Slide - Maine Dartmouth Family Medicine Residency
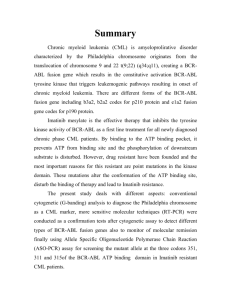
advertisement

Genomics, cancer, and medicine: 10 years after the Human Genome Project Edison Liu, M.D. April 13, 2012 Declaration We are entering one of the most profound periods of advancement in biology and medicine – one that will transform: Health and Medicine Driven by technologies in genetics, genomics, and computational biology Genomics and Genetics Genetics: study of genes and their function Genomics: study of all genes and how they function together “Discover all possible genes involved in a biological process or a human disease” Genomics enables the complete genetic “view” of a disease Transformative technologies enabling this revolution: •New generation of ultra-fast sequencing technologies “Massive Data Generation” • Enabling computational advances “”Analytical power“ •Genetic engineering to model organisms of disease “Surrogates of disease” A* C T A G C T G A T T C A G T* T* T* A A G T C T A G C T G A T T A C G A T G G* C* A* Massively Parallel Sequencing: Sequencing by Synthesis ~105-107 kb per run = 0.1-3 X human genome equivalents / run 7 orders of magnitude increase in throughput MR Stratton et al. Nature 458, 719-724 (2009) Cost of sequencing a human genome 300 million USD - 30 million USD - 3 million USD - 300 million Cost-effective sequencing = Accessibility of genomic data 1 million 300,000 USD $60,000 30,000 USD - $ 3,000 Low complexity image Data complexity when ordered appropriately gives high resolution picture Genomic scale information provides unique biological insights Genomics & Personalized Medicine Towards personalized cancer medicine No benefit Non-selective Conventional chemothrapy Molecular marker & target Severe side effect Responders Personalized cancer medicine Other therapy No treatment Selection High response rate by marker Molecular specific drug CAT ATE RAT BAT ATE RAT RAT ATE CAT Wild Type Point Mutation Rearrangement Cathryn Kathryn Kathrine Polymorphism Polymorphism Polymorphism Chronic Myelogenous Leukemia: and the 9;22 chromosomal rearrangement Molecular Mechanisms: How to make a Leukemia • Ph1 chromosome identified 1960 as a marker for CML (Nowell) • bcr-abl cloned and shown to be the molecular mechanism 1984-1990 (Groffen and Lugo) BCR ABL Chronic Myelogenous Leukemia Chronic Myelogenous Leukemia: Mortality 1969 - 2002 Large scale clinical trials begin with Gleevec Gleevec Approved By FDA STI521:Gleevec BCR ABL From Concept to Molecular Mechanism to Treatment • Ph1 chromosome identified 1960 as a marker for CML (Nowell) • bcr-abl cloned and shown to be the molecular mechanism 1984-1990 (Groffen and Lugo) • Specific drug (Gleevec) to target gene abnormality 1999 (Druker) From discovery of a single oncogene to treatment: 39 years Nature 2007 In 2007, the genomic analysis of one lung cancer from a 62 year-old smoker EML-ALK fusion in 6% of lung cancer patients EML ALK Lung Cancer Crizotinib 60% response rate in those 6% of patients with lung cancer with the EML-ALK mutation. On August 26, 2011, the US FDA gave approval of crizotinib by for the treatment of ALK-rearranged lung cancer 4 years from genomic discovery to treatment Ou, Drug Des Devel Ther. 2011; 5: 471–485. Chronic Myelogenous Leukemia (CML) Optimizing treatment for CML based on genetic makeup of the patient Clinical Challenge: Drug resistance •Acquired resistance – resistance after long term treatment - due to second ABL mutation •Primary resistance – resistance at the beginning of treatment. •In Asia, complete cytogenetic response rates are lower 50% vs. 74%. Mechanism unknown Question: is there a reason why 25% of CML cases do not respond to imatinib? Approach: We compared the genomes of three CML cases with primary resistance to Imatinib with two CML cases sensitive to Imatinib therapy Results: 3/3 resistance cases had the same 2.9kb deletion in the BIM gene not seen in sensitive cases (0/2) BIM: • BIM is a gene that activates cell death (pro-apoptotic). • Activated BCR-ABL1, suppresses BIM function thus allowing leukemia cells to survive. When CML cells are treated with Imatinib, BIM expression goes up cell death Bcr-ABL: CML Imatinib Intact BIM Death of Leukemia cells BIM deletion polymorphism: • This deletion polymorphism is 3-5X more common in CML cases resistant to imatinib that sensitive cases • This 2.9 kb 2 deletion of BIM is not a mutation, but is a polymorphism present in normal genomes (a germline polymorphism): 12% in Asian individuals 0% in Africans 0% in Caucasians How does it work?: The 2.9kb BIM deletion polymorphism results an abnormal transcript (E3) that a produces a truncated and inactive BIM protein Normal Transcripts E3 Imatinib Bcr-ABL: CML Intact BIM Death of Leukemia cells Imatinib Bcr-ABL: CML BIM E3 Primary Drug Resistance We used this genomic intelligence to overcome this resistance: Imatinib Bcr-ABL: CML BIM 3 BH3 mimetics Bcr-ABL: CML Primary Drug Resistance Imatinib BIM Death of Leukemia cells This genomic experiment with 5 patients explains the lower response rate In North Asians to a life saving treatment in CML. Personalizing medicine in Asia Now: New ~50% cytogenetic response CML Patient in Asia Check for bcr-ABL rearrangement YES Check for 2.9kb deletion polymorphism in BIM YES NO Imatinib & BH3-mimetic Imatinib >75% cytogenetic response 75% cytogenetic response Visualizing the Cancer Genome Copy LOH Number Structural Variations BT55 ‘Conductor’ mutation = early event that conducts the direction of further cancer mutations Mutation pattern appears to be generated by separate cuts when mapped to the original physical “map” Chromosomal “origami” simultaneously generates oncogenic “pattern” Chromosomal origami to generate cancer gene cassette ERBB2 ERBB2 P53 ERBB2 17q21.3 ERBB2 17q21.3 ERBB2 17q21.3 ERBB2 BRCA1 Oncogenes 17q21.3 ERBB2/HER2 17q21.3 amplicon Oncogene BRCA1 Tumor Suppressor Gene TD207 U-Inv331 U-Inv75 17q21.3 ERBB2 TD49 + Del67 Del51 There are 16 weak oncogenes here. 4 that are synergistic with ERBB2 oncogenesis 17q21.3 Amplification BT55 (ER+, ERBB2++) Luminal B Chr17 ‘evolutionary origami’ has treatment implications for Combination therapy Cancer progression 17p (TP53) loss Chromosomal instability Tandem duplication in ERBB2 locus Recurrent UnpairedInversion: “Conductor” Mutation Massive ERBB2 amplification Nutlins 17q21.3 amplification BRCA1 locus loss Oncogenes Lapatinib Tumor Suppressor genes New Target PARP inhibitor Cancer Genomics Consultation Model Using Mouse Avatars for Human Disease Druggable mutations Tumor DNA sample Sequence Tumor Germline DNA sample Generation of serum-based personalized and private cancer biomarker test Expand tumor in NSG mice Automated sequence analysis of tumor and germline Germline pharmacogenetic analysis Identification of cancer specific rearrangements Monitor for recurrence and clonal variation Test specified drugs for response in vivo Prognostic information Devise optimal combination therapy Visualization formatted report Consultation with patient and physician for treatment plan Radiologist of the Genome Radiologist Interprets complex data rendered through computational algorithms Is the consultants to doctors Genomics, cancer, and medicine: 10 years after the Human Genome Project Edison Liu, M.D. April 13, 2012 Age Adjusted Mortality for breast cancer is declining since 1990 D ~ 20% 1990 T2N1M0 Age: 56 family history: negative Sequence performance: ER (IHC) positive HER2 (FISH) Positive Ki67: +++ GHI recurrence score: XXX 9.6 million reads; 75 base pair, paired end on Illumina HiSeq Comparison of germline and cancer genomes This is a visual representation of the cancer genome of your patient as compared to her constitutional (germline) genome. The 23 chromosomes are arrayed in a circle; amplifications are on the outer circle, and the deletions and inversions are in the inner circles. In the innermost circle is a representation of the chromosomal translocations. Each arc represents a translocation, and the intensity of the arcs is an indication of Amplification of that translocation. By clicking onto the figure, you will get a blow up of the schematic and a detailed legend. Maximal Normal The mutational load score is a composite score the integrates the mutational load that is seen in the tumor of your patient. It is made up of two components: sequence mutations, structural mutations/rearrangements. Your patient’s mutational score when compared to a panel of XXX tumors of the same type is in the following distribution: What if this trend continues? 1990 Can death from breast cancer be eliminated? 2020