Soft tissue tumors - Patologos de Puerto Rico
advertisement

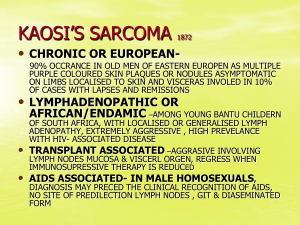
Soft Tissue Tumors Academy of Pathology and Laboratory Medicine of Puerto Rico April 2013 Bruce Horten, M.D. Medical Director Integrated Oncology, New York Part I Sarcomas In My Consult Practice MFH Evaluation • IHC • Molecular FISH RT∙PCR Part II GIST • IHC • Molecular Small Round Cell Tumors • IHC • Molecular Brain Tumor Evaluation Explosion of Interest in Soft Tissue Tumors • WHO Classification of Tumors of Soft Tissue and Bone 4th Edition 2013 Editors include C. Fletcher, J. Bridge • USCAP Annual Meeting, Baltimore 2013 * Long Course Soft Tissue Tumors C. Fletcher, C. Antonescu * Special Courses Practical Guide to Molecular Testing in Cancer J. Bridge Advanced Molecular Pathology F. Barr • New York Pathological Society, Saturday May 4 President’s All Day Symposium: Soft Tissue Neoplasms C. Antonescu, C. Fletcher, M. Miettinen Most Common Sarcoma Diagnoses • Currently a very elusive statistic Dependant on a site’s approach to malignant fibrous histiocytoma. As a result, very few current texts offer such a statistic. • Enzinger/Weiss or Rosai In adults, spindle cell sarcomas dominate. • 35-45% MFH and liposarcoma. In childhood, round cell sarcomas dominate. • Rhabdomyosarcoma, neuroblastoma, PNET / Ewing’s. • Current WHO (2013) on sarcomas 75% include undifferentiated pleomorphic sarcoma, liposarcoma, leiomyo-, myxofibro-, synovial sarcoma and MPNST. 75% highly malignant 75% in extremities (esp. thigh) Malignant Fibrous Histiocytoma (MFH) • Now considered a diagnosis of exclusion. • The most high grade, poorly differentiated myofibroblastic or fibroblastic sarcoma. • To properly evaluate such a tumor, it is now considered essential to exclude (usually via immunohistochemistry) more specific entities. • If all investigations come up negative, the new term of choice is: “Undifferentiated Pleomorphic Sarcoma (UPS)” What Has Become of MFH? • Fletcher Study (AJSP 1992;16:213-228) 61% Pleomorphic sarcoma with specific differentiation 13% Pseudosarcoma 26% Remain MFH though now termed UPS What Are The Specific Subtypes (61%)? • About 1/3 are myogenic including: Leiomyo- and rhabdomyo- sarcoma However the rhabdo subtype is very rare • Another 1/3 are liposarcomas including: Dedifferentiated (abdomen) and pleomorphic • A final 1/3 includes: Myxofibrosarcoma and Malignant peripheral nerve sheath tumor Do These Subtypes Really Matter? • The myoid subtypes are very aggressive with a highly metastatic rate (70% to >90%). 5 yr. • The liposarcoma subtypes are less aggressive with a 5 yr. metastatic rate of 15% (dedifferentiated) to 40% (pleomorphic). Pseudosarcomas (13%) • Sarcomatoid carcinoma. Most common. • Melanoma • Anaplastic lymphoma How Are These MFH-like Entities Recognized? • Principally By Immunohistochemistry Myoid Lipoid MPNST Smooth Muscle Actin Dedifferentiated: CD34, MDM2/CDK4 S∙100 SMMHC Pleomorphic: Lipoblasts CD34 Caldesmon S∙100 Calponin Desmin Myogenin • But Also By Using Molecular Techniques • Above all gene fusions Translocations Inversions Deletions Duplications • Examples DDIT3 (CHOP) FISH break-apart probe • Myxoid liposarcoma FOX01 (FKHR) FISH break-apart probe • Alveolar rhabdomyosarcoma How Are Pseudosarcomas Recognized? • By Immunohistochemistry Sarcomatoid Carcinoma Melanoma Anaplastic Lymphoma CAM 5.2 S∙100 CD30 AE1/AE3 HMB45 ALK-1 CK903 Melan A CK5/6 MiTF1 p63 And What of the Remaining Undifferentiated Pleomorphic Sarcoma? • By immunohistochemistry, focal smooth muscle actin may be seen but no desmin reactivity. The pattern for myofibroblasts. • By molecular techniques, largely nonspecific. BUT by CGH (Comparative Genomic Hybridization) some shared factors with pleomorphic leiomyosarcoma. Part II Gastrointestinal Stromal Tumors Most common mesenchymal tumor of the gastrointestinal tract At least ½ in the stomach of which ¼ of these gastric tumors are malignant Gastrointestinal Stromal Tumors Cell of origin: Interstitial cells of Cajal • Immunohistochemistry: DOG1 – Most sensitive marker. Also ANO-1. CD117 (KIT) CD34 With exclusions S100 and SMA • Prognostic Factors: Tumor size: 2,5,10,>10 cm. Mitotic activity: ≤ or > 5 per 50 hpf Anatomic site: gastric vs. small intestinal Mutations in GIST Wild Type 15% KIT 75% PDGFRA 10% Exon 9 8% Exon 12 2% Exon 11 65% Exon 14 Rare Exon 13 1% Exon 18 8% Exon 17 1% Includes D842V Predictive Value of Mutations • Exon 11 mutation KIT (65%) Favorable survival and response to Imatinib (Gleevec) • Exon 9 mutation KIT (8%) Best response to Imatinib if dose is doubled to 800 mg. • Exon 18 (D842V) PDGFRA (8%) Resistent to Imatinib • Wild type (15%) Regular dose of Imatinib but response variable Small Round Cell Tumors of Childhood • Neuroblastoma • Ewing’s sarcoma/primitive neuroectodermal tumor (ES/PNET) • Rhabdomyosarcoma • Desmoplastic small round cell tumor IHC Analysis of Small Round Cell Tumors NERD NERD AE1/AE3 e D Desmin Vimentin ERD CD45 RD Synaptophysin Ne CD56 Ne Chromogranin Ne D S100 N CD99 E EMA FLI1 E Myogenin WT1(c) D NSE D R NE D Neuroblastoma • • The most common of the small round cell tumors outside the CNS. Grading systems • At least 5 are proposed. Differentiation is key. • 5%: Neuropil with ganglion cells Age: 2 yrs. Mitotic rate: 10/10 hpf Other prognostic factors IHC: CD45, S∙100 favorable CD44, BCL2, P-glyoprotein unfavorable Flow: Aneuploid and 100% S, G2, M phases favorable FISH: NMYC Amplification in 25%. Unfavorable. Ewing’s Sarcoma/ Primitive Neuroectodermal Tumor • • Older and broader age range than neuroblastoma. Also broader sites of origin from bone to soft tissues. 95% of cases feature the fusion of the EWS gene at 22q12 with another gene especially FLI-1 (80-90%). • Translocation: t(11;22) Fusion gene: EWSR1-FLI-1 Protein: FLI-1 (nuclear) IHC CD99 and FLI-1 versus NSE in neuroblastoma EWSR1 And Its Partners At Least 9 Different Partners In Ewing’s/PNET 3 in myoepithelial tumor of soft tissue 2 in clear cell sarcoma 1 in extraskeletal myxoid chondro sarcoma 1 in myxoid/round cell liposarcoma 1 in desmoplastic small round cell sarcoma Rhabdomyosarcoma Embryonal versus Alveolar Sites: • Head/neck and urogenital vs. extremities Cytology/Histology Prognosis IHC: • Myogenin, desmin, sarcomeric actin Molecular Analysis of Rhabdomyosarcoma • Embryonal No distinctive genetic features • Alveolar FOXO1 (FKHR) Translocations 2;13 (PAX3-FOX) more aggressive than 1;13 (PAX 7-FOX) NMYC in about 50% of alveolar subtype Brain Tumor Evaluation • Immunohistochemistry CAM 5.2 EMA CHROMOGRANIN Vimentin PR GH GFAP S∙100 Prolactin Neu∙N ACTH Ki67 LH TSH FSH • FISH 1p/19q deletion