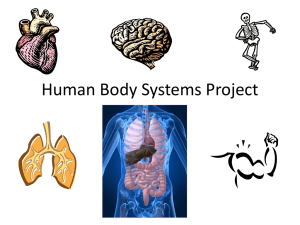
OVERVIEW OF GIT FUNCTIONS
& REGULATION
1
OBJECTIVES
To know the components of GIT and their
functional significance.
Emphasize the functional importance of four
layers of GIT.
Outline four basic digestive processes.
Recognize the importance of regulatory factors
that controls digestive functions.
2
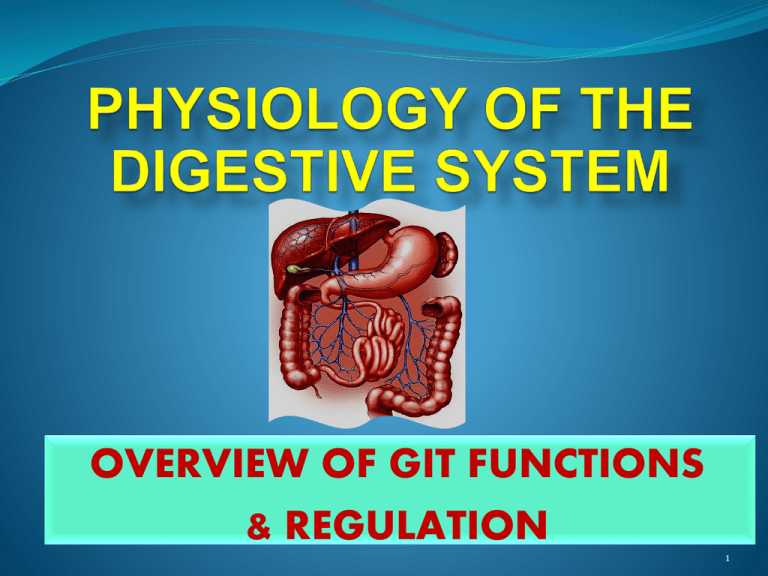
DIGESTIVE SYSTEM (GIT)
Digestive Tract:
Mouth
Pharynx
Esophagus
Stomach
Small intestine
- Duodenum
- Jejunum
- Ileum
Large intestine
- Cecum
- Appendix
- Colon
- Rectum
Anus
Accessory Digestive Organs:
Salivary glands
Exocrine pancreas
Biliary system
- Liver
- Gall bladder
3
DIGESTIVE SYSTEM
Digestive tract is 4.5 m (15 feet) in normal
contractile state.
Lumen is continuous
from mouth to anus
and hence is
continuous with
external environment.
4
DIGESTIVE SYSTEM
Primary Function:
Transfer nutrients, water, and electrolytes from
ingested food into body’s internal environment.
Food is ingested – digested – absorbed – distributed
and used.
The Digestive System Performs Four Functions:
1- Motility
2- Secretion
3- Digestion
4- Absorption
5
FUNCTIONS OF THE DIGESTIVE SYSTEM
1- Motility:
Muscular contractions that mix and move
forward the contents of the digestive tract.
Two Types of Digestive Motility:
Propulsive (peristaltic) movements
Mixing (segmenting) movements
6
Types of Digestive Motility
1- Propulsive (= Peristaltic) Movements:
Push contents forward through the digestive tract.
Velocity with which contents are moved forward (rate
of Propulsion) varies in different regions of GIT,
depending on functions of that region. For example:
* Rapid movements in esophagus.
* Slow movements in Small intestine.
7
GIT Motility
Movements of contents through most of digestive
tract is accomplished by contraction of smooth
muscles (involuntary component) except:
1- Mouth (chewing).
2- Early part of esophagus (swallowing).
3- External anal sphincter (defecation).
In these regions, motility involves skeletal muscle
(voluntary component).
8
Types of GIT Motility
2- Mixing (=segmenting) Movements:
Serve Two Functions:
1- Mixing food with digestive juices & hence promotes
digestion of foods.
2- Facilitates absorption by exposing all parts of intestinal
contents to absorbing surfaces of digestive tract.
9
Segmentation
Gut law: Distension of gut leads to
peristaltic wave starting at the point
of distension & proceeds anal wards.
10
FUNCTIONS OF THE DIGESTIVE SYSTEM
2- Secretions:
Digestive juices are secreted in to GIT lumen
by exocrine glands (through ducts).
Digestive secretions consists of:
1- Water.
2- Electrolytes.
3- Specific organic constituents (enzymes, bile
salts, or mucus) important in digestive
process.
11
GIT SECRETIONS
Secretions are released into the digestive tract lumen on
appropriate neural or hormonal stimulation.
Normally absorbed in one form or another into blood
after their participation in digestion.
Total quantity of fluid that is secreted from digestive
glands into GIT lumen equals 7 liters / day.
Failure of absorption of digestive juices, as in diarrhea &
vomiting results in loss of fluid (dehydration).
12
13
FUNCTIONS OF THE DIGESTIVE SYSTEM
3- Digestion:
Biochemical
breakdown of structurally complex
foodstuffs into smaller, absorbable units by enzymes
produced within GIT.
Complex food stuffs:
i). Carbohydrate
ii). Proteins
iii). Fats
These are large molecules, therefore, they are digested
and then absorbed into the blood or lymph.
14
i). CARBOHYDRATES
Carbohydrates are absorbed as monosaccharides e.g.
glucose, fructose, and galactose.
Cellulose is a polysaccharide found in plants. It can not be
digested, therefore, works as bulk or ingestible fibers.
ii). PROTEIN
Proteins are absorbed as
- Amino acids.
- Small polypeptides.
iii). FAT
Fat are absorbed as
- Monoglyceride [glycerol with one fatty acid].
- Free fatty acid.
15
FUNCTIONS OF THE DIGESTIVE SYSTEM
4- Absorption:
In the small intestine, digestion is completed & most absorption
occurs. The small intestine, with its epithelial folds, villi, and
microvilli, has an internal surface area of 200 m2.
Through process of digestion, small absorbable units resulting
from digestion, along with water, vitamins, and electrolytes are
transferred from digestive tract lumen into blood or lymph.
Total quantity of fluid that must be absorbed: 2 L (ingested)
+ 7 L (secreted) = 9 liters / day.
16
DIGESTIVE TRACT WALL
GIT wall has same general structure throughout length
from esophagus to anus (with some local characteristic
variations).
Four major tissue layers:
Mucosa (Innermost
layer).
Submucosa.
Musculosa (Muscularis externa).
Serosa (Outer
layer).
17
Layers of Digestive Tract Wall
18
19
MUCOSA
Lines luminal surface of digestive tract.
Highly folded surface greatly increases absorptive
area.
Of Three layers:
1- Mucous membrane
2- Lamina propria
3- Muscularis mucosa
20
MUCOSA
1- Mucous Membrane:
Inner epithelial layer serves as a protective surface.
Modified in particular areas for secretion and
absorption.
Contains:
Exocrine gland cells secrete digestive juices.
Endocrine
gland cells secrete blood-borne
gastrointestinal hormones.
Epithelial cells specialized for absorbing digestive
nutrients.
21
MUCOSA
2- Lamina Propria:
Middle layer of connective tissue on which epithelium rests.
Houses gut-associated lymphoid tissue (GALT)
Important in defense against disease-causing intestinal
bacteria.
3- Muscularis Mucosa:
Sparse layer of smooth muscle, contraction modifies the
pattern of surface folding.
22
SUBMUCOSA
Thick layer of connective tissue.
Provides digestive tract with distensibility and
elasticity.
Contains larger blood and lymph vessels.
Contains Submucosal nerve plexus or
Meissners
Secretion.
plexus
that
regulates
GIT
23
MUSCULOSA (= MUSCULARIS EXTERNA)
Major smooth muscle coat of digestive tube. In most
areas, it consists of two layers:
1- Circular layer (Inner layer):
Contraction decreases diameter of lumen.
2- Longitudinal layer (Outer layer):
Contraction shortens the tube.
Together, contractile activity of these layers produces
propulsive and mixing movements.
Myenteric nerve plexus lies between the two muscle
layers that controls Movements of GIT.
24
SEROSA
Outer connective tissue covering of GIT.
Secretes serous fluid (watery & slippery fluid) that
Lubricates and prevents friction between digestive
organs and surrounding viscera.
Continuous with mesentery throughout much of the
tract. This Attachment provides relative fixation and
supports digestive organs in proper place while still
allowing them freedom for mixing and propulsive
movements.
25
REGULATION OF GIT FUNCTION
Digestive motility and secretion are carefully
regulated to optimize the digestion.
Four factors are involved in regulating digestive
system function:
1- Autonomous smooth muscle function.
2- Intrinsic local nerve plexuses.
3- Extrinsic autonomic nerves.
4- Gastrointestinal hormones.
26
1- AUTONOMOUS SMOOTH MUSCLE FUNCTION
In the wall of GIT, some specialized smooth
muscle cells are pacemakers cells known as
interstitial cells of Cajal.
These cells lie in between circular & longitudinal
layer of smooth muscles.
These are self-excitable cells that display
rhythmic spontaneous variations in membrane
potential known as slow wave potential or
basic electrical rhythm (BER).
27
Autonomous Smooth Muscle Function
28
Slow Wave Potential
If
slow
wave
potential
(slow
depolarization)
reaches threshold, action potentials are triggered
resulting in rhythmic cycles of contraction.
Reaching threshold depends on mechanical, neural
and hormonal factors that influence starting point of
slow wave potential (e.g. presence of food bolus in
GIT).
29
Slow Wave Potential
The rate of self-induced contractile activity
depends on inherent rate established by involved
pacemaker.
The intensity of contractions depends on number
of action potentials occurring at peak of slow
wave.
Greater the number of contraction, the higher the
cytosolic calcium, the stronger the contraction.
30
2- INTRINSIC NERVE PLEXUSES
Submucosal plexus and myentric plexus, together are
often termed as Enteric
nervous system.
Primarily coordinate local activity in GIT.
Intrinsic nerve plexuses can affect all functions of
digestive tract, i.e. motility, secretion of digestive
juices and gastrointestinal hormones.
Intrinsic nerve plexuses activity can be influenced by
endocrine, paracrine and nerve signals.
31
Submucosal
nerve
plexus
or
Meissners plexus that regulates GIT
Secretion.
Myenteric nerve plexus lies between
the two muscle layers that controls
Movements of GIT.
32
3- EXTRINSIC NERVES (AUTONOMIC)
Both branches of ANS influence GIT motility
& secretion either by:
Modifying activity of intrinsic nerve plexuses.
Altering level of GIT hormones secretion.
Directly acting on smooth muscle and glands.
Sympathetic inhibits the motility and secretion
and parasympathetic increases both.
Extrinsic nervous system coordinates activity
between different regions of GIT.
33
Parasympathetic
Sympathetic
(Dominant)
* Vagus supplies from the * Greater splanchnic nerve:
esophagus till 1st half of large
from LHCs of lower 8 Thoracic
intestine.
segments.
* Lesser splanchnic nerve:
* Sacral (S2, 3, 4) segments supply
from LHCs of upper 2 Lumbar
the rest of GIT till anal region.
segments.
1. Contraction of GIT wall
Relaxation of sphincters.
& 1. Relaxation
of GIT wall
Contraction of sphincters.
2. Increase GIT secretions.
2. Decrease GIT secretions.
3. VD.
3. VC.
34
&
GASTROINTESTINAL HORMONES
Endocrine gland cells are tucked within mucosa of
certain regions of GIT that release hormones into blood
on appropriate stimulation.
These hormones acts on other areas of GIT and exert
either stimulatory or inhibitory influences on smooth
muscle and exocrine cells.
E.g. CCK, Secretin, Gastrin……………etc
35
Pathways Controlling GIT activities
36
GIT RECEPTORS & REFLEXES
(i)
Chemoreceptors: sensitive to chemical changes in lumen.
(ii) Mechanoreceptors: sensitive to stretch on the wall.
(iii) Osmoreceptors: sensitive to osmolarity of luminal
contents.
Stimulation of these receptors causes neural reflexes or
secretion of hormones which effect motility and secretion of
digestive juices.
In GIT, two types of reflexes occur:
1. Short reflexes: local enteric reflex in wall of digestive tract.
2. Long reflexes: between CNS and Digestive system.
37
REFERENCES
Human Physiology, Lauralee Sherwood, seventh
edition.
Text book Physiology by Guyton &Hall,11th edition.
Text book of Physiology by Linda S. Contanzo,
third edition.
Physiology by Berne and Levy, sixth edition.
38
Thank you
39