Drug metabolism and pharmacogenetics
advertisement

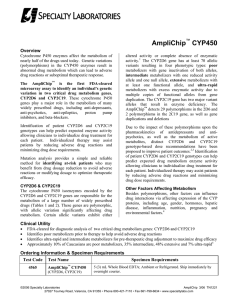
Drug/xenobiotic metabolism and pharmacogenetics George Howell III, Ph.D Sites of drug metabolism • Liver – responsible for the majority of drug metabolism – First pass metabolism • • • • • Kidney GI Lung Skin Brain Drug metabolism and its effects • Drug metabolism – the processes by which biochemical reactions alters drugs within the body • 4 ways a drug can be altered: 1. Active drug can be inactivated 2. Active drug can be converted to an active metabolite or toxic metabolite 3. Prodrug can be converted to an active drug 4. Unexcretable drug can be converted to an excretable metabolite Major types of biotransformation reactions • Oxidation/reduction reactions (Phase I) – – – – • Typically transform drug into more hydrophilic metabolites by adding or exposing a polar functional group Catabolic Can be more reactive and toxic than the parent compound Can be excreted is sufficiently polar Conjugation/hydrolysis reactions (Phase II) – – – Further modifications to compounds to improve hydrophilicity Anabolic Conjugate drug with an endogenous substrate such as glucuronic acid, sulfuric acid, acetic acid, or an amino acid to form a highly polar compound Oxidation/reduction reactions (Phase I) • More than 95% of oxidative biotransformations are performed by the cytochrome P450 monoxygenases • ~75% of all drugs currently used are oxidized by the P450s • Cytochrome P450 enzymes – Broad substrate specificity – Metabolize xenobiotics – Can play a role in formation of endogenous substances (steroid production) • Alcohol/aldehyde dehydrogenases • Monoamine oxidase • Esterases – Acetylcholinesterase (AchE) – Butylcholinesterase (BchE) – Carboxylesterase (CES) Percentage of total liver P450 content CYP3A4 = 30% CYP2C9 = 20% CYP1A2 = 15% CYP2E1 = 10% CYP2D6 = 5% CYP2A6 = 4% CYP2B6 = 1% Cytochrome P450s • Located within the endoplasmic reticulum • 74 CYP gene families • Three main ones involved in drug metabolism in the liver – CYP1, CYP2, CYP3 – ~50% of all rx drugs metabolized by CYP3A4 • P450 3A4 (CYP3A4) – 3 = number of the enzyme family – A = letter of the subfamily – 4 = specifies specific enzyme • Broad substrate specificity due in part to the activated oxygen of the complex (powerful oxidizing agent that can easily react) • Can be induced or inhibited by a variety of compounds – Leads to significant drug interactions ~50% P450 cycle Drug + O2 + NADPH + H+ Microsomal drug oxidations require: 1. P450 2. P450 reductase 3. NADPH 4. Molecular oxygen Steps of P450 mediated oxidation: 1. Oxidized P450 binds with drug to form a complex 2. P450 reductase reduces the P450/drug complex 3. P450 reductase reduces molecular oxygen to form an “activated oxygen”-P450/drug complex 4. Activated oxygen is transferred to drug to form oxidized product 5. One molecule of water is produced Drug-OH + H2O + NADP+ Electron donated Fe3+ reduced to Fe2+ P450 substrates, inducers, and inhibitors • P450 induction – Increase expression by increased synthesis or decreased degradation – Results in increased metabolism of substrates • Decreased substrate plasma concentrations • P450 inhibition – Decrease enzyme activity – Decrease rate of metabolism of other substrates • Increase substrate plasma concentrations Conjugation/hydrolysis reactions (Phase II) • Glucuronidation (highest % of drug metabolism of phase II) – Addition of UDP glucuronic acid catalyzed by UDP glucuronosyltransferase (UGT) • Acetylation – Addition of acetate by N-acetyltransferase (NAT) • Glutathione conjugation – Addition of glutathione by glutathione-Stransferase (GST) • Glycine conjugation – Addition of glycine by Acyl-CoA glycinetransferase • Sulfation – Addition of a sulfate by sulfotransferase (SULT) • Methylation – Addition of a methyl group by transmethylases • Water conjugation – Addition of water by epoxide hydrolase Conjugation reactions Factors affecting drug metabolism • Genetic variability (pharmacogenomics) – Certain populations have polymorphisms or mutations in metabolic enzymes with make them rapid or poor metabolizers • Race and ethnicity – Polymorphisms in metabolic genes among races • CYP2D6 polymorphisms among races • Age – Many biotransformations are slowed in young and elderly – Neonates can carry out most but not all oxidative reactions • Enzyme systems mature over the first two weeks and through childhood – Neonates can have decreased conjugating ability • Jaundice as a result of deficient bilirubin conjugation by UGT • Gray baby syndrome – decreased conjugation of chloramphenicol metabolite • Gender – Males metabolize ethanol, propranolol, some benzodiazepines, estrogens, and salicylates more rapidly Factors affecting drug metabolism (cont.) • Diet – Chargrilled foods and cruciferous vegetables induce CYP1A enzymes – Grapefruit juice inhibits CYP3A • Environment – Cigarette smoke induces P450 enzymes via Ahr dependent mechanism – Industrial workers exposed to some pesticides metabolize more rapidly • Drug interactions – See tables 4-5 and 4-6 in Lange for known inducers and inhibitors • Disease – Liver diseases (hepatitis, cirrhosis, cancer, hemochromatosis, fatty liver) can impair P450 activity – Cardiac disease can slow blood flow to liver and therefore decrease metabolism – Thyroid disease • Hyperthyroid – increase metabolism • Hypothyroid – decrease metabolism Acetaminophen toxicity •Normally undergoes glucuronidation and/or sulfation •Remaining drug undergoes P450 mediated metabolism •Excess acetaminophen saturates conjugation pathways…..shunts to P450 mediated metabolism •Role of ethanol •Hepatic glutathione (GSH) is depleted faster than is regenerated and Nacetylbenzoiminoquinone (toxic metabolite that reacts with proteins) accumulates •N-acetylcysteine is administered w/I 8-16 hours to protect from hepatotoxicity Pharmacogenetics How genetic variability affects drug metabolism GENETIC POLYMORPHISMS • Major factor accounting for differences in pharmacokinetic and pharmacodynamic parameters of individuals • Approximately 25 polymorphisms identified • Clinically important – – – – – N-acetylation debrisoquine/sparteine hydroxylation mephenytoin oxidation aldehyde oxidation butyrylcholinesterase (BchE) deficiency HYDROXYLATION POLYMORPHISMS • Debrisoquine (old antihypertensive) – CYP2D6 – 5-10% most populations are poor metabolizers (12% Chinese, Japanese) – Predominant enzyme for amines with hydrophobic planer unit – Approximately 15 variants of CYP2D6 • 4 - no activity, 5 - reduced activity, 3 - increased activity, 2 - no effect • Variation of 1000 fold can be found in extensive metabolizers (heterozygous, allelic variants) IMPACT of DEFICIENT CYP2D6 • Debrisoquine – single dose – Primary effect on first pass metabolism – Little change in ½ life – Increased peak plasma concentration (Clinical effects) • Sparteine – single dose – Primary effect – increased ½ life – No appreciable change in peak plasma concentration – (no observable clinical effects) GENETIC POLYMORPHISMS • S-mephenytoin hydroxylation – CYP2C19 Caucasians (3%) Orientals (15-20%) • Results in poor metabolizer phenotype • Substrates – Acids, bases or neutral compounds • Diazepam, imipramine, propranolol • Proguanil (antimalarial) activated by CYP2C19 12th Edition of Basic and Clinical has a more extensive table…….look up metabolizer phenotype for the prevalent polymorphisms (can be inferred from clinical consequence) N-ACETYLATION • Incidence – slow acetylators – 90% Moroccans, 5% Canadian Eskimos, 30-67% Caucasians and persons from African – Slow acetylators • Phenytoin-isoniazid inhibition of CYP450 • Arylamine – induced bladder cancer – benzidine – Rapid acetylators • Drug ineffective – dose must be increased • Hepatitis (insignificant) N-ACETYLATION • N-acetylation – Slow acetylators • Isoniazid- induced peripheral polyneuropathy • Drug - induced lupus erythematosus – 35 drugs with primary amino group ALDEHYDE DEHYDROGENASE – About 50% of people of Oriental descent are slow metabolizers of acetaldehyde – Rare outside the Oriental population • Significant acetaldehyde build up associated with ethanol intake – flushing, increased heart rate, nausea Butyrylcholinesterase deficiency • Autosomal recessive • Succinylcholine is metabolized by BchE • Increased accumulation of succinylcholine (depolarizing neuromuscular blocker) • Increased muscle paralysis including respiratory paralysis (succinylcholine apnea)