Breast Cancer - Texarkana College
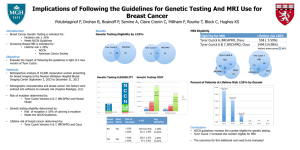
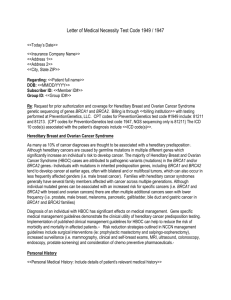
advertisement

Hereditary Breast & Ovarian Cancer Syndrome HBOC Tammy McKamie RN MSN OCN Cancer Genetics Educator Clinical Oncology Patient Navigator Objectives • Understand the application of genetics in the nursing assessment. • Identify risk factors (red flags) that potentially increase a person’s risk for hereditary cancer. • Differentiate between sporadic and inherited cancer. • Summarize surveillance and medical management options for individuals and families based on possible genetic testing outcomes. Objectives • Analyze the impact of genetic conditions on patients and their families. • Discuss the ethical, legal, and social issues involving genetic education and testing. • Evaluate the pros and cons of genetic testing Human Genome Project • Began in 1990, • A 13-year Project • Coordinated by the U.S. Department of Energy and the National Institutes of Health. Genetic Testing Available: • Breast Cancer • Ovarian Cancer • Colorectal Cancer • Endometrial (uterine) Cancer • Melanoma Hereditary Breast & Ovarian Cancers 90% 7-10% Sporadic Hereditary Cells have Two Copies of Each Chromosome Father Mother x Y x Child x TUMOR SUPPRESSOR GENES MSH6 MLH2 MSH1 APC EPCAM2 PMS2 BRCA2 p16 BRCA1 x Cancer arises when both copies of tumor suppressor genes are inactivated Tumor develops In hereditary cancer, one damaged gene is inherited. 2 normal genes 1 normal gene 2 damaged 1 damaged gene genes 1 normal gene 2 damaged 1 damaged gene genes Tumor develops Sporadic vs Inherited Sporadic – No clear pattern of inheritance Common types of cancer diagnosed @ standard ages > 50 y/o Inherited – Multiple generations affected with same type of cancer Diagnosed @ young age < 50 y/o Autosomal Dominant Inheritance Father with mutation on one chromosome Each child has a 50% chance of inheriting an Autosomal Dominant disorder RED FLAGS For Hereditary Cancer Syndromes Young age of cancer (<50) in patient or family Breast Colon Endometrial (uterine) RED FLAGS For Hereditary Cancer Syndromes Multiple family members with the same cancer Breast/ovarian Colon/Endometrial Melanoma/pancreatic RED FLAGS For Hereditary Cancer Syndromes Rare cancers in patient or family Ovarian cancer any age Male breast cancer Individuals with multiple primary cancers Signs of Sporadic Cancer d. 65 Prostate ca dx 59 78 d. 80 heart 70 d. 70 heart d. 76 COPD 76 Cervical ca dx 56 58 Breast ca dx 57 76 70 Lung ca dx 60 56 49 75 Signs of Hereditary Cancer Syndromes 86 d. 70 heart d. 80 heart d. 56 Ovarian 76 78 70 77 70 Ovarian ca dx 62 58 breast ca dx 48 56 49 75 BRCA 1or 2 Mutations Increase the Risk of Early Onset Breast Cancer By age 40 By age 50 By age 70 Population Risk Hereditary Risk 0.5% 2% 7% 10%20% 33%50% 56%87% BRCA 1 or 2 Mutations Increase the Risk of Ovarian Cancer By age 70 Population Risk 1-2% Hereditary ~ 44% (BRCA1) Risk ~ 27% (BRCA2) Managing Hereditary Cancer Risk Improved outcomes with proven medical interventions* • Surveillance • Chemoprevention • Prophylactic surgery *Individual risk reduction may vary based on personal health history JAMA 2000;283:617-24 Surveillance • Monthly Self-Breast Exams starting @ 18y • Clinical Breast Exam, Semiannually, starting @ 25yrs • Annual Mammogram & Breast MRI (Breast Coil) starting @ 25 yrs • Trans-vaginal US every 6 months • Serum CA-125 every 6 months NCCN Practice Guidelines in Oncology-v.1.2008 HBOC EARLY DETECTION IS THE KEY! Chemoprevention • Tamoxifen effective in prevention of contralateral breast cancer Reducing the risk up to 49% NCCN Practice Guidelines in Oncology-v.1.2008 HBOC Prophylactic Surgery • Bilateral Mastectomy Reducing the risk by 90% • Bilateral Oophorectomy Reducing the risk of Breast Cancer by 68% Reducing the risk of Ovarian Cancer by 96% NCCN Practice Guidelines in Oncology-v.1.2008 HBOC For Men • Risk for Developing Breast Cancer Increases 1% (general Pop) to 7% • Risk for Developing Prostate Cancer Increases 15% (general Pop) to 20% NCCN Practice Guidelines in Oncology-v.1.2008 HBOC / b.2.2007 PCED For Men • Monthly Breast self-exams • Semi-annual Clinical Breast exam • Consider baseline Mammogram • PSA starting @ 40 y/o NCCN Practice Guidelines in Oncology-v.1.2008 HBOC / b.2.2007 PCED PRO Identification of Family Members Not at Risk • Negative for known familial BRCA mutation –Did not inherit cancer risks • General population screening guidelines • Avoid unnecessary screening and possibly surgery PRO Genetic Discrimination Myth versus Reality • Federal and state laws prohibit the use of genetic information as a ‘pre-existing condition’ Federal HIPAA & GINA (Genetic Information Nondiscrimination Act) The majority of states have additional laws including Texas, Arkansas, Louisiana, & Oklahoma No documented cases of genetic discrimination http://www.ncsl.org (National Conference of State Legislature) PRO Insurance Coverage of Genetic Testing • Most insurers provide coverage for genetic testing – On average, a patient will pay $300 or less out-of-pocket • Established guidelines meeting criteria – Medicare pays 100% – Most major carriers – Myriad’s Indigent Program pays 100% CONS & SOLUTIONS • Cost --Genetic Testing – ↑ Screenings → • Assistance Programs – Free or reduced Screenings Surgery • Lack of Genetic Educators & Counselors → • Educate nurses working in High Risk areas to Identify Pts • On line list of available sites • Free Kits • Lack of availability of Testing → • Fear of Discrimination → • Reassurance & providing copies of Federal & State Laws • Education • Feeling of Guilt → Nursing Responsibilities The International Council of Nurses (ICN) Code of ethics for nurses states primary responsibility of nursing is to ensure that a patient receives adequate information on which to base care and treatment decisions. • http://www.icn.ch/abouticn.htm NURSING IMPLICATIONSResearch – Support – Advocate – Participate Education – Plan and push for genetic content integration – Ensure nursing guidelines have incorporated ethical principles regarding genetic information – Develop appropriate clinical application of genetic technology Social – Define and develop policies addressing ethical, legal, and social implications NURSING IMPLICATIONS Ethical, Legal & Social • Privacy and confidentiality of genetic information. • Individuals own and control information, entitled to privacy. • Misuse of genetic information. • Who should have access and how it will be used? • Stigmatization – Use of information to marginalize and discriminate based on persons genes. References • http://www.nursingworld.org/Main MenuCategories/EthicsStandards/Ge netics1.aspx • Essential Competencies • Professional Responsibilities OR • http://www.genome.gov/Glossary The Talking Dictionary developed by The National Human Genome Research Institute (NHGRI) Sporadic or Hereditary ? 75 breast ca dx 49 78 d. 56 Prostate ca d.36 MVA 70 breast ca dx 49 72 75 d. 70 heart 70 Leukemia dx 68 58 Ovarian ca dx 58 56 49 75 Knowledge is Power & Hope