Detecting Cancer earlier in Tower
Hamlets – The New Network Service
The Tools we’ll need
Dr. Tania Anastasiadis
Tower Hamlets GP Cancer Lead
& GP Macmillan facilitator
Sunday times 11th May 2014
Our stats….
• TH mortality rates are amongst the highest in
the country and our survival rates amongst
the lowest
• Of 550 TH residents diagnosed with Cancer
<64% (350) were alive at 12 months post
diagnosis (Office of National Statistics 2010)
A postcode lottery…?
• The Sunday Times article relates to those
diagnosed at Stage 1+2 (35.7%)
• Half of London boroughs weren’t reported
as there was not enough available data…
• We know residents in TH have more health
inequalities & higher than average
deprivation
Our role…
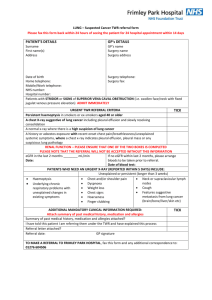
• Public Health are funding the new NIS (£130,000)
• The outcome measures are based on current available evidence &
research to date
Early detection in primary care relies on:
•
•
•
•
Patients being aware of symptoms that could mean cancer
Patients deciding to present
GPs recognising symptoms
Rapid referral of symptomatic patients for investigation and
treatment
Training &
updating
Reviewing and
improving
systems in
primary care
Use of cancer
decision support
tools
Community
training and
engagement
Auditing
cancers
Lung cancer –
targeting high risk
groups
Increasing
uptake of bowel
screening
Training and updating teams in early
diagnosis of cancer
• Clinical & public facing non clinical
eg PLTs, Talk Cancer, e-learning modules
http://cancerawarenesstoolkit.com/
Community organisation engagement
• Increasing public awareness
Reviewing and improving systems in
primary care
• SEA/peer discussion relating to
newly diagnosed cancers
• Strengthened safety netting eg
‘small-c’ resource packs
• Meeting with CCG Cancer Lead
(practice profiles, bowel screening
metrics, cancer audits, identify
barriers to earlier diagnosis)
http://www.smallc.org.uk/health-professionals/resource-packs/
Auditing cancers
• National audit of cancer diagnoses in primary care
(2009/2010 NAEDI, RCGP)
• Same audit tool
• Better understand and address the reasons for later diagnosis
of cancer
• Identify local areas for improvement
• £70 per audit
• Feature of future appraisals…
Use of Clinical decision support
tools (CDST)
• 90% patients diagnosed with cancer present with
symptoms, most of these to primary care
• Many don’t fulfill current urgent referral
criteria…(NICE updates are due..)
• Tools can help aid referral decisions
• AID not REPLACE clinical judgement
• Two different tools have been developed:
Hamilton risk
assessment tool
Qcancer
http://www.qcancer.org/
Risk assessment tool- mouse mat & easel
Primary Care Cancer Risk Assessment Tool
NICE guidance implies risks above 3% require urgent referral. These tools help you
to decide which patients below this level may benefit from urgent investigation
To be used to supplement NICE guidance
For patients aged 40 and over
To calculate the risk value:
o For a single symptom, read the value from the top row
o For a single symptom presented more than once, read the value from
the cell on the left hand diagonal
o For multiple symptoms, read the value from the cell combining the
worst 2 symptoms
Amber and red risk values suggests 2WW referral; yellow and white may well
be best managed by review within primary care, but use your discretion
Macmillan Cancer Support- Early Diagnosis
Programme
(Links to papers / guides to both)
CEG – Cancer risk assessment template
Integration into Emis web – on the way…
Increasing uptake of bowel screening
• Based on what we know from local pilots
works
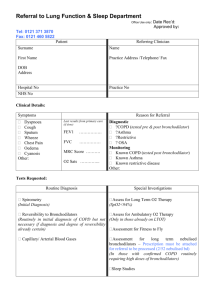
Lung Cancer - targeting the high
risk groups
• Leading cause of cancer death
• Others improved mortality rates
Lung unchanged..
• 5 yr survival <10% locally (CRC 50.2%)
• Present LATE (80% stage III&IV)
Take home points
• Musculoskeletal sounding pain (neck or shoulder) can be a presenting
symptom have a low threshold for CXR
• Heightened suspicion of lung cancer in patients with worsening COPD or
new or persistent COPD symptoms
• NICE guidance : newly diagnosed COPD need CXRs
(NIS outcome measure)
Lung cancer cannot be excluded even if a CXR is normal
REFER IF SUSPECT
don’t be falsely reassured
Screening for lung cancer…
• USA: 50,000 patients, 50% had a CT scan every
3 years
• 20% fewer lung cancer deaths in the CT group
• Proven to reduce lung cancer deaths
• Smokers are a clearly defined cohort
Watch this space…Pilots planned in UK to
evaluate use further
Lung cancer Incidence Rates
per 100,000 Population, by Sex, UK
This afternoon
- GP, Secondary Care & Public Health Input
- Finer brush strokes!
- Macmillan resource packs for GPs
- Screening resources