M. pneumoniae
advertisement

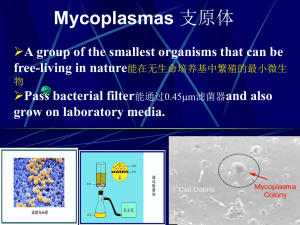
Mycoplasmas Mycoplasmas A group of the smallest organisms that can be free-living in nature, Pass bacterial filter and also grow on laboratory media. More than 80 species, belong to Mycoplasmatales of Mollicute. 3 families can be divided: Mycoplasmataceae (require external cholesterol during growth, contain Mycoplasma and Ureplasma two genera); Acholeplasmataceae (need not external cholesterol during growth); Spiroplasmataceae (can form spiral structure). ORGANISM Genus: Mycoplasma, Ureaplasma Species: M. pneumoniae: Upper respiratory tract disease, tracheobronchitis, atypical pneumonia M. hominis: Pyelonephritis, pelvic inflammatory disease, postpartum fever M. genitalium: Nongonococcl urethritis M.penetraus, U. urealyticum: Nongonococcl urethritis Morphology The smallest among prokaryotic microganisms with circular dsDNA, usually 0.2-0.3um in size; lack of cell wall; Pleomorphic, spherical, short rod, filament; Gram negative, but stained hardly, usually use Giemsa stain. Morphology They can assume multiple shapes including round, pear shaped and even filamentous. "fried egg" colonial morphology. BIOLOGICAL FEATURES Motility: Motile by possible release and reattachment of terminal cell organelle; no flagella present; possess a protein attachment factor termed P1 that interacts with a specific cellular receptor and allows adherence to respiratory epithelium. Respiration-Fermentation: Aerobes-anaerobes. Culture Most aerobic; require 10%-20% human or animal serum added to basic nutrient media except Acholeplasma; typical colony show fried egg apperance. Many species are part of the normal flora These organisms are a frequent cell culture contaminant The organisms have limited biosynthetic abilities; they require cholesterol for their cell membrane and can generate energy via the breakdown of arginine Ureaplasma requires urea to produce an electrochemical gradient; urea is converted to ammonia to produce ATP. GENETICS These bacteria have the smallest genome of any prokaryote ( about 20% that of E. coli) and the lowest G C content (about 24%). Resistance Sensitive to osmotic presssure resistant to thallium acetate醋酸亚 铊 in a concentration of 1:10000 which can inhibit bacteria Transmission M. pneumoniae is spread by close contact via aerosolized droplets and thus is most easily spread in confined populations (e.g., families, schools, army barracks). PATHOGENESIS Adherence factors - The P1 Adhesin localizes at tips of the bacterial cells and binds to sialic acid residues on host epithelial cells.The nature of the adhesins in the other species has not been established. Colonization of the respiratory tract by M. pneumoniae results in the cessation of ciliary movement. Toxic Metabolic Products Immunopathogenesis : most children are infected from 2 - 5 years of age but disease is most common in children 5-15 years of age. Clinical Findings M.pneumoniae primary atypical pneumonia. Incubation: 1-3 weeks This disease can range from subclinical to bronchopneumonia, often with a gradual onset and mild to moderate severity. A long convalescence (4-6 weeks) and several possible complications (CNS, cardiac) follow acute disease. Clinical Findings U. urealyticum, M.hominis, M.genitalium are responsible for one form of nongonococcal urethritis. M. hominis is associated with pyelonephritis, pelvic inflammatory disease and post-partum fevers. HOST DEFENSES Host defenses are not well characterized but probably involve both humoral and cell mediated responses. EPIDEMIOLOGY Mycoplasma affect a specific age distribution (5-9 year olds) and represent 8-15% of all pneumonias in school age children. Disease occurs worldwide, is endemic in some areas and is spread by close personal contact (schools, families). U. urealyticum is sexually acquired. Antibody titers in different age groups. Anti-mycoplasma pneumoniae antibodies indicate pneumonia caused by this organism is highest in the 5-15 year age group Acquired Pneumonia Caused by Mycoplasma pneumoniae Microbiological diagnosis Specimens: throat swab, sputum, genital secretion, etc. Microscopy - This is not particularly useful because of the absence of a cell wall but it can be helpful in eliminating other possible pathogens. Culture - Sputum (usually scant) or throat washings must be sent to the laboratory in special transport medium. It may take 2 -3 weeks to get a positive identification. Culture is essential for a definitive diagnosis. Complement fixation test Cold agglutinins - Approximately 34% - 68% of patients with M. pneumoniae infection develop cold agglutinins. ELISA - There is a new ELISA for IgM that has been used for diagnosis of acute infection. PCR The antibodies of cold agglutinins arise before the complement fixing antibodies and they decline faster CONTROL Sanitary: Avoidance of contacts, if possible. Immunological: No single vaccine is available. Natural resistance follows infection. Chemotherapeutic: Tetracycline,erythromycin or chloramphenicol are effective. Mycoplasma and L Form Bacteria MYCOPLASMA L-FORM BACTERIA No genetic relationship with bacteria Relate to their parent bacteria ,sometimes can revert Cholesterol for their cell membrane No cholesterol for their cell membrane Stable in ordinary medium Need hyperosmotic solution Grow slowly, colony small (diameter 0.1-0.3mm) Colony larger(diameter 0.51.0mm) Low turbidity in liquid medium High turbidity in liquid medium ,may adhere to the wall or bottom of the tube


![2- Pneumonia I [Autosaved]](http://s3.studylib.net/store/data/009752027_1-098b5b19a0e3b878ffe76ff65cdcd01d-300x300.png)