Faith Davies - UK Myeloma Forum
advertisement

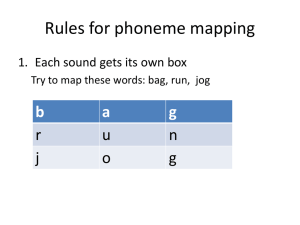
in partnership with The Role of Cytogenetics in Elderly patients with Myeloma Dr Faith Davies Cancer Research UK Senior Cancer Fellow Centre for Myeloma Research Divisions of Molecular Pathology, Cancer Therapeutics and Clinical Studies Royal Marsden Hospital and The Institute of Cancer Research London Making the discoveries that defeat cancer Stages of Disease clinically and biologically Morgan, Walker & Davies Nat Rev Cancer 2012 12:335 Advances in technology have led to an increasing knowledge of myeloma genetics Translocations of C14 G band FISH 1995 Conventional Cytogenetics G-banding Wikipedia et al !! Chromosome 14 FISH - translocation Immunoglobulin heavy chain locus Dual, Break Apart probe Centromere J segs D segs 14q32 region Constant seg Telomere Variable segments c. 250 kb c. 900 kb IGH 3’ Flanking Probe IGHV Probe Kindly provided by Dr Fiona Ross, Wessex Regional Cytogenetics Laboratory Molecular classification of myeloma Early events • Translocations – – – – – t(4;14) t(11;14) t(6;14) t(14;16) t(16;20) Translocations Hyperdiploidy • Chromosome gain – 3, 5, 7, 9, 11, 15, 19, 21 Kuehl & Bergsagel 2005 Normal Isotype Switching on Chromosome 14q32 telomer e VDJ centromere switch region = 1-3kb long, tandem pentameric repeats) VDJ S VDJ C 2 S2 C2 C2 - Intervening DNA deleted - Hybrid switch formed S S2 2 Illegitimate switch recombination in Myeloma VDJ VDJ Gene X VDJ Gene X 2 C2 Gene Y Gene Y C2 2 Translocations into 14q32 • Various partner chromosomes are linked to 14q32, in cell line studies. Some have also been identified in patients. • Up to 70% of patients have a translocation - thought to be a primary event. • • • • t(11;14)(q13;q32) t(4;14)(p16:q32) t(6;14)(p25;q32) t(14;16)(q32;q23) 30% 15% 4% 5% cyclin D1 FGFR3 and MMSET cyclin D3 and IRF4 cMAF (and WWOX) • many other regions may be involved • often the partner is not identified. Advances in technology have led to an increasing knowledge of myeloma genetics Translocations of C14 Global mapping Gene expression arrays G band TC classification FISH Normal MGU S MM methylation miRNA NGS Translocations t(4;14) t(11;14) t(6;14) t(14;16) t(14;20) Translocations Hyperdiploid Chromosome gain 3, 5, 7, 9, 11, 15, 19, 21 1995 2000 2005 2010 2015 11 Hyperdiploidy • Gain of chromosomes (between 48-74) • Mostly odd numbered chromosomes • 3, 5, 7, 9, 11, 15, 19, 21 1 2 4 3 5 • gain of chromosomes 15, 9 and 19 are most frequent • mechanism of gain not understood 6 7 8 13 14 15 19 20 9 10 11 12 16 17 18 21 22 X Walker et al. Blood 2006 Myeloma specific copy number variation Deletion Gain -Deletion 1p (30%) CDKN2C, FAF1, FAM46C - Deletion 6q (33%) Gain 12p LTBR -Deletion 8p (25%) Gain 17p TACI - Deletion 13 (45%) Gain 17q NIK RB1, DIS3 - Deletion 11q (7%) BIRC2/BIRC3 - Deletion 14q (38%) TRAF3 - Deletion 16q (35%) WWOX, CYLD - Deletion 17p (8%) TP53 - Deletion 20 (12%) - Deletion 22 (18%) - Deletion X (28%) 1 2 Gain 1q 3 4 5 6 7 8 9 (40%) 10 11 CKS1B, ANP32E 12 13 14 15 16 17 18 19 202122 X Boyd KD, et al. Leukemia. 2012;26:349-355. Walker BA, et al. Blood. 2010;116:e56-e65. Myeloma Abnormalities • Number of common abnormalities – Deletions • 13q (45%) and 17p (8%) • Other regions – 1p, 1q (40%), 16q – Translocations – Hyperdiploidy • odd number chromosomes (3,7,9,11,17) The Incidence of Abnormality Changes With Disease Progression Abnormality MGUS (%) SMM (%) MM (%) t(11;14) 10 16 14 t(14;16) 3 3 3 t(14;20) 5 <1 1.5 del(13q) 24 37 45 del(17p) 3 1 8 1q+ 22 39 41 del(CDKN2C) 4 10 15 14 Ross et al. Haematologica 2010 95:1221 Leone et al. Clinical Cancer Research 2008 14:6033 Lopez-Corral et al. Clinical Cancer Research 2011 17:1692 Myeloma Disease Progression and Genetic Events 15 Morgan, Walker & Davies Nat Rev Cancer 2012 12:335 Inter relationship of abnormalities t(4;14) t(11;14) 6 16 20? No Data HRD 16 HRD+t(#;14) None All t(4;14) have del(13) 17p evenly distributed Boyd KD, et al. Leukemia. 2012;26:349-355. Walker BA, et al. Blood. 2010;116:e56-e65. Inter relationship of abnormalities t(4;14) t(11;14) 6 16 20? No Data HRD 17 HRD+t(#;14) None All t(4;14) have del(13) 17p evenly distributed Boyd KD, et al. Leukemia. 2012;26:349-355. Walker BA, et al. Blood. 2010;116:e56-e65. 18 Myeloma IX trial: del(13) by FISH not associated with poor survival outcome* Survival according to del(13) with “bad” IgH and del(17)(p53) removed Survival according to del(13) by FISH 100 100 No del(13) del(13) 80 n = 568 ms 48.3 months 60 40 n = 478 ms 40.9 months 20 Patients (%) Patients (%) 80 No del(13) del(13) only Bad IgH or del(17p) 60 n = 283; ms not reached 40 n = 568 ms 48.3 months 20 p = 0.024 n = 191 ms 27.7 months p < 0.001 0 0 0 10 20 30 40 50 Survival (months) 60 70 0 10 20 30 40 50 60 70 Survival (months) * In the absence of other adverse prognostic features. Inter-relationship of Adverse Lesions 19 Genetic abnormalities are not solitary events and can occur together Strong positive association with adverse IGH and 1q+ -72% of IGH translocations with 1q+ Implications i. In order to understand the prognosis of any lesion need to know if other lesions are present. ii. Lesions may collaborate to mediate prognosis. Boyd et al. Leukemia 2011 Frequency in the Elderly Frequency of abnormalities with age N = 228 Ross et al Leukemia 2006 Frequency of abnormalities with age N = 1890, median age 72, range 66-94 Avet Loiseau et al 2013 JCO Clinical and prognostic significance in the Elderly Myeloma IX trial: effect of “bad” IgH translocations on survival Combined “bad” IgH translocations No “bad” IgH translocations Any “bad” IgH translocation 80 n = 858 ms 49.6 months 60 40 20 0 n = 170 ms 25.8 months p < 0.001 0 10 20 30 40 50 Survival (months) 60 70 Intensive arm 100 Patients (%) “Bad” IgH Rest n = 495 ms not reached 80 60 40 n = 170 ms 36 months 20 0 10 80 60 0 20 ms = median survival. 30 40 50 Survival (months) 60 n = 363 ms 33.4 months 40 20 p < 0.001 0 Non-intensive arm 100 Patients (%) Patients (%) 100 70 n = 63 ms 13.1 months p < 0.001 0 10 20 30 40 Survival (months) 50 60 Myeloma IX trial: effect of deletion 17p53 on survival Survival of patients with del(17)(p53) No del(17)(p53) del(17)(p53) 80 n = 929 ms 45.8 months 60 40 20 0 n = 87 ms 22.2 months p < 0.001 0 10 20 30 40 50 Survival (months) 60 70 del(17)(p53): intensive arm 100 Patients (%) del(17p) Rest 80 n = 545 ms not reached 60 40 20 0 n = 48 ms 40.9 months p = 0.004 0 10 20 30 40 50 Survival (months) del(17)(p53): non-intensive arm 100 60 70 Patients (%) Patients (%) 100 80 60 n = 384 ms 32.6 months 40 20 0 n = 39 ms 19.2 months p = 0.017 0 10 20 30 40 Survival (months) 50 60 Prognostic Impact of Lesions 26 N = 1890, median age 72, range 66-94 Avet Loiseau et al JCO 2013 Myeloma IX trial: effect of combined deletion 17p53 and “bad” IgH on survival Any bad IgH translocation + del(17)(p53) 100 p < 0.001 Patients (%) 80 60 n = 754 40 n = 214 20 n = 18 Bad IgH translocation 0 Bad IgH translocation + del(17p) 0 500 1,000 Survival (days) 1,500 2,000 Rest 28 Impact of Combined Lesions The number of adverse markers has an additive effect on overall survival 60 months 40 months 23.4 months 9.1 months Boyd et al. Leukemia 2011 Defining high risk according to the ISS: “bad” IgH and del(17p) Myeloma IX trial: effect of adverse prognostic features on survival 1 2 3 4 100 ISS + any bad IgH translocation + del(17)(p53) 1 = 1 excluding bad IgH or del(17)(p53) 2 = ditto + 1 including, etc. p < 0.001 Group 1 ISS1 Group 2 ISS2 Group 3 ISS3 Group 4 Patients (%) 80 n = 125 60 n = 244 40 n = 269 bad IgH or del(17p) 20 n = 76 bad IgH or del(17p) 0 0 500 1,000 1,500 2,000 Survival (days) ie having something bad doesn’t always mean it is! Boyd et al. Leukemia 2011 Non-intensive pathway – chemotherapy regimens 500 mg po Days 1, 8, 15, 22 Thalidomide 50 - 200 mg po Daily Dexamethasone a ttenuated 20 mg po Days 1- 4, 15- 18 Maximal response Every 28 Days to maximal response. 6 - 9 cycles Melphalan 7 mg/m2 od po Days 1 - 4 Prednisolone 40 mg od po Days 1 - 4 Every 28 Days to maximal response. 6 - 9 cycles THALIDOMIDE RANDOMISATION CHEMOTHERAPY RANDOMISATION C yclophosphamide Primary endpoints: PFS and OS Secondary endpoints: Response, QoL and toxicity Baseline assessment Response assessment Morgan et al Blood 2011 Summary of patient characteristics at trial entry MP (N=423) CTDa (N=426) Age (years) Median Range 73 57–89 73 58–87 Gender (N (%)) Male Female 231 (54.6) 192 (45.4) 242 (56.8) 184 (43.2) ISS (N (%)) I II III Missing Data 64 (15.1) 156 (36.9) 165 (39.0) 38 (9.0) 46 (10.8) 156 (36.6) 168 (39.4) 56 (13.1) β2M (mg/l) Median Range 4.9 0.3-40.4 5.0 0.4–64.0 Summary of cytogenetics at trial entry Translocation Favourable Adverse MP % CTDa % Total % 125 58.1 129 57.3 254 57.7 90 41.9 96 42.7 186 42.3 Adverse group includes t(4;14), t(14;20) t(14,16), gain 1q and del 17p Morgan et al Blood 2011 PFS and OS according to cytogenetics Favourable Adverse PFS OS 14 months 37 months 95% CI 12-17 range 0-65 95% CI 22-44 range 0-69 12 months 24 months 95% CI 10-13 range 0-67 95% CI 20-28 range 0-68 Morgan et al Blood 2011 OS according to treatment group in patients with favorable cytogenetics P=0.1041 CTDa MP Morgan et al Blood 2011 OS in favorable cytogenetics according to treatment; landmark at 1.5 years CTDa median not reached MP 42 months CTDa not reached vs 42 months Morgan et al Blood 2011 Influence of cytogenetics on survival among patients achieving a CR Favourable Adverse Morgan et al Blood 2011 NGS results inform myeloma biology • No single mutation responsible for myeloma – hundreds of mutations identified. • Deregulation of pathways is an important molecular mechanism. • Including NF-κB pathway, histone modifying enzymes and RNA processing. Morgan GJ, Walker BA and Davies FE. Nature Reviews Cancer. Vol 12 May 335-348, 2012, Mutational landscape of myeloma • Acute leukaemia – 8 non-synonymous variants per sample Hallmarks Of Myeloma • Myeloma – 35 non-synonymous variants per sample • Solid tumours – 540 non-synonymous variants per sample Morgan G, et al. Nat Rev Cancer. 2012;12:335-48. Comparative analysis of cancer evolutionary trees Comparison across disease states and curability Paediatric ALL Myeloma Solid cancer Linear and branching models for myeloma evolution 40 Morgan, Walker and Davies Nature Reviews Cancer 2012 Linear and branching models for myeloma evolution 41 Morgan, Walker and Davies Nature Reviews Cancer 2012 “Nothing in biology makes sense except in the light of evolution” Theodosius Dobzhansky, 1973 “Nothing in biology makes sense except in the light of evolution” Theodosius Dobzhansky, 1973 Adaption and survival of the fittest Charles Darwin “Applying the ideas developed initially by Darwin, to explain the origin of the species, can inform us of how cancer develops and how best to treat it” Clonal evolution of myeloma Selective pressures Ecosystem 1 Ecosystem 2 Treatment Ecosystem 3 Ecosystem 5 EMM Diffuse Single founder cell (stem or progenitor) MGUS Ecosystem 4 Focal MM PCL Adaption and survival of the fittest Subclones with unique genotype/”driver” mutations Adapted from Greaves MF, Malley CC. Nature. 2012;481:306-13. A Model of MM Disease Progression A model based on the random acquisition of genetic hits and Darwinian selection Initiation Germinal centre Post-GC B cell Progression Bone marrow MGUS Peripheral blood Smouldering myeloma Myeloma Plasma cell leukaemia Inherited variants Primary genetic events IgH translocations Hyperdiploidy Secondary genetic events Copy number abnormalities DNA hypomethylation Acquired mutations COMPETITION AND SELECTIVE PRESSURE MIGRATION AND FOUNDER EFFECT Clonal advantage Myeloma progenitor cell TUMOUR CELL DIVERSITY GENETIC LESIONS Morgan G, et al. Nat Rev Cancer. 2012;12:335-48. A Darwinian View of Induction, maintenance and relapse Clones can be eradicated - cured Morgan GJ, Walker BA, Davies F. Nature Reviews Cancer, 2012 A Darwinian view of induction, maintenance and relapse Clones can be eradicated - cured Post treatment Myeloma progenitor cell Evolutionary / Treatment Bottleneck Morgan GJ, Walker BA, Davies F. Nature Reviews Cancer, 2012 Intraclonal heterogeneity and targeted treatment Clones with a distinct pattern of mutations Target Intraclonal heterogeneity and targeted treatment Clones with a distinct pattern of mutations Suboptimal response at 30% A Darwinian View of Induction, maintenance and relapse Clones can be eradicated - cured Morgan GJ, Walker BA, Davies F. Nature Reviews Cancer, 2012 A Darwinian view of induction, maintenance and relapse Clones can be eradicated - cured Post treatment Myeloma progenitor cell Evolutionary / Treatment Bottleneck Morgan GJ, Walker BA, Davies F. Nature Reviews Cancer, 2012 Clonal Tides During Myeloma Treatment Relapse can come from any one of a number of clones Relapse Original clone – treatment resistant Myeloma progenitor cell Differential sensitivity to treatment treatment sensitive Morgan GJ, Walker BA, Davies F. Nature Reviews Cancer, 2012 Clonal dynamics over multiple relapses Clinical evidence supports this - a t(4;14) case Keats JJ, et al. Blood. 2012;120:1067-76. Conclusions • Myeloma is biologically and genetically diverse. • Genetic complexity develops early before clinical symptoms develop. • Linking biological data to clinical data is beginning to identify clinically distinct subgroups with different disease characteristics and outcomes. • The frequency of the different subgroups differs with age, but the prognostic significance remains • Darwinian style processes can describe the multistep pathogenesis of myeloma. • The impact of clonal heterogeneity needs to be considered when making treatment choices Conclusion • Knowledge of the patients genetic sub group is important regardless of the patients age • This has been incorporated into the UKMF/BCSH guidelines • C14 translocation, 17p, HRD, C1 in partnership with Centre for Myeloma Research, ICR Davies Lab Mike Bright Chief Investigators Lei Zhang JA Child Lauren Aronson GJ Morgan Jade Strover GH Jackson Jackie Fok Daniel Izthak NH Russell Morgan Lab Brian Walker Chris Wardell David Johnson Li Ni David Gonzalez Ping Wu Fabio Mirabella Lorenzo Melchor AnnaMaria Brioli Charlotte Pawlyn Elileen Boyle Matthew Jenner Kevin Boyd Martin Kaiser CTRU, Leeds K Cocks W Gregory A Szubert S Bell N Navarro Coy F Heatley P Best J Carder M Matouk D Emsell A Davies D Phillips Leeds RG Owen AC Rawstron R de Tute M Dewar S Denman G Cook S Feyler MRC Leukaemia Trial Steering Committee MRC Leukaemia Data Monitoring and Ethics Committee NCRI Haematological Oncology Clinical Studies Group UK Myeloma Forum Clinical Trials Committee Myeloma UK D Bowen Birmingham MT Drayson K Walker A Adkins N Newnham Salisbury F Ross L Chieccio Funding Medical Research Council Pharmion Novartis Chugai Pharma Bayer Schering Pharma OrthoBiotech Celgene Kay Kendall Leukaemia Fund