undergo a reversible gel–sol phase transition in the presence of free glucose due to competitive binding between the free glucose and Con A. G-insulin acts as a cross-linker for the Con A chains due to the presence of four glucose-binding sites on the molecule, but competitive binding with glucose disrupts these cross-links, making the material more permeable and thus increasing the rate of drug delivery. Sol–gel phase transition in polymers crosslinked with Con A. Similar systems have been developed that use the interaction between an antibody and an antigen to control the release of a drug in the presence or absence of the antigen. A hydrogel held together by the interaction of polymerbound antigen to polymer-bound antibody will swell in the presence of free antigen due to the competitive binding of bound antibody to free antigen, reducing the number of crosslinks in the hydrogel and thus increasing the rate of drug delivery in proportion to the antigen concentration. Open-loop Delivery Systems Open-loop delivery systems are not self-regulating, but require externally generated environmental changes to initiate drug delivery. These can include magnetic fields, ultrasound, electric fields, temperature, light, and mechanical forces. Open-loop delivery systems may be coupled to biosensors to obtain systems that automatically initiate drug release in response to the measured physiological demand. 1. Magnetic Field One of the first methodologies to achieve an externally controlled drug delivery system is the use of an magnetic field to adjust the rates of drug delivery from a polymer matrix. A magnetic steel beads embedded in an EVAc copolymer matrix that is loaded with the drug. An oscillating magnetic field ranging from 0.5 to 1000 gauss cause increased rates of drug release. The rate of release could be altered by changing the amplitude and frequency of the magnetic field. The increased release rate was caused by mechanical deformation due to magnetic movement within the matrix. During exposure to the magnetic field, the beads oscillate (swing) within the matrix, creating compressive and tensile forces which acts as a pump to (squeezing) push an increased amount of the drug molecule out of the matrix. 2. Ultrasound Ultrasound stimulus can be used to adjust drug delivery by directing the waves at a polymer or hydrogel matrix. Where drug release can be increased 27-fold from an EVAc matrix during exposure to ultrasound. Increasing the strength of the ultrasound resulted in a increase in the amount of drug released (1 W/cm for 30 min). The principle depends on that sound cavitation occurred by ultrasonic irradiation at a polymer–liquid interface forms high-velocity jets of liquid directed at the polymer surface that are strong enough to release away material at the surface of the polymer device, causing an increase in the erosion rate of the polymer. Also the sound cavitation enhances mass transport at a liquid–surface interface. Electric Field Electric current signal can be used to activate drug delivery. The presence of an electric current can change the local pH which initiate the erosion of pH-sensitive polymer and the release of the drug contained in polymer matrix. Polymers as poly(methacrylic acid) or poly(acrylic acid) can be dissolved at pH>5.4 A 5 mA electric current resulted in drug delivery due to the production of hydroxyl ions at the cathode, which raised the local pH, disrupting the hydrogen bonding between the comonomers. In the absence of the electric stimulus, drug release was negligible. Humans can tolerate direct current densities of under 0.5 mA/cm for up to 10 min; therefore no visible skin damage was observed. Temperature Thermally-responsive hydrogels and membranes can be used for pulsatile delivery of drugs. Temperature sensitive hydrogels have a lower critical solution temperature (LCST), a temperature at which a hydrogel polymer undergo a phase change. In which transition of extended coil to the uncross-linked polymer an can be occurred . This phase change is based on interactions between the polymer and the water surrounding the polymer. Thermally sensitive hydrogel systems can exhibit both negative controlled release, in which drug delivery is stoped at temperatures above the LCST, and positive controlled drug delivery, in which the release rate of a drug increases at temperatures above the LCST . N-Isopropylacrylamide (NIPAAm) is a commonly used thermosensitive polymer with an LCST of 32 °C. Thermally sensitive materials exhibiting negative thermally controlled drug delivery. When the temperature of the hydrogel is held below its LCST, the most thermodynamically stable configuration for the free (non-bulk) water molecules is to remain clustered around the hydrophobic polymer. When the temperature is increased over the LCST, the collapse of the hydrogel is initiated by the movement of the clustered water from around the polymer into bulk solution. Once the water molecules are removed from the polymer, it collapses on itself in order to reduce the exposure of the hydrophobic domains to the bulk water. Thermally sensitive materials exhibiting positive thermally controlled drug delivery. A copolymer of NIPAAm and acrylamide (AAm) is an example of such a material. The hydrophilic AAm increases the LCST of the copolymer as well as reducing the thickness and density of the outer layer formed when the temperature of the hydrogel is raised above its LCST. Upon collapse, the hydrogel will push out soluble drug held within the polymer matrix 5. Light The interaction between light and a material can be used to adjust drug delivery. This can be accomplished by combining a material that absorbs light at a desired wavelength and a material that uses energy from the absorbed light to adjust drug delivery. Near-infrared light has been used to adapt the release of drugs from a composite material fabricated from gold nanoparticles and poly(NIPAAm-co-AAm) When exposed to near-infrared light, the nanoshells absorb the light and convert it to heat, raising the temperature of the composite hydrogel above its LCST (40 °C(. This in turn initiates the thermoresponsive collapse of the hydrogel, resulting in an increased rate of release of soluble drug held within the polymer matrix . 6. Mechanical force Drug delivery can also be initiated by the mechanical stimulation of an implant. Alginate hydrogels can release included drugs in response to compressive forces of varying strain amplitudes. Free drug that is held within the polymer matrix is released during compression; once the strain is removed the hydrogel returns to its initial volume. This concept is similar to squeezing the drug out of a sponge.