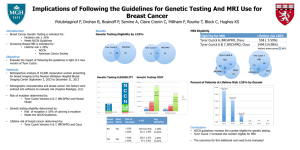
Oncologic Genetic
Syndromes and Screening
Brad T Tinkle, MD PhD
Director of AMG Genetics
6th Annual Trends in Hematology/Oncology
March 2, 2013
Disclosures
• No financial disclosures
Objectives
• Review the role of genetic susceptibility in
various cancer types
• Discuss the genetic syndromes and testing
options of various cancer types
• Describe the role that genetics health
professionals offer
Genetics in Cancer
• 5-10% of all malignancies are due to highly
penetrant hereditary cancer predisposition
syndromes [Ballinger, 2012]
• Over 400 cancer-related genes have been
identified
– May account for many familial cancers
– Caution! Current clinical testing may include
some of these genes of lower-risk
http://www.sanger.ac.uk/genetics/GCP/Census
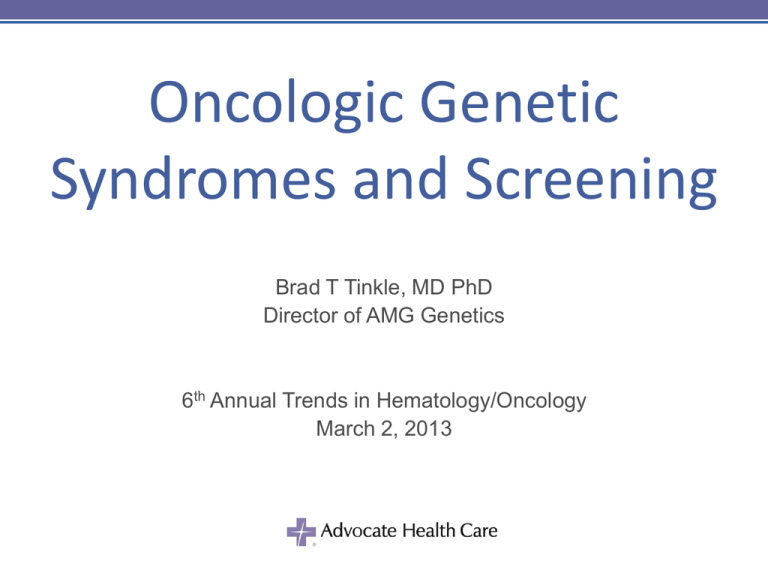
Breast Cancer
•
•
•
•
Most prevalent type of cancer in women
2nd leading cause of cancer death in the US
New cases in 2012: 229,060 (estimated)
Deaths in 2012: 39,920 (estimated)
15%-20%
5%–10%
Sporadic
Family clusters
Hereditary
Ovarian Cancer
• 22,000 newly diagnosed in the US
annually
• 1.4% lifetime risk
• ~45% 5-year survival rate
• 4.6x RR if mother had ovarian cancer and
1.6x RR is sister [Ziogas et al., 2009]
Sporadic
Hereditary
5%–10%
Endometrial Cancer
• 47,130 newly diagnosed in 2012 (estimated)
• Lifetime risk is estimated to be 2.5%
• 8,010 estimated deaths in 2012
• Most common heritable form is Lynch syndrome
(a.k.a. hereditary non-polyposis coli) which
represents 2-3% of all cases
• May also be related to Cowden (PTEN
Hamartoma Tumor syndrome) and PeutzJeghers
Colorectal Cancer
•
•
•
•
•
4th most common cancer diagnosis in US
1 in 20 Americans will develop CRC
In 2012, expected number of new cases: 143,460
Expected deaths due to CRC: 51,690
Death rate is declining – early detection and prevention
5%
General population
15%-20%
Personal h/o CRC
15%–40%
Inflammatory bowel disease
70%–80%
HNPCC mutation
>95%
FAP
0
20
40 60 80
Lifetime risk (%)
100
Gastric Cancer
•
•
•
•
Estimated 21,320 new diagnoses in the US (2012)
Estimated 10,540 deaths in the US (2012)
4th leading cause of cancer deaths worldwide
5 year survival of 20%
• 3-10% are hereditary
–
–
–
–
–
–
–
Hereditary diffuse gastric cancer
Hereditary breast/ovarian cancer
Lynch syndrome
Li-Fraumeni syndrome
Familial Adenomatous Polyposis
Juvenile polyposis
Peutz-Jeghers
Pancreatic Cancer
• Estimated 43,920 new diagnoses in the US (2012)
• 4th leading cause of cancer-related deaths in the
US
– Estimated deaths 37,390 in 2012
• 5-10% are hereditary
– Associated with familial forms of pancreatitis
– Breast-ovarian cancer syndrome (BRCA2 and PALB2)
– Familial multiple melanoma with 0.6-31% lifetime risk
• Higher risk if first-degree relative with pancreatic ca.
– Lynch syndrome 0.4-4% lifetime risk
– Peutz-Jeghers 8-36% risk
Solomon S et al. Cancer J 2012;18:485-91.
Bartsch DK, et al. Nat Rev Gastroenterol Hepatol 2012;9:445-54.
Melanoma
• 76,250 new cases in the US in 2012
(estimated)
• 9,180 estimated attributable deaths in 2012
• ~10% hereditary
– Familial atypical mole-melanoma syndrome
• Accounts 5-7% of all melanoma
– May be associated with HBOCS (BRCA2)
Prostate Cancer
• Most frequently diagnosed cancer in US men 36% of all cancers
• Lifetime risk for men in US: 15-20%
• 241,000 new cases diagnosed in 2012
(estimated)
• 5-10% is heritable
– ~40% under 55y
– Higher in families with
breast/ovarian cancer
5-10%
Cancer Syndromes
Genetic Syndromes
• There are those with dysmorphic or characteristic
features that also have a tumor predisposition
–
–
–
–
–
–
–
–
–
–
Beckwith-Wiedemann syndrome
Bloom syndrome
Diamond-Blackfan
Down syndrome
Fanconi anemia
Neurofibromatosis type I and II
Gorlin syndrome (basal cell nevus syndrome)
Rothmund-Thomson syndrome
Tuberous sclerosis
Werner syndrome
Hereditary Breast Cancer Syndromes
•
•
•
•
•
Hereditary breast-ovarian cancer (5% of all breast cancer)
Li-Fraumeni (~1%)
PTEN hamartoma (<1%)
Peutz-Jeghers (<1%)
Hereditary diffuse gastric cancer syndrome
• Also:
–
–
–
–
–
–
Autoimmune lymphoproliferative (ALPS)
Ataxia telangiectasia
Bloom syndrome
Familial melanoma
Werner syndrome
Xeroderma pigmentosa
Heritable Ovarian Cancer
• Lifetime risk varies from 12-60%
• Often earlier than those of the general
population
• 6-15% breast/ovarian cancer syndrome
• Also includes:
– Lynch syndrome
– Peutz-Jeghers syndrome
Hereditary CRC Syndromes
• Accounts for 5-10% of all CRC cases
• Polyposis types:
– Adenomatous
• Familial adenomatous polyposis (<1%)
• MYH-associated polyposis (<1%)
– Hamartomatous
• Juvenile polyposis (<1%)
• Peutz-Jeghers
• Cowden (PTEN)
• Lynch syndrome (2-3%)
– Often not polyps but can have and still increased cancer risk
• Seldom in:
– Bloom, hereditary diffuse gastric cancer syndrome, and Li-Fraumeni
Breast/Ovarian Cancer Syndrome
• Primarily BRCA1 and BRCA2
• Frequency of carriers 1 in 300 (BRCA1)
to 1 in 800 (BRCA2)
– Ashkenazi Jewish (1 in 40)
• Accounts for >90% of families with
breast and ovarian cancers
Breast-Ovarian Cancer Syndrome
• Of those with BRCA1 mutations:
– 50-80% risk of invasive breast carcinoma-females
• ~1% risk for males
– Up to 60% risk of serous ovarian carcinoma
– Up to 30% risk of prostate cancer
– 1-3% risk of pancreatic
• Of those with BRCA2 mutations:
– 40-85% risk of invasive breast carcinoma-females
• 6-7% risk for males
– Up to 35% risk of serous ovarian carcinoma
– Up to 39% risk of prostate cancer
– 2-7% risk of pancreatic
Van der Kolk et al. Breast Cancer Res Treat 2010;124:643-51.
HBOCS- Tumor Characteristics
• Breast tumor often originates from breast
epithelia cells
– Basal keratin positive
• More commonly a/w with invasive lobular and
ductal carcinoma as well as DCIS
• More likely to be high-grade malignancies and
lymph node positive
– Estrogen receptor negative
– Progesterone receptor negative
– Her2/neu negative
• >90% ovarian serous adenocarcinoma
Li-Fraumeni Syndrome
• Prevalence: Up to 1 in 20,000
• Inheritance: Autosomal dominant
• Gene: TP53
• Lifetime risk of cancer:
–
–
–
–
–
50% by age 30-35y
90% by 60y
Female lifetime risk is 90%
Male lifetime risk is 70%
57% risk of a second primary
LFS- Diagnostic Criteria
•
•
•
Proband with sarcoma <45yoa
First-degree relative with any cancer <45yoa
First- or second-degree relative with any cancer <45yoa or sarcoma
at any age
•
LFS-related cancers include:
– Breast cancer
• Most common LFS-related cancer
• Lifetime risk 49%
• <1% overall of total breast cancers; however, more likely with diagnosis <30yoa
(up to 7%)
• More likely to be triple positive
– Soft tissue and bone sarcomas
– Brain tumors
• Choroid plexus tumors
– Adrenocortical carcinoma
• LFS accounts for 80% of childhood ACC
– Leukemia
– Bronchoalveolar cancer
NCCN 1.2012 Guidelines: Genetic/Familial High-Risk Assessment: Breast and Ovarian
Masciari S et al. Breast Cancer Res Treat 2012;133:1125-30.
Li-Fraumeni Syndrome
Noncarrier
Bilateral Breast, 40
TP53carrier
Affected with
cancer
50
Breast, 40
Leukemia, 33
Osteosarcoma, 42
Breast,
35
Soft tissue
sarcoma, 7
ASCO
Brain tumor, 32
Leukemia, 6
PTEN Hamartoma Syndrome
• A.k.a Cowden syndrome, BannayanRiley-Ruvalcaba syndrome
• Prevalence: 1 in 200-250,000
Planchon S M et al. J Cell Sci 2008;121:249-253
• Inheritance: Autosomal dominant
• Gene: PTEN
PTEN Hamartomatous Syndrome
•
25-85% lifetime risk of breast cancer
– <1% overall of all breast cancer
– Average age of diagnosis 38-46y
•
5-28% lifetime risk of endometrial cancer
•
3-35% lifetime risk of non-medullary thyroid (follicular) cancer
•
40-93% lifetime risk of polyps (hamartomatous)
– 9% lifetime risk of CRC
– Ganglioneuroma
– 13% of PTEN mutation-associated Cowden syndrome patients developed CRC
<50yoa
•
Strongly a/w Lhermitte-Duclos (dysplastic gangliocytoma)
•
May also be associated with renal cancer and melanoma
PTEN Physical Features
• Macrocephaly
• Facial papules
(trichilemmomas)
– ≥2 pathognomic?
• Oral mucosal
papillomatosis
– 99% incidence
• Acral keratoses
•Macrocephalic
•No unusual skin lesions
or pigmentation
•BrCa at 42yoa
Breast Cancer- When to Refer
• Breast cancer <50yoa
• Triple negative breast cancer
– 11-28% have BRCA1 mutations
• Two breast cancer primaries in a single individual
– ~30% risk of second primary in 10 years for BRCA1/2
• Breast or ovarian cancer at any age in those of
Ashkenazi Jewish ancestry
• Breast cancer at any age and…
– ≥1 close relative* with breast cancer <50yoa
– ≥1 close relative* with epithelial ovarian cancer at any age
– ≥2 close relatives* with breast cancer and/or pancreatic
cancer at any age
NCCN Guidelines: Genetic/Familial High-Risk Assessment: Breast and Ovarian
*Includes third degree relatives
When to Refer (2)
• A combination of breast cancer with one or more of the
following in close relatives:
–
–
–
–
–
–
–
–
Thyroid cancer
Sarcoma
Endometrial cancer
Pancreatic cancer
Brain tumors
Diffuse gastric cancer
Dermatologic manifestations and/or macrocephaly
Leukemia/lymphoma
• Ovarian cancer with a family history of breast and/or
ovarian cancer
• Male breast cancer
– 4-14% due to BRCA2
NCCN Guidelines: Genetic/Familial High-Risk Assessment: Breast and Ovarian
Lynch Syndrome
• A.k.a. hereditary nonpolyposis colorectal cancer; includes MuirTorre (sebaceous adenomas)
• Incidence: 1 in 440
MSH6
• Accounts for:
– 2-10% of all CRC
– 2% of ovarian cancers
– 2-5% of endometrial
MSH2
• 9-20% of those <50y
• Autosomal dominant
PMS1
• Multiple genes (MLH1, MSH2, MSH6,
MSH3, PMS1, PMS2, TACS (EPCAM), TD1)
Chr 2
Lynch Syndrome- Cancer Risks
• 22-92% lifetime risk of CRC
– Mean age of 44yo (MLH1 or MSH2)
• 6-19% lifetime risk of gastric cancer
– More common in Japan
• 20-70% risk of endometrial cancer
– MSI-IHC testing recommended
•
•
•
•
4-12% risk of ovarian cancer
18% hepatobiliary
5-10% urinary tract cancers
May also develop:
– Small bowel, pancreatic cancer
– Skin: (sebaceous carcinomas, keratocanthomas,
and epitheliomas)
– Brain tumors, especially glioblastoma
Lynch Syndrome- Amsterdam II
• Amsterdam II criteria (all have to be met):
– ≥3 family members, one of whom is a firstdegree relative of the other two, with HNPCCrelated cancers (CRC, endometrial, stomach,
small bowel, hepatobiliary, renal pelvic, or
ureteral cancer)
– Two successive generations
– One or more HNPCC-related cancer
diagnosed before 50yoa
Used to make a clinical diagnosis of Lynch syndrome and does not
take into account all possible Lynch syndrome-related tumors
Lynch Syndrome- Bethesda
• Modified Bethesda criteria (any of the following):
– CRC diagnosed <50yoa
– Presence of synchronous or metachronus CRC, or
other HNPCC-related tumors (CRC, endometrial,
gastric, ovarian, pancreatic, ureteral, biliary tract and
brain tumor) regardless of age
– CRC with microsatellite instability-high <60yoa
– CRC in ≥1 first-degree relatives with HNPCC-related
tumor with one cancer <50yoa
– CRC in ≥2 first- or second-degree relatives at any age
Used to guide additional testing such as MSI/IHC
Lynch Syndrome- MSI
• Microsatellite instability
– Microsatellites are highly-repetitive DNA
sequence
– Susceptible to dynamic changes if not for the
mismatch repair genes
• MSI-high= instability >30% of cells
• MSI-low= instability <30% of cells
• MSI stable= no evidence of MSI
Lynch- MSI Caveats
• 90% of inherited tumors are MSI-high
• MSI-high can be caused by many somatic
(not inherited) events, most notably BRAF
methylation/mutation
• Some Lynch syndrome patients will have
MSI-low or MSI-stable testing
• Immunohistochemistry for mismatch repair
proteins (MLH1, MSH2, MSH6, PMS1,
PMS2) recommended as adjunctive analysis
Lynch- Genetic Testing
• If met Amsterdam II criteria, recommend genetic
testing
• If met Bethesda, testing of the tumor sample by
MSI/IHC recommended initially with
consideration of genetic testing
• If MSI-high and IHC positive (i.e. absence of one
of the proteins) the probability of Lynch is high
therefore genetic testing recommended
Familial Adenomatous Polyposis
• A.k.a Turcot or Gardner syndromes
• 1 in 6-20,000 live births
• Due to genetic defect in APC
– If negative, consider MYH testing
• Accounts for <1% of all CRC
• Hallmark is the adenomatous polyposis
– 20-100% penetrance in the duodenum
• 100% lifetime risk of CRC with average
age of cancer diagnosis of 39y
FAP: Age and Development
of Adenomas and CRC
100
FAP
Adenomas
80
% of patients
with neoplasia
CRC
60
40
General population
20
0
20
Bussey HJR. Familial Polyposis Coli, 1975
Petersen GM et al. Gastro 100:1658, 1991
40
60
Age
80
FAP- Associated Risks
• 4-12% lifetime risk of other intestinal cancers
– 0.5-2% gastric
– 5% duodenal
• 1-2% risk of pancreatic and non-medullary thyroid
• 0.6% risk of hepatoblastoma before 6yoa with 1-2% lifetime
• 10-30% lifetime risk of desmoid tumors
• Also a/w medulloblastoma as well as gliomas and ependymoma
• CHRPE- congenital hypertrophy of the retinal pigmented
epithelium
Peutz-Jeghers Syndrome
•
•
•
•
Prevalence: 1 in 25-280,000
Inheritance: Autosomal dominant
Gene: STK11
Hamartomatous and adenomatous
polyposis especially of the small intestine
• 37-93% lifetime risk of cancer
– 38-66% risk of gastrointestinal
• 2-39% CRC
• 29% gastric
• 11-36% pancreatic
–
–
–
–
30-54% risk of breast cancer
Lifetime uterine cancer risk is 9-21%
Lung 15% lifetime risk
Includes ovarian and sex cord tumors
Labial and oral mucosal
hyperpigmentation- may
fade with time
Letterman’s Top 10 Genetic Cancers
1. Adrenocortical carcinoma (LiFraumeni and BWS)
2. Carcinoid tumors (MEN I)
3. Diffuse gastric cancer (Hereditary Diffuse Gastric
Cancer)
4. Fallopian tube (HBOCS)
5. Leiomyosarcoma (HLRCC, Lynch, Rb)
6. Medullary thyroid carcinoma (MEN 2)
7. Paraganglioma/pheo (MEN 2, VHL, NF1, PGL)
8. Renal cell carcinoma- chromophobe, hybrid
oncocytotic, oncocytoma histology (Britt-HoggDube)
9. Sebaceous carcinoma (Lynch)
10. Sex cord tumor with annular tubule (PJS)
Banks et al. Familial Cancer 2013;12:1-18.
Genetic Services
When to Suspect Hereditary Cancer Syndrome
• Cancer in 2 or more close relatives
• Early age at diagnosis
• Multiple primary tumors
• Bilateral or multiple cancers
• Constellation of tumors consistent with
specific cancer syndrome (e.g. breast and
ovary)
• Evidence of autosomal dominant
transmission
Genetic Counseling- A Multistep Process
• Detailed and extensive family history
• Ethnic-risk evaluation
• Cancer cluster recognition
– Breast-ovarian-pancreatic
– Macrocephaly-skin lesions-breast cancer
•
•
•
•
•
•
•
•
Gather necessary medical records
Determine who best to test
Insurance and insurability questions
Test selection
Pre- and post-test counseling
Psychosocial support
Test result interpretation
Help with informing family members of risk
Taking a Cancer Family History
• Obtain at least a three-generation pedigree
• Ask about all individuals in the family
and record:
– Age at cancer diagnosis, age at and cause of
death
– Primary vs metastatic cancer
– Precursor lesions, bilateral cancer
– Physical features
– Birth defects
– Other diagnoses
• Record ethnicity and race
Clarify Family History
Verbally reported pedigree
Stomach Ca
Bone Ca
d. 59
Prostate
Ca
Revised pedigree based on
pathology reports
Ovarian Ca
dx 43, d. 49
Breast Ca BPH
dx 45 dx 54
d. 59
Testing The More Appropriate
Person in the Family
Colon Ca, 42
Colon Ca, 38
d.45
Test first, if possible
Colon Ca,
45
Person seeking
counseling (proband)
If a mutation is found in an affected person, testing
will be more informative for other family members
ASCO- Genetic testing
• A personal or family history suggesting
genetic cancer susceptibility
• Test can be adequately interpreted and put
into clinical context
• Results will aid in the diagnosis OR influence
the management of the patient/family
Informed Consent: Benefits of
Genetic Testing
• Improved cancer risk management
• Relief from uncertainty and anxiety about
cancer risk
• Information for individual and family members
• Lifestyle decision making
Informed Consent: Potential Risks
of Genetic Testing
•
Psychological distress
–
–
–
–
Anxiety/fear
Guilt
Depression
Grief
•
Loss of privacy
•
Discrimination by employers and insurers
•
Change in family dynamics
•
False sense of security
Informed Consent: Limitations of
Genetic Testing
• Not all mutations are detectable
• Uncertain significance of some mutations
• Negative result is fully informative only if
mutation has been identified in family
• Results indicate probability, not certainty, of
developing cancer
• Unproven efficacy of most interventions
ASCO
Possible Testing Results:
Beyond Positive or Negative
• Variants of Uncertain Significance (VUS)
• Amino acid substitutions
• Frequency 11% at Myriad, > in African
American
• Determine significance several ways:
–
–
–
–
Observed with deleterious mutation
Population studies (frequency >1%)
Biochemical, evolutionary models
Linkage in large families
ASCO
Implications For The Entire Family
• Consider the impact of testing on all family
members
• Ultimately, testing is the individual’s choice
ASCO
THANK YOU!
References
•
•
•
•
•
•
•
•
•
•
•
Shannon KM, Chittenden A. Genetic testing by cancer: breast. Cancer J 2012;18:310-319.
Jasperson KW. Genetic testing by cancer: colon (polyposis syndromes). Cancer J
2012;18:328-333.
Senter L. Genetic testing by cancer: colon (nonpolyposis syndromes). Cancer J
2012;18:334-337.
Daniels MS. Genetic testing by cancer site: uterus. Cancer J 2012;18:338-342.
Chan-Smutko G. Genetic testing by cancer: urinary tract. Cancer J 2012;18:343-349.
Axilbund JE, Wiley EA. Genetic testing by cancer: pancreas. Cancer J 2012;18:350-354.
Chun N, Ford JM. Genetic testing by cancer site: stomach. Cancer J 2012;18:355-363.
Pilarski R, Nagy R. Genetic testing by cancer: endocrine system. Cancer J 2012;18:364371.
Gabree M, Seidel M. Genetic testing by cancer: skin. Cancer J 2012;18:372-380.
Schneider KA. Counseling about cancer: strategies for genetic counseling, 3rd ed. WileyBlackwell, 2012.
NCCN Clinical Practice Guidelines in Oncology (NCCN Guidelines) “Genetic/Familial
High-Risk Assessment: Breast and Ovarian”, version 1.2012.