Isfahan University of Technology
College of Agriculture, Department of Animal Science
Advanced Reproduction
Physiology
(Part 2)
Prepared by: A. Riasi
http://riasi.iut.ac.ir
Oogenesis & Folliculogenesis
Overview
1: ovary, 2: tertiary follicle, 3: proper ovarian ligament,
4: fallopian tube, 5: ovarian artery and vein
Overview
Overview
Overview
Overview
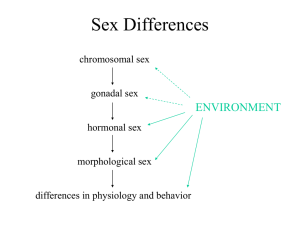
The ovaries have two distinct functions:
Producing the sex steroids and protein hormones
Prepare the vagina and fallopian tubes to assist in fertilization
Prepare the lining of uterus to accept and implant a zygote
Maintain hormonal support for the fetus before placenta capacity
Act on diverse target organs
Ovogenesis and folliculogenesis
Maintain and nurture the resident oocyte
Mature the oocyte and release it at the right time
The biology of oogenesis
Primordial germ cells migrate from the yolk sac
The primordial germ cells proliferate by mitosis to
form primary oocytes:
In cattle, the first meiotic prophase in days 75-80
The first meiotic division is not completed befor ovulation
The biology of oogenesis
In contrast the male, the female cannot manufacture
new oogonia
It must function with continuously declining number of
primary oocytes.
Folliculogenesis
The first stage of development of the ovarian follicle
parallels the prophase of the oocyte.
As an oocyte enters meiosis, it induces a single layer
of spindle cells to surround it completely.
Cytoplasmic processes from these cells attach to the plasma
membrane of the oocyte.
Folliculogenesis
In the next phase, the spindle-shaped cells become
cuboidal and granulosa cells and a primary follicle is
formed.
Then secondary follicle is created.
After that the zona pellucida is formed.
Folliculogenesis
Folliculogenesis
During the initial deposition of zona pellucida
material some changes occur in oocyte:
Formation of cortical granules within the oocyte cytoplasm
Onset of oocyte RNA synthesis
Gonadotrophin responsiveness
Folliculogenesis
Primordial, primary and secondary follicles appear in
the fetal ovary on Days 90, 140 and 210, respectively
(Russe, 1983).
The second stage of follicular development is take
place during in postnatal and in puberty.
Folliculogenesis
Follicular growth in prepubertal heifers occurs in
waves.
Each wave is preceded by a peak in serum FSH
concentrations (Fortune, 2004).
There is a marked but transient increase in blood
concentrations of both LH and FSH.
Folliculogenesis
From 30-80 days before the first ovulation, the LH
pulses frequency result:
Increases in follicle diameter
Increase in serum estradiol concentrations
Enhancing antral follicle development
Folliculogenesis
The transition to the tertiary follicle includes:
Development of the theca interna and externa
Formation of basal lamina
Formation of cumulus cells
Formation of a fluid-filled antral cavity
Folliculogenesis
The fluid in the antrum contains different chemicals:
Mucopolysachrides
Plasma proteins
Electrolytes
Glycosoaminoglycans
Proteoglycans
Gonadal steroid hormones
FSH, Inhibin and other factors
Folliculogenesis
Folliculogenesis
Folliculogenesis
The final stage of follicular development occurs only
in the postpubertal reproductive ovary.
Some event in third stage:
The granulosa cells spread apart
The cumulus oophorus loosens
The follicle generally ruptures, releasing the oocyte with
adherent cumulus oophorus
At this time the initial meiotic division complete
Follicular waves
Follicles develop in waves.
Emergence of a new follicular wave is preceded by a
rise in FSH.
Suppression of FSH prevents further growth of 3-5
mm follicles.
Follicular waves
The FSH surge peaks, on average, when the largest
follicle is about 5 mm.
Rather than selection of a dominant follicle, selection
involves an action against the other follicles in the
wave (Ginther et al, 2003).
Follicular waves
A subordinate follicle remains viable for at least 1 day
after deviation starts
Administration of FSH when a dominant follicle is
present does not consistently hasten emergence of the
next wave
Follicular waves
With decreasing serum FSH concentrations, follicles
begin to undergo changes:
Reduced production of estrogens
Reduced levels of higher molecular weight (MW) inhibins
Increased amounts of lower MW insulin-like growth factor
(IGF)-binding proteins
Culminating in granulosa cell apoptosis
Follicular waves
FSH stimulates the production of estradiol, activin-A
and inhibin-A (Glister et al, 2001).
These FSH-stimulated factors have intrafollicular
roles in deviation.
Both estradiol and inhibin act alone (as well as
synergistically) to suppress blood FSH concentrations.
Follicular waves
The estradiol secretion by dominant follicle increase
the expression of genes in granulosa cells for:
Aromatase
3-beta-HSD
Receptors for FSH and LH
Follicular waves
Follicular waves
Follicular Size
Progesterone
Atresia
Dominance
Selection
Recruitment
Ovulation
9
16
Day After Ovulation
21
Follicular waves
Follicular waves
The
IGF system is involved in cell growth and
differentiation and consists of:
IGF-1
IGF-2
IGF receptors
A family of binding proteins (IGFBPs)
IGFBP proteases
Follicular waves
It appears that pregnancy-associated-plasma protein-A
(PAPP-A) is the earliest change detectable in the
future dominant follicle.
PAPP-A is a protease and increase intrafollicular IGFI concentrations.
Follicular waves
Increased IGF-I acts together with FSH to increase
estradiol synthesis.
It is noteworthy that estradiol stimulates the
production of IGF-1 and IGF-1 stimulates the
production of estradiol.
Follicular waves
In the early estrogenic follicle some changes occur for
receptors:
The mRNAs for the FSH receptor and aromatase are
elevated within the granulosa layer.
Theca cells have increased abundances of LH receptor and
17α-hydroxylase.
Follicular waves
Two cell, two-gonadotropin theory of ovarian steroidogenesis
Follicular waves
Dynamic changes are evident within the inhibin
family:
In estrogen-active follicle the large molecular weight
inhibins (i.e., >160 kDa) are elevated.
In estrogen-inactive follicles the smaller inhibins (32 to 34
kDa) are increased.
Follicular waves
FSH secretion by pituitary gland will reduce by:
The increased secretions of estradiol
The increased secretion of large MW inhibin
Lack of FSH prevents further growth of subordinate
follicles, which are also nonestrogenic due to low
concentrations of free IGF-I.
Follicular waves
Once the dominant follicle reaches 10 mm its
granulosa cells begin to express LH receptors.
Continued growth and dominance of the dominant
follicle beyond10 mm appears to be dependent upon
LH secretion.
Follicular waves
+
*
*
+
*
+
*
+
*
+
+
*
*
*
*
Ovarian follicular and corpus luteum development correlated with endocrine
changes during the bovine estrous cycle. E2 = Estradiol; IGFBP-4 and -5 = insulinlike growth factor binding proteins 4 and 5; OvF = ovulatory follicle.
Follicular waves
Dominant follicles continue to grow for a few days
after selection.
If there is an LH surge the dominant follicle continues
to grow and the oocyte within undergoes:
Final maturation
Culminating in follicle rupture
Ovulation
Follicular waves
Final maturation includes:
Expansion of the cumulus cover
Disruption of the contact between the corona radiata cells
and the oocyte membrane
Perivitelline space formation
Increase lipid content in oocyte cytoplasm
Decrease golgi compartment in oocyte cytoplasm
Follicular waves
Final maturation includes:
The cortical granules are aligned just inside the oocyte
membrane
The chromosomes condense and progress through the final
stages of meiosis I and arrest at metaphase of meiosis II
Follicular waves
The peak and average plasma concentrations of FSH
and inhibin A are lower in the two non-ovulatory
waves than a three-wave cycle
Follicular waves
Higher fertility in three-wave cycles could be due to:
A shorter interval for development of the ovulatory follicle
(Townson et al, 2002).
Delayed regression of the corpus luteum.
Progesterone
Follicular Size
Atresia
Recruitment
Dominance
Ovulation
Selection
FSH Sensitive Pool
Ovulation
9
16
Day After Ovulation
21
Ovulation
Ovulation takes place about 10-14 hours after the end
of oestrus.
The gonadotropin surge is important for ovulation:
Increase progesterone production
Increase estrogen production
Increase prostaglandins (PGE2 & PGF2α)
Corpus luteum formation
In
its
early
stages
of
growth
the
corpus
haemorrhagicum is difficult to palpate.
The corpus luteum (CL) is palpable at about five
days post ovulation.
Corpus luteum formation
It frequently has a distinct crown:
About ½ cm in diameter
About ½ cm high
The corpus luteum enlarges progressively to two to
three cm by day-8 or 9 and has a liver like
consistency.
Corpus luteum formation
Actually the CL is made up two cell groups:
The large luteal cells, which originated from granulosa
cells.
The small luteal cells which originated from theca cells.
The luteal cells are steroidogenic and secrete
progesterone.
Corpus luteum formation
Progesterone has the following functions during
pregnancy:
It prevents the cow from coming on heat.
The function of the hormone oxytocin is blocked.
It regulates the changes in the mucous membranes in the
uterus.
It plays a role in the formation of udder tissue.
Some research papers associated to this lecture
1.
Beg, M. A. et al. 2002. Follicle Selection in Cattle: Dynamics of follicular
fluid factors during development of follicle dominance. Biology of
Reproduction. 66: 120–126.
2.
Bisinotto, R. S. Et al. 2010. Follicular wave of the ovulatory follicle and
not cyclic status influences fertility of dairy cows. J. Dairy Sci. 93 :3578–
3587.
3.
Rýfat, M. et al. 2005. Evaluation of the corpus luteum size throughout
the cycle by ultrasonography and progesterone assay in cows. Turk. J.
Vet. Anim. Sci. 29: 1311-1316.