LUNG CANCER - UMF IASI 2015
advertisement

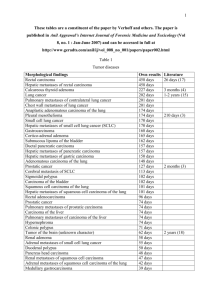
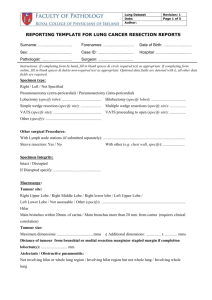
LUNG CANCER * Carcinoma of the lung is the leading cause of cancer death in USA. * 171900 new cases in 2003=12.8% of total new cases. *5-year survival rate for the lung remains 14% in USA,8%in China and Europe. *Factors: tabacco smoking,COPD,arsenic, asbestos,beryllium,Chromium, Nickel, Polycyclic aromatics, Hydrocarbon compounds, Radon, Investigation for lung cancer Chest X-ray, Thoracic CT, Fiberbronchoscopy,with biopsy, Fine-needle aspiration from a pulmonary nodules, Ultrasonography – pulmonary/abdominal. PET, Mediastinoscopy for mediastinal limph nodes, VATS for diagnosis of small pulmonary nodules. Clinical presentation of lung cancer Cough, 29-87% Hemoptysis- 9-57% Chest pain 6-60% Dyspnea 3-58% Wheezing or stridor 2-14% Pleural effusion 7% Dysphagia 2% Superior vena cava syndrome 4-11% Pancoast syndrome 3-5% Phrenic nerve paralysis 1% Symptoms from metastatic disease Bone metastases: bone pain in hands,feet. Neurologic metastases:central nervous system,spinal cord compression secondary to epidural or vertebral mts. Adrenal mts, Liver mts, Others sites:soft tissue,etc. Paraneoplastic syndromes Metabolic: - hypercalcemia, - Cushing syndrome, - carcinoid syndrome, -gynecomastia, -elevated growth hormone level,prolactin,folliclestimulating hormone,luteinizing hormone,antidiuretic hormone production. - hypoglicemia, -hypertiroidism Paraneoplastic syndomes Neurologic -encephalopathy, - subacute cerebrall degeneration - peripheral neuropathy, - polymiosytis, - autonomic neuropathy, - myoclonus. Paraneoplastic syndromes Skeletal - clubbing - pulmonary hypertrophic osteoartropathy Hematologic - anemia, -leukemoid reactions -trombocytosis, -trombocytopenia, -eosinophilia, -pure red cell aplasia, -disseminated intravascular coagulation Paraneoplastic syndromes Cutaneous and muscular - hyperkeratosis, - dermatomyositis, - acanthosis nigricans, -erytremia gyratum repens, - hypertricosis lanuginosa acquisita Other -nephrotic syndrome, -hypouricemia, -hyperamylasemia, -anorexia-cachexia. Diagnosis and staging of lung cancer Diagnosis : sputum cytology, fiberoptic bronchoscopy, VATS,CT,Xr Transthoracic fine-needle aspiration Indication 1.Patient is a high operative risk, 2.Patient hjas a low risk of malignancy based on clinical and radiologic characteristics. 3. A definite benigne diagnosis is considered likely, 4. The patient prefers to have a diagnosis of cancer before proceeding to the operating room. 5.Patient is not an operative candidate, but tissue confirmation is needed before definitive treatment with radiation therapy or chemotherapy or both. Characteristics of solitary pulmonary nodules predicting malignancy Radiologic characteristics - diameter>2cm, - spiculation present, - upper lobe location Clinical characteristics - age>40 years - positive smoking history History of other cancer Radiographic features Early signs of a lung tumor are as follows: 1.a density within the lung parenchima, 2. a cavitary mass, 3. a segmental, indistinct, poorly defined dense area, 4. a nodular streaked, local infiltration along the course of a blood vesel, 5. segmental consolidation, 6 a roughly triangular lesion arising in the apex and extending toward the hilus, 7. a mediastinal mass, 8.an enlargement of one hilus, 9. segmental or lobar obstructive emphysema, 10. segmental atelectasis. Chest radiographic presentations of lung cancer Pulmonary nodule<3 cm in size, Pulmonary or hilar mass, Pulmonary opacities(lobar, segmental, subsegmental), Tracheal or bronchial intraluminal opacity, luminal narrowing or chest wll thickening, Atelectasis (lung, lobar, segmental, subsegmental) Pulmonary cavitary lesion, Air trapping(hyperinflation) Mediastinal mass, Pleural lesion, Pleural effusion, Pericardial effusion (enlarged cardiac silhouette), Elevated hemidiaphragm(paralysis or paresis), Chest wall mass or bone metastases. Classification of lung carcinoma Squamous cell carcinoma, Small cell carcinoma - pure small cell carcinoma, - small- large cell carcinoma, - combined small cell carcinoma (with areas of squamous or glandular differentiation), Adenocarcinoma - variant: bronchioloalveolar carcinoma, Large cell carcinoma, Adenosquamous carcinoma. TNM Definition TNM classification Primary tumour (T) TxPrimary tumour cannot be assessed or tumour proven by the presence of malignant cells in sputum or bronchial washings but not visualised by imaging or bronchoscopy T0No evidence of primary tumour TisCarcinoma in situ T1Tumour <3 cm in greatest dimension, surrounded by lung or visceral pleura, without bronchoscopic evidence of invasion more proximal than the lobar bronchus T2Tumour with any of the following features of size or extent: >3 cm in greatest dimension involves main bronchus >2 cm distal to the carina invades the visceral pleura associated with atelectasis or obstructive pneumonitis that extends to the hilar region but does not involve the entire lung T3Tumour of any size that directly invades the following: chest wall (including superior sulcus tumours), diaphragm, mediastinal pleura, parietal pericardium; or tumour in the main bronchus <2 cm distal to the carina but without involvement of the carina; or associated atelectasis or obstructive pneumonitis of the entire lung T4Tumour of any size that involves any of the following: mediastinum, heart, great vessels, trachea, oesophagus, vertebral body, carina; or tumour with a malignant pleural or pericardial effusion, or with satellite tumour nodule(s) within the ipsilateral primary tumour lobe of the lung Stage Grouping for Lung Cancer Regional lymph nodes (N) NxRegional lymph nodes cannot be assessed N0No regional lymph node metastases N1Metastases to ipsilateral peribronchial and/or ipsilateral hilar lymph nodes and intrapulmonary nodes involved by direct extension of primary tumour N2Metastases to ipsilateral mediastinal and/or subcarinal lymph nodes N3Metastases to contralateral mediastinal, contralateral hilar, ipsilateral or contralateral saclene or supraclavicular lymph nodes Distant metastases (M) Mx Presence of distant metastases cannot be assessed M0 No distant metastases M1Distant metastases present Stage grouping TNM subsets 0Carcinoma in situ IA T1N0M0 IB T2N0M0 IIA T1N1M0 IIB T2N1M0 T3N0M0 IIIA T3N1M0 T1N2M0 T2N2M0 T3N2M0 IIIB T4N0M0 T4N1M0 T4N2M0 T1N3M0 T2N3M0 T3N3M0 T4N3M0 IV Any T Any N M1 Algoritm for therapy in lung cancer NSCLC Comprehensive clinical evaluation Clinical examination negative - Chest CT *T4 = 1. defined 2. indeterminate : VATS surgery. ** LN Positive = sample LN= a)N2 Positive- unresectable and induction protocol b)N3 Positive- unresectable *** LN Negative = Surgery Clinical examination positive suspect M1. *Organ specific= specific scan=a) negative scan =follow chest CT sequence, b) positive scan= treat M1. **Organ nonspecific findings= scan succesive organs= a)negative scan= follow chest CT sequence, b) positive scan= treat M1.