File - SPHS Devil Physics
advertisement

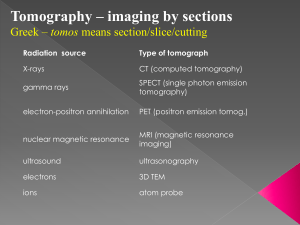
DEVIL PHYSICS THE BADDEST CLASS ON CAMPUS IB PHYSICS TSOKOS OPTION I-2 MEDICAL IMAGING Reading Activity Answers IB Assessment Statements Option I-2, Medical Imaging: X-Rays I.2.1. Define the terms attenuation coefficient and half-value thickness. I.2.2. Derive the relation between attenuation coefficient and half-value thickness. I.2.3. Solve problems using the equation, I I 0e x IB Assessment Statements Option I-2, Medical Imaging: X-Rays I.2.4. Describe X-ray detection, recording and display techniques. I.2.5. Explain standard X-ray imaging techniques used in medicine. I.2.6. Outline the principles of computed tomography (CT). IB Assessment Statements Option I-2, Medical Imaging: Ultrasound I.2.7. Describe the principles of the generation and the detection of ultrasound using piezoelectric crystals. I.2.8. Define acoustic impedance as the product of the density of a substance and the speed of sound in that substance. I.2.9. Solve problems involving acoustic impedance. IB Assessment Statements Option I-2, Medical Imaging: Ultrasound I.2.10. Outline the difference between A-scans and B-scans. I.2.11. Identify factors that affect the choice of diagnostic frequency. IB Assessment Statements Option I-2, Medical Imaging: NMR and Lasers I.2.12. Outline the basic principles of nuclear magnetic resonance (NMR) imaging. I.2.13. Describe examples of the use of lasers in clinical diagnosis and therapy. Objectives State the properties of ionizing radiation State the meanings of the terms quality of Xrays, half-value thickness (HVT), and linear attenuation coefficient Perform calculations with X-ray intensity and HVT, I I 0e x HVT 0.693 Objectives Describe the main mechanisms by which X rays lose energy in a medium State the meaning of fluoroscopy and moving film techniques Describe the basics of CT and PET scans Describe the principle of MRI State the uses of ultrasound in imaging State the main uses of radioactive sources in diagnostic medicine Properties of Radiation Two uses in medicine: Diagnostic imaging (this lesson) Radiation therapy (next lesson) Properties of Radiation Types of Radiation: Alpha (α) Beta (β) Gamma (γ) Properties of Radiation Intensity – power as if it were radiated through a sphere P I 2 4r Attenuation Intensity drops exponentially when passed through a medium capable of absorbing it The degree to which radiation can penetrate matter is the quality of the radiation I I 0e x μ is a constant called the linear attenutation coefficient Attenuation Attenuation depends not only on the material the radiation passes through, but also on the energy of the photons Attenuation Half-Value Thickness (HVT) – similar to radioactive decay law, the length that must be travelled through in order to reduce the intensity by a factor of 2 HVT 0.693 Attenuation Half-Value Thickness as a function of photon energy Attenuation X-rays absorbed via photoelectric and Compton effects Photoelectric effect – X-ray photons absorbed by an electron which is then emitted by the atom or molecule Compton effect – photon gives part of its energy to a free electron and scatters off it with a reduced energy and increased wavelength (elastic collision) X-ray Imaging First radiation to be used for imaging Operate at voltage of around 15-30 kV for mammogram 50-150 kV for chest X-ray X-ray Imaging X-ray Imaging Most energy lost through photoelectric effect Photoelectric effect increases with atomic number of elements in tissue Bone will absorb more X-rays than soft tissue X-rays show a contrast between bone and soft tissue Energy will pass through soft tissue and expose the film on the other side Energy absorbed by bone tissue will cast a shadow X-ray Imaging When there is no substantial difference between Z-numbers in the material, patients are give a contrast medium, usually barium Barium absorbs more X-rays to give a sharper image X-ray Imaging Image is sharper if: Film is very close to patient X-ray source is far from patient Lead strips are moved back and forth between patient and film to absorb scattered X-rays Low-energy X-rays removed by filtering Intensifying screens used to enhance energy of photons passed through patient to reduce exposure time X-ray Imaging X-ray Imaging X-rays on TV Capability to project real-time X-ray images on a monitor Advantages outweighed by increased exposure time/radiation dosage Does have advantages for examining cadavers and inanimate objects (jet engines) Computed Tomography (CT Scan) Computed (axial) tomography or Computer assisted tomography (CAT) Still uses X-rays, but Reduced exposure time Greater sharpness More accurate diagnoses Computed Tomography (CT Scan) Thin X-ray beam directed perpendicular to the body axis Beam creates an image slice that can be viewed from above • Source then rotates to take a slice from a different angle Computed Tomography (CT Scan) Many detectors are used to record the intensity of X-rays reaching them Information is sent to a computer to reconstruct the image Similar to digital camera processing • Detector grids are also called pixels Magnetic Resonance Imaging (MRI) Based on a phenomenon called nuclear magnetic resonance Superior to CT Scan No radiation involved (don’t let ‘nuclear’ throw you) But, much more expensive Magnetic Resonance Imaging (MRI) Electrons, protons and most particles have a property called spin – See Eric Particles with an electrical charge and spin behave like magnets – magnetic moment In the presence of a magnetic field, the moment Will align itself parallel (‘spin up’) Or anti-parallel (‘spin down’) to the direction of the field Magnetic Resonance Imaging (MRI) Hydrogen protons have specific energy levels In the presence of a magnetic field, the energy level will change based on how the magnetic moment aligns with the field Difference in energy levels is proportional to the external magnetic field strength Magnetic Resonance Imaging (MRI) A radio frequency (RF) source (electromagnetic radiation) is introduced If the frequency of the RF source corresponds to the difference in energy levels, the proton will jump to the higher state, then go back down and emit a photon of the same frequency Magnetic Resonance Imaging (MRI) Detectors register the photon emissions and a computer can reconstruct an image based on the point of emission Rate of photon emission important to identifying tissue type Magnetic Resonance Imaging (MRI) Point of emission determined by using a second magnetic field to break up uniformity of original magnets used to align the spins External magnetic field regulates photon emissions Magnetic Resonance Imaging (MRI) Process dependent on hydrogen saturation Newer techniques can measure rate at which protons return to ground state to better identify tissue type Magnetic Resonance Imaging (MRI) Show and Tell Positron Emission Tomography (PET Scan) Similar to a CT Scan Involves annihilation of an electron and a positron (anti-particle of the electron) and detection of two photons that are then produced Positron Emission Tomography (PET Scan) Patients injected with radioactive substance that emits positrons during decay Emitted positron collides with an electron in the patient’s tissue Electron-positron collision annihilates in two photons each of energy 0.511 MeV e e 2 Positron Emission Tomography (PET Scan) Total momentum is conserved an the photons move in opposite directions with same velocity Detectors can then located the point of emission Can give a resolution of 1mm Especially good for brain images Ultrasound Uses sound in the 1 to 10 MHz range – not audible No radiation No known adverse side effects Can produce some images X-rays can’t (lungs) Not as detailed as X-rays Ultrasound Sound emitted in short pulses and reflection off various surfaces is measured Very similar to sonar and radar Diffraction limits resolution size, d, to λ < d Wavelength determined by speed of sound in tissue In practice, with the frequencies used, pulse duration and not diffraction limits resolution Ultrasound Frequency determined by the type of organ tissue studied Rule of thumb is f = 200(c/d) where c is speed of sound and d is depth (depth of 200 wavelengths Ultrasound Transition into a body an into different tissues means some of the waves will be reflected Amount transmitted into second tissue depends on impedance of the two media Z v It 4 Z1 Z 2 2 I 0 Z 1 Z 2 I r Z 1 Z 2 2 I 0 Z 1 Z 2 2 Ultrasound For the most energy to be transmitted, impedances should be as close as possible Gel is used between transducer and body to improve impedance matching Ultrasound A-Scan Ultrasound A-Scan Ultrasound Combined A-Scans Diagnostic Uses of Radioactive Sources Used to monitor organs and their functions Measurement of body fluids How food is digested Vitamin absorption Synthesis of amino acids How ions penetrate cell walls Radioactive iodine used to monitor thyroid functions Diagnostic Uses of Radioactive Sources Most commonly used is technetium-99 Horse example (27 minutes) Abridged version Summary of Imaging Methods Σary Review State the properties of ionizing radiation State the meanings of the terms quality of Xrays, half-value thickness (HVT), and linear attenuation coefficient Perform calculations with X-ray intensity and HVT, I I 0e x HVT 0.693 Σary Review Describe the main mechanisms by which X rays lose energy in a medium State the meaning of fluoroscopy and moving film techniques Describe the basics of CT and PET scans Describe the principle of MRI State the uses of ultrasound in imaging State the main uses of radioactive sources in diagnostic medicine IB Assessment Statements Option I-2, Medical Imaging: X-Rays I.2.1. Define the terms attenuation coefficient and half-value thickness. I.2.2. Derive the relation between attenuation coefficient and half-value thickness. I.2.3. Solve problems using the equation, I I 0e x IB Assessment Statements Option I-2, Medical Imaging: X-Rays I.2.4. Describe X-ray detection, recording and display techniques. I.2.5. Explain standard X-ray imaging techniques used in medicine. I.2.6. Outline the principles of computed tomography (CT). IB Assessment Statements Option I-2, Medical Imaging: Ultrasound I.2.7. Describe the principles of the generation and the detection of ultrasound using piezoelectric crystals. I.2.8. Define acoustic impedance as the product of the density of a substance and the speed of sound in that substance. I.2.9. Solve problems involving acoustic impedance. IB Assessment Statements Option I-2, Medical Imaging: Ultrasound I.2.10. Outline the difference between A-scans and B-scans. I.2.11. Identify factors that affect the choice of diagnostic frequency. IB Assessment Statements Option I-2, Medical Imaging: NMR and Lasers I.2.12. Outline the basic principles of nuclear magnetic resonance (NMR) imaging. I.2.13. Describe examples of the use of lasers in clinical diagnosis and therapy. QUESTIONS? Homework #1-8