polymorphisms
advertisement

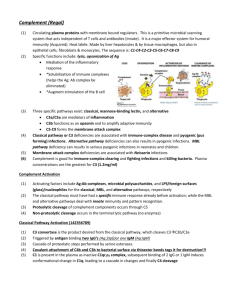
Academic Trainees Meeting – 5th May, 2011 Interesting aspects of complement regulation…… Matthew Pickering Wellcome Trust Senior Fellow in Clinical Science Consultant Rheumatologist Complement activation protein deficiency Classical pathway C3 Terminal pathway Infection Recurrent infection with encapsulated bacteria e.g. pneumococci, Haemophilus influenzae SLE-like illness Vasculitis, glomerulonephritis Recurrent Neisseria infections Complement dysregulation C1 inhibitor deficiency [classical pathway dysregulation] Terminal pathway dysregulation Alternative pathway dysregulation renal thrombotic microangiopathy Atypical haemolytic uraemic syndrome Hereditary angioedema Paroxysmal nocturnal haemoglobinuria Dense deposit disease, Disorders of complement ‘too little’ complement Activation protein deficiency Tell us what might happen if we therapeutically inhibit complement ‘too much’ complement’ Regulatory protein deficiency Provide diseases in which complement inhibiting therapies ought to be effective Complement activation immune complexes classical pathway Bacterial Carbohydrate, ficolins ‘always on’ lectin pathway alternative pathway C3 C5a C4b2a C3bBb C5 activation C3b MAC C3b C3b C3b C3b FOREIGN SURFACE MAC = membrane attack complex ‘C3b amplification loop’ Complement regulation C1 inhibitor C4bp C1 inhibitor classical pathway lectin pathway Factor H alternative pathway C3 Factor H C4b2a C3bBb C3b Factor I iC3b MAC CD59 MAC = membrane attack complex CD46 Factor I C3b CR1 DAF (CD55) Factor H iC3b Complement dysregulation and disease: Physiological control of complement activation REGULATORS ACTIVATORS Loss of function Gain of function The balance is influenced by mutations (extreme) and and/or polymorphisms (‘fine tuning’) What does factor H do? Critical negative regulator of the alternative pathway and C3b amplification loop What happens to C3 levels in individuals with complete genetic deficiency of CFH? Uncontrolled spontaneous activation of the alternative pathway and secondary consumption of C3 Why is factor H important? It is associated with human disease: ‘protective’ and ‘at risk’ polymorphisms common mutations rare Dense deposit disease Dense deposit disease Electron-dense transformation of the glomerular basement membrane Glomerular C3 staining in DDD DDD retinopathy Dense deposit disease Associated with plasma C3 activation: C3 nephritic factor Factor H C3 C3bBb Anti-factor H C3b B, D Dense deposit disease Animal models: Spontaneous porcine factor H deficiency and gene-targeted factor Hdeficient mice Profound plasma C3 depletion – 5% of normal C3 levels Spontaneous renal disease – ‘murine/porcine DDD’ Plasma C3 - mg/l 600 Factor H deficiency Wild-type 400 200 0 C3 staining wild-type Cfh-/- Dense deposit disease What have the animal models taught us? The renal disease does not develop if activation of C3 is blocked The renal disease does develop if C5 activation is blocked Dense deposits still develop Glomerular inflammation reduced but not absent Glomerular basement membrane deposits in mice with combined deficiency of factor H and C5 Pickering MC, et al. PNAS 2006 103(25):9649-54. Murine dense deposit disease is dependent on the ability to activate C3 but not C5 Human complement deficiency Deficiency State: C3 Factor I Factor H Plasma C3: absent low low C3b iC3b, C3d Associations: Recurrent infection immune complex-mediated renal disease e.g. MPGN type I Dense deposit disease Pickering MC, Cook HT. Clin Exp Immunol. 2008 51(2):210-30. Plasma C3 regulation Continuous activation of C3 occurs in plasma through the C3 ‘tick-over’pathway C3c C3d C3 iC3b Factor H C3bBb Factor I C3b C3b Factor B Factor D Dense deposit disease Administration of factor I to mice with combined deficiency of H and I restores GBM C3 staining Plasma C3 levels (mg/l) 200 150 100 50 0 injections 0 24 48 hours Rose KL et al. J Clin Invest. 2008 118(2):608-18. 72 Why is factor H important? It is associated with human disease: ‘protective’ and ‘at risk’ polymorphisms common mutations rare Atypical haemolytic uraemic syndrome Dense deposit disease Atypical Haemolytic uraemic syndrome Alternative pathway dysregulation Associated with: COMPLEMENT MUTATIONS Loss of function mutations in regulators • Factor H • Mutations • Hybrid gene (copy number variation) • Factor I • MCP (CD46) renal thrombotic microangiopathy Atypical haemolytic uraemic syndrome Gain of function mutations in activation proteins • C3 • Factor B ACQUIRED COMPLEMENT DYSREGULATION Anti-factor H autoantibodies Atypical Haemolytic uraemic syndrome – factor H mutations C3 regulation C3 Surface recognition C3bBb MAC C5a B, D C3b C5 activation Factor I C3b C3b C3b C3b C3b HOST SURFACE RENAL ENDOTHELIUM CD46 iC3b Murine model of factor H-associated atypical haemolytic uraemic syndrome Gene-targeted factor H-deficient mice transgenically expressing a mutant mouse factor H protein (FH16-20) wild-type mouse CFH Mutated mouse FH16-20 Plasma C3 - mg/l 100 75 50 25 0 Cfh-/- Cfh-/-FH16-20 Renal histology in Cfh-/-.FH16-20 Murine model of factor H-associated atypical haemolytic uraemic syndrome Use this model to determine contribution of C5 activation to renal injury Spontaneous renal disease does not occur in C5-deficient Cfh-/-FH16-20 animals Murine model of factor H-associated atypical haemolytic uraemic syndrome C3 C9 Cfh-/-FH16-20 animals are hypersensitive to experimentally triggered renal injury – this injurious response is C5 dependent Atypical haemolytic uraemic syndrome - therapy C5 inhibition successful in case reports – examples: Eculizumab for aHUS – N. Engl. J. Med. 2009 360:5 pp542-543 Eculizumab for congenital aHUS – N. Engl. J. Med. 2009 360:5 pp544-6 Open Label Controlled Trial of Eculizumab in Adult Patients With Plasma Therapy-sensitive / -resistant Atypical Hemolytic Uremic Syndrome (aHUS) Successful outcomes announced in ASN 2010 meeting http://clinicaltrials.gov/ct2/results?term=eculizumab Why is factor H important? It is associated with human disease: ‘protective’ and ‘at risk’ polymorphisms common mutations rare Atypical haemolytic uraemic syndrome Dense deposit disease Factor H and Age-related macular degeneration Factor H and AMD – the ‘Y402H’ polymorphism From Sofat et al., Atherosclerosis 213 (2010) 184-90 Factor H and Age-related macular degeneration Alternative pathway dysregulation Associated with: Polymorphic variants in: Regulators • Factor H Y402H ‘at risk’ V62I ‘protective’ activation proteins • C3 C3FF ‘at risk’ Ocular drusen Age-related macular degeneration • Factor B Bf32Q ‘protective’ Factor H and Age-related macular degeneration 62Valine 62Isoleucine Age-related macular degeneration Functional differences in the Valine62Isoleucine CFH polymorphism 62Isoleucine more efficient at preventing red cell lysis 14nM vs. 22.6nM at 50% lysis Complement dysregulation and eye disease – age-related macular degeneration Factor H 402Y* Factor H 62I Factor B 32Q C3S CFHR1/3 deletion* Factor H 402H* Factor H 62V Factor B 32R C3F ‘protective’ polymorphisms ‘at risk’ polymorphisms Factor H null alleles C3 3923∆DG mutations alternative pathway activation Ocular drusen Age-related macular degeneration *functional consequences not understood DDD retinopathy Dense deposit disease Why is factor H important? It is associated with human disease: ‘protective’ and ‘at risk’ polymorphisms common Age-related macular degeneration Meningococcal sepsis mutations rare Atypical haemolytic uraemic syndrome Dense deposit disease Factor H and susceptibility to meningococcal infection Meningococcal sepsis The factor H family Why are the factor H-related proteins important? They are associated with human disease: ‘protective’ and ‘at risk’ polymorphisms common mutations rare The factor H family: copy number variation Most frequent CFH-CFHR allele CFH CFHR3 CFHR1 CFHR4 CFHR2 CFHR5 CFHR2 CFHR5 CFHR1-3 deletion allele polymorphism (common) CFH CFHR4 Deletion homozygotes: African American European Americans Hageman et al, Ann. Medicine 2006 16% 4.7% Others (uncommon - <1%) CFH CFHR1 CFH CFHR3 CFH CFHR3 CFH CFHR3 CFHR1 CFH CFHR3 CFHR1 CFHR4 CFHR2 CFHR5 CFHR4 CFHR2 CFHR5 CFHR2 CFHR5 CFHR3 CFHR1 CFHR4 CFHR2 CFHR5 CFHR1 CFHR4 CFHR2 CFHR5 Why are the factor H-related proteins important? They are associated with human disease: ‘protective’ and ‘at risk’ polymorphisms CFHR1-3 deletion allele polymorphism associated with protection against AMD common Age-related macular degeneration Mol Immunology 44 (2007):3921. Complement therapeutics Pathologies in which complement is activated Complement therapeutics Examples of the many complement inhibitors in development Eric Wagner and Michael Frank Nature Reviews 2010, vol. 9, 43-56. Thanks Elena Goicoechea de Jorge Katherine Vernon Mitali Patel Kirsten Rose Talat Malik Sharmal Narayan Marieta Ruseva Tamara Montes Lola Sanchez-Nino Danielle Paixao-Cavalcante Fadi Fakhouri Terence Cook Marina Botto Santiago Rodriguez de Cordoba Veronique Fremeaux -Bacchi Patrick Maxwell Danny Gale