Bernard-Soulier syndrome
advertisement

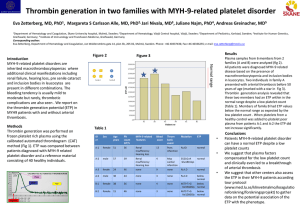
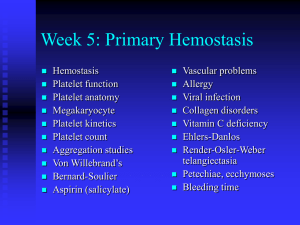
Platelet structure 1 • Membrane glycoproteins – IIb-IIIa: integrin, cryptic in resting platelet, after platelet activation binds fibrinogen and other adhesive proteins, necessary for aggregation – Ib-IX-V: binds VWF, necessary for platelet adhesion at high shear rates – Ia-IIa: integrin, binds collagen, mediates adhesion at low shear rates and platelet spreading (also acts as receptor) Platelet structure 2 • Membrane receptors – Thrombin receptors (2): cleaved and activated by thrombin – Thromboxane A2 receptor – ADP receptors (3) – Epinephrine receptor – Serotonin receptor – Cytokine, chemokine receptors – Fc receptor Platelet structure 3 • Granules – Dense granules: small molecules involved in platelet activation (ATP/ADP, serotonin) – Alpha granules: fibrinogen, fibronectin, thrombospondin, P-selectin, plasminogen, alpha-2 antiplasmin, factor V, PF4, PDGF, TGF-alpha and beta, ECGF Bernard-Soulier syndrome • Pathophysiology: – Deficiency of platelet membrane glycoprotein Ib-IX (VWF “receptor”) – Defective platelet adhesion • Clinical: Moderate to severe bleeding • Inheritance: autosomal recessive • Morphology: – Giant platelets – Thrombocytopenia (20-100K) • Diagnosis: – No agglutination with ristocetin, decr thrombin response, responses to other agonists intact – Morphology – Decreased GP Ib expression Bernard-Soulier syndrome Glanzmann thrombasthenia • Pathophysiology: – Deficiency of platelet membrane GPIIb-IIIa – Absent platelet aggregation with all agonists; agglutination by ristocetin intact • • • • Clinical: Moderate to severe bleeding Inheritance: autosomal recessive Morphology: normal Diagnosis: – Defective platelet aggregation – Decreased GP IIb-IIIa expression Gray platelet syndrome • • • • Pathophysiology: Empty platelet alpha granules Clinical: Mild bleeding Inheritance: Autosomal dominant or recessive Morphology: – – – – Hypogranular platelets Giant platelets Thrombocytopenia (30-100K) Myelofibrosis in some patients • Diagnosis – Variably abnormal platelet aggregation (can be normal) – Abnormal platelet appearance on blood smear – Electron microscopy showing absent alpha granules Gray platelet syndrome Giant platelet syndromes associated with MYH9 mutations 1. 2. 3. 4. May-Hegglin anomaly Fechtner syndrome Sebastian syndrome Epstein syndrome • All associated with mutations in the non-muscle myosin heavy chain gene MYH9 Thrombocytopenia with giant platelets, but mild bleeding Autosomal dominant inheritance No consistent defects of platelet function detectable in the clinical laboratory Diagnosis usually based on clinical picture, family history, examination of blood smear for neutrophil inclusions • • • • Giant platelet syndromes associated with MYH9 mutations Syndrome MayHegglin Fechtner Sebastian Epstein Neutrophil Hereditary Deafness inclusions nephritis Yes No No Yes Yes Yes Yes* No No No Yes Yes *Neutrophil inclusions have different structure from those in May-Hegglin Neutrophil inclusions in May-Hegglin anomaly Neutrophil inclusions in MYH9 giant platelet syndromes May-Hegglin Sebastian In both cases an oval cytoplasmic inclusion (*) not bounded by a membrane and lacking specific granules is evident (original magnification 7,000). At higher magnification (insets, original magnification 13,400), inclusion bodies in MHA contain clusters of ribosomes oriented along parallel filaments 7?10 nm in diameter, whereas in SBS they are composed of highly dispersed filaments and randomly distributed ribosomes. Wiskott-Aldrich syndrome • Pathophysiology – Mutation in WASP signaling protein – Decreased secretion and aggregation with multiple agonists; defective T-cell function • Clinical: – Mild to severe bleeding – Eczema, immunodeficiency • Inheritance: X-linked • Morphology: – Thrombocytopenia (20-100K) – Small platelets with few granules • Diagnosis: Family hx, clinical picture, genetic testing Wiskott-Aldrich syndrome Hermansky Pudlak syndrome Chédiak-Higashi syndrome • Pathophysiology: – Platelet dense granule deficiency: decreased aggregation & secretion with multiple agonists – Defective pigmentation – Defective lysosomal function in other cells • Clinical: – Mild to moderate bleeding – Oculocutaneous albinism (HPS) – Lysosomal storage disorder with ceroid deposition, lung & GI disease (HPS) – Immunodeficiency, lymphomas (CHS) • Inheritance: autosomal recessive • Morphology – Reduced dense granules – Abnormal neutrophil granules (CHS) • Diagnosis: clinical picture, neutrophil inclusions (CHS), genetic testing HPS, with oculocutaneous albinism Chédiak-Higashi, showing neutrophil inclusions Hermansky-Pudlak syndrome Br J Haematol 2007;138:671 Disaggregation after primary aggregation with ADP Dense granule deficiency Control platelet Platelet type von Willebrand disease • Pathophysiology: Gain of function mutation in GP Ib, with enhanced binding to VWF and clearance of largest multimers from blood • Clinical: Mild to moderate bleeding • Inheritance: Autosomal dominant • Morphology: Normal, but platelet count often low • Diagnosis: Variably low VWF antigen, disproportionately low ristocetin cofactor activity, loss of largest VWF multimers on electrophoresis, enhanced platelet agglutination by low dose ristocetin (indistinguishable from type 2B VWD) • Can distinguish from 2B VWD by mixing studies with normal/pt platelets and plasma and low dose ristocetin, or by genetic testing Von Willebrand multimer analysis