Restrictive Lung Disease
advertisement

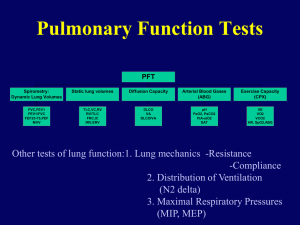
Restrictive and Interstitial Lung Disease J.B. Handler, M.D. Physician Assistant Program University of New England 1 Abbreviations SLE- systemic lupus erythematosis DLCO- diffusing capacity for carbon monoxide HRCT- high resolution computed tomography ALS- Amyotrophic Lateral Sclerosis RR- respiratory rate IFIP- idiopathic fibrosing interstitial pneumonia RA- rheumatoid arthritis 2 Restrictive Disease and Dysfunction Collection of diseases that are characterized by reduction in volume of air within the lung parenchyma. Abnormal reduction in pulmonary ventilation. Restrictive pattern on PFT’s. Compensated by RR. Multiple etiologies: Most common are forms of interstitial lung disease. Some diseases have both obstructive and restrictive components: Cystic fibrosis, others. 3 Interstitial Lung Disease Heterogeneous group of diseases (>180) with common response to lung injury. Idiopathic fibrosing interstitial pneumonia (IFIP), formerly called Idiopathic (primary) Pulmonary Fibrosis: Classic example of restrictive lung disease. Multiple secondary etiologies- see below. Pathology is similar, regardless of etiology. 4 Secondary Etiologies Drug related: Amiodarone (potent antiarrhythmic), bleomycin (tx cancer), some antibiotics (sulfonamides), others. Occupational inhalation: Silica, asbestos, beryllium, others. Connective tissue disorders: SLE, Polymyositis, RA, scleroderma. Others: Radiation, amyloidosis, sarcoidosis. Infections: Fungal (Coccoidiomycosis, Pneumocystis), Mycobacterium, some 5 viruses. IFIP Diagnosis of exclusion Must exclude other etiologies (via biopsy) before saying “idiopathic”. Variations of IFIP exist, with varying response to therapy. Characteristic clinical, radiographic, PFT and other findings. Poor prognosis as with many other etiologies of interstitial lung disease. 6 Pathology Inflammatory infiltrate in lung parenchyma/interstitium: Inflammation of alveolar epithelium and capillary endothelium followed by: Fibrosis of the alveoli and interalveolar septum Inflammation can include the respiratory bronchioles. Thickening of alveolar-capillary membrane by collagen and fibrous tissue. Over timeFibrosis throughout lung parenchyma. 7 Terminal Respiratory Unit Images.google.com Pathology/Pathophysiology Inflammatory cellular and fibrotic response. Inflammatory cells release chemical mediators activation of fibroblasts collagen deposition. Tissue injury, vascular injury and permeability. Epithelial injury thickens/breaks alveolarcapillary membraneimpaired diffusion of gas (DLCO). 9 Pathophysiology Destruction of alveoli/capillariesV/Q mismatch; both shunting and increased dead space. Ongoing repair/re-injury cycle; nonhomogeneous scarring throughout lung. Lung compliance. 10 Normal Lung Parenchyma Images.google.com Pulmonary Fibrosis Images.google.com Clinical Presentation (IFIP) Insidious onset most often with gradual development of shortness of breath; initially exertional, then at rest. Other etiologies may have acutechronic presentation. History: Occupational exposure? Smoker? Travel history (parasitic infections) Risk factors for HIV 13 Clinical Presentation Decreased activity tolerance Dry, non-productive cough +/- fever; depends on etiology Presentation may vary depending on etiology 14 Physical Exam, Testing Lungs: Fine, inspiratory crackles (like velcro) at lung bases. RR late. Clubbing of fingers: bony growth and enlargement of terminal phalange; present 25-50% of cases. Chest x-ray (see below): May appear normal until advanced disease. HRCT- may be useful- confirms “honeycomb pattern”. 15 Clubbing of Fingers Images.google.com Chest X-Ray Lung volume Interstitial “honeycombing” Indicates advanced Disease Images.google.com PFT’s and ABG Marked reduction in all lung volumes. FVC, FEV1, both often markedly Normal FEV1/FVC (or ) DLCO ABG: progressive hypoxemia due to both DLCO and V/Q mismatch. Worse with exercise. PCO2 reflects increased respiratory rate to accommodate hypoxemia. PCO2 levels rare except with end stage disease. 18 Lung Biopsy Most important tool to confirm diagnosis and sort out underlying etiologies. Trans bronchial biopsy- least invasive, but sample size to small in most cases. Thoracoscopic biopsy- less invasive than open thoracotomy but still requires small incisions into thorax. Open lung biopsy- requires thoracotomy; multiple samples obtained from different areas of lung. 19 Treatment No data to show that any treatment improves survival or quality of life of in patients with IFIP. Progressive disease in most patientsdeath in 3-5 years. Other etiologies sometimes respond to systemic corticosteroids (prednisone, et al) or immunosuppressive agents with varying degrees of improvement. 20 Restrictive Disease: Others Neuromuscular diseases: ALS, Muscular Dystrophy, Polio,etc. Impair lung inflation; restrictive pattern on PFT’s. Kyphoscoliosis: Decrease lung volume; restrictive pattern on PFT’s. – abnl forward bending puts pressure on lungs Pleural diseases: prevent lung expansion; restrictive pattern on PFT’s. 21 Scoliosis Images.google.com