TUMORS-OF-LUNG-AND-PLEURA
advertisement

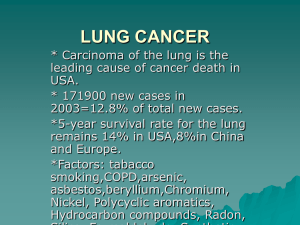
TUMORS OF LUNG AND PLEURA TUMORS OF THE LUNG TYPES : • Carcinomas – 90-95 % • Carcinoids – 5% • Mesenchymal tumour – 2-5 % HISTOLOGIC CLASSIFICATION OF MALIGNANT EPITHELIAL LUNG TUMORS • Squamous Cell Carcinoma • Small Cell Carcinoma • Adenocarcinoma Acinar, papillary, bronchiolo-alveolar, solid, mixed • Large Cell Carcinoma • Large Cell Neuroendocrine Carcinoma • Adenosquamous Carcinoma • Carcinomas with pleomorphic, sarcomatoid, or sarcomatous elements • Carcinoid tumor – Typical – Atypical . Carcinoma of salivary gland type . Unclassified Carcinoma Etiology and pathogenesis • Several environmental factors are known to cause genetic damage that transform benign bronchial epithelium to neoplastic tissue 1 -Tobacco Smoking • Overwhelming evidence • 87% lung carcinoma occurs in smokers • 10 fold greater risk – Average smoker • 60 fold greater risk – Heavy smokers • Passive smoking – 3000 deaths per year Histologic sequence of events: • Normal epithelium • Squamous Metaplasia • Squamous Dysplasia • Carcinoma in situ • Invasive Carcinoma Cytogenetics : • Mutations in p53 gene ( G: C > T: A) Carcinogens in cigarette smoke: • Polycyclic aromatic hydrocarbons – Benzopyrine • Phenol derivatives • Radioactive elements – Polonium – 210 – Carbon – 14 – Potassium - 40 Other Contaminants : • • • • Arsenic Nickel Molds Additives 2 -Industrial Hazards • High dose Ionizing Radiation; High incidence in Hiroshima / Nagasaki atomic bomb survivors • Uranium – 4 times increased risk in • nonsmoker uranium miners Asbestos – 5 times increased risk in nonsmokers, 50-90 times in smokers • Latent period – 10-30 years 3 -Air Pollution • Indoor air pollution – Radon • Increased incidence in miners . Molecular Genetics • • -For all practical purposes, lung cancer is divided into two clinical subgroups : a - Small Cell Carcinoma b - Nonsmall Cell Carcinoma -Supported by some specific molecular lesions in each subgroup . Oncogenes : • C-Myc • Kras • EGFR • c-MET • c-KIT Tumor Suppression Genes : • p53 • RB1 • p16 ( INK 4a) • Genes on chromosome 3p (FHIT, RASSF 1A ) Small Cell Carcinoma Genes : • C-KIT • MYC N • MYC L • p53 • 3p ( Early genetic change ) • RB • BCL 2 Non Small Cell Carcinoma Genes : • EGFR • KRAS ( Late genetic change) • p53 • p16 INK4a MORPHOLOGY • Origin : – ¾ in the hilus – Bronchi – ¼ in the periphery – Alveolar septal cells, terminal bronchioles PRECURSOR LESION PHASE • ( Squamous metaplasia ,Dysplasia, Carcinoma in situ ) – Preceed invasive carcinoma – May last for many years – Asymptomatic – No X-Ray changes; Small lesion – Positive diagnostic test ; Cytology ( Sputum, Bronchial lavage fluid/ brushings ) • PRECURSOR LESION POST INVASION PHASE • Larger tumour mass • Symptomatic, obstruct major bronchus – Infection ( Pneumonia ) – Atelectasis . Grow inside the bronchus; fungating mass . Penetrate the wall of the bronchus into the peribronchial tissue POST INVASION PHASE INVASIVE LESION • Cauliflower like intraparenchymal mass • Grey white, firm to hard • Yellowish white mottling and softening • Extension to pleural surface and cavity • Involve pericardium • Regional lymph node involvement (Tracheal, Bronchial, Mediastinal ) Metastasis • Via both lymphatics and hematogenous spread • May be the first manifestation • Any organ; most commonly – Adrenals ( 60 %) – Liver ( 30-50%) – Brain ( 20% ) – Bone ( 20% ) ADENOCARCINOMA • Malignant epithelial tumour with glandular differentiation or mucin production • Patterns of growth : – Acinar – Papillary – Bronchioloalveolar – Solid with mucin formation ADENOCARCINOMA; CHARACTERISTICS • • • • • • • Most common type in : Woman Non-smokers ( 75% v/s > 98% ) Lesion more peripherally located Smaller size Slow growth Early and widespread mets Cytogenetics ; - K RAS ( Specific for adenocarcinoma ) - p53 , RB1, p16 - EGFR ( mutation, amplification ) - C-MET Bronchioloalveolar Carcinoma • Arises in terminal bronchioloalveolar region • 1-9 % • Gross : – Single / multiple nodules in lung periphery – Solid, grey white areas like pneumonia Bronchioloalveolar Carcinoma Histology : • Growth along the preexisting structures • Preservation of alveolar architecture • No stromal, vascular or pleural invasion Sub types : - Mucinous: Tall columnar cells with cytoplasmic / intraalveolar mucin - Non-mucinous: Columnar or cuboidal cells SEQUENCE OF EVENTS -Atypical adenomatous hyperplasia (Well demarcated focus of cuboidal to low columnar epithelium) | -Bronchioloalveolar Carcinoma | -Invasive Adenocarcinoma (Poorly demarcated invasive lesion/tumor) SQUAMOUS CELL CARCINOMA • Most common lung cancer in Males • Strong correlation with smoking • Arise from segmental bronchi HISTOLOGY : – Sheets / clusters of atypical squamous cells – Keratinization / squamous pearls varies with grade of tumour – Intercellular bridges • • • Histologic Grades : Well differentiated Moderately differentiated Poorly differentiated Cytogenetics : - p53 mutation; Most common - RB1, p16 ( INK4a), EGFR - Alleles at 3p, 9p, 17p - EGFR overexpression SMALL CELL CARCINOMA • Highly malignant tumour • Strong correlation to cigarette smoking (Only 1% in non-smokers) • May arise centrally or peripherally • No percursor / preinvasive lesion • Widely metastatic • Surgically incurable • Ectopic hormone production Small Cell Carcinoma • Cytogenetics : - p53 mutation - RB1 mutation Small Cell Carcinoma • • • • • • • Histology : Clusters of relatively small round/oval/spindle shaped neoplastic epithelial cells with scant cytoplasm, illdefined cell borders Salt and pepper chromatin Absent /inconspicuous nucleoli Prominent nuclear molding High mitotic count Azzopardi effect Necrosis Small Cell Carcinoma • • • • Immunohistochemistry : Synaptophysin Chromogranin CD 57 Parathyroid hormone- like product Electron Microscopy : Dense core neurosecretory granules LARGE CELL CARCINOMA • • • • • Large neoplastic cells Increased N/C ratio Prominent Nucleoli Represent poorly differentiated Squamous Cell Carcinoma and Adenocarcinoma Histologic variants : – Large cell neuroendocrine carcinoma; organoid nests, trabeculae, rosette-like and pallisading patterns – Neuroendocrine features both on Immunohistochemistry and Electron Microscopy Combined Carcinoma • Histology similar to two or more of usual lung carcinomas Complications of CA Lung • Emphysema • Atelectasis • Severe suppurative /ulcerative bronchitis • Bronchiectasis • Lung Abscess • Superior vena cava syndrome • Pericarditis • Pleuritis CLINICAL PRESENTATION • Cough • Weight loss • Chest pain • Dyspnoea INVESTIGATIONS • Chest X-Ray • Sputum for Cytology • Bronchial washings / brushings for Cytology • CT guided lung biopsy • CT Scan / MRI TREATMENT Early stage disease ( 15% ) – Lobectomy – Pneumonectomy Last stage Disease – Chemotherapy – Radiotherapy – EGFR inhibitors SURVIVAL RATE •Early stage : 48% •Last stage : 10-15 % NEUROENDOCRINE NEOPLASMS 1 .Benign tumorlet : Small nests of hyperplastic neuroendocrine cells adjacent to scarring / chronic inflammation 2 .Carcinoids - Typical - Atypical 3. Small Cell Carcinoma 4. Large Cell Neuroendocrine Carcinoma Carcinoid tumour • 1-5 % • < 40 years of age • 20-40 % nonsmokers • Behavior; low grade malignant epithelial neoplasm • Subclassified into : • • Typical Atypical • Central / peripheral origin Carcinoid Tumor Morphology : • Gross : – Finger- like or spherical polypoidal masses – Project into the lumen of mainstem bronchi – Covered by intact mucosa – Size ;usually < 3-4 cm Carcinoid Tumor Histology : • Patterns – Organoid, trabecular, pallisading, • • • ribbon or rosette-like Delicate fibrovascular stroma Regular, uniform, round cells with moderate cytoplasm Mitosis; < 2 /10 x HPF – Typical Carcinoid. 2-10 /10 x HPF – Atypical Carcinoid. Histology Atypical Carcinoid : • Increased pleomorphism • Necrosis • Disorganised growth pattern • Lymphatic invasion • Mitoses 2-10 /10 HPF MISCLENOUS TUMOURS • • • • • • • • • • Inflammatory Myofibroblastic Tumor Fibroma Fibrosarcoma Lymphangioleiomyomatosis Leiomyoma Haemangioma Haemangiopericytoma Chordoma Langerhan Cell Histiocytosis Hamartoma Inflammatory Myofibroblastic Tumor Langerhan Cell Histiocytosis Hamartoma Lung Hamartoma Lung METASTASIS TO LUNG • More common than any of the other lung malignancy • From any carcinoma/sarcoma • TUMORS OF PLEURA PLEURAL TUMORS Solitary Fibrous Tumor • Size – Variable; small 1-2 cm to very large tumour • Histology : -Whorls of reticulin and collagen fibres with scattered fibroblast- like spindle cells • CD 34 + • Keratin – • D/D : Mesothelioma Pleural Tumors Malignant Mesothelioma : • Asbestos exposure ; 7-10 % • Latent period ; 25-45 years -Histology : • Asbestos bodies in the lung • Asbestos plaque -Cytogenetics : Del 1p, 3pCq ,9p or 22q p16 mutation Malignant Mesothelioma Morphology : Gross : • Thick layer of soft,gelatinous greyish pink tumour “ensheathing” the lung Histology : . Epithelioid- 60 %; Cuboidal /Columnar cells, tubules or papillary .Sarcomatoid- 20%; spindle cell growth resembling Fibrosarcoma .Mixed- 20% Malignant Mesothelioma - Clinical Presentation : • Chest pain • Dyspnoea • Recurrent pleural effusions • Hilar Lymphadenopathy • Distant mets ; liver etc. - Prognosis : 50% die within 12 months Malignant Mesothelioma Treatment : • Extrapleural pneumonectomy • Chemotherapy • Radiotherapy