PROTEIN BINDING
advertisement
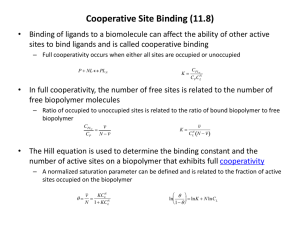
PROTEIN BINDING Roselyn Aperocho-Naranjo Faculty, College of Pharmacy USPF Binding of drug to proteins may: Facilitate the distribution of drugs Inactivate the drug by not enabling a sufficient concentration of free drug to develop at a receptor site Retard the excretion of a drug The interaction of drugs to protein may cause: Displacement of body hormones or coadministered agent Change the configuration of protein to another structure capable of binding a coadministered agent Inactivates the drug biologically by forming a drug-protein complex Structure of Binding Site of ColonCancer Drug and Its Protein Target Schematic showing how Erbitux takes the place of the EGFR growth factor, thereby inhibiting cancerous growth. Two Important Plasma Proteins ALBUMIN Is the most important protein that binds to drug molecule due to its high concentration compared with other proteins It binds both acidic and basic Constitute 5% of the total plasma Two Important Plasma Protein ∂1-ACIDGLYCOPROTEIN Also known as orosomucoid (∂1-globulin) Binds to numerous drugs Have greater affinity for basic than acidic drugs molecules Binds only basic and highly lipophilic drugs Things to remember: Many drugs bind to the same receptor site but drugs with higher affinity will replace those drugs with lower affinity by competition Only free and unbound drugs exert therapeutic effect by interacting with receptors Drugs may bind to protein through: Hydrophobic Interaction Proposed by Kauzmann tendency to develop of hydrophobic molecules or parts of molecules to avoid water because they are not readily accommodated in the H-bond structure of water Binding of Ca to a target protein Drugs may bind to protein through: Self-Association Some drug may self dissociate to form dimers, trimers or aggregates of larger size Dimers or trimers - is a reaction product of two or three identical molecules May affect solubility, diffusion, transport, therapeutic action of drugs Amino Acids A. Basic Group Arginine Histidine Lysine bind Acidic Drugs bin d Basic Drugs Amino Acids B. Acidic Group Aspartic Acid Glutamic Acid Protein binding is determined by: Dialysis Ultracentrifugation Ultrafiltration Sephadex-gel filtration Molecular filtration Electrophoresis Agar plate test The Pharmacokinetic Importance of Protein Binding Drug-protein binding influences the distribution equilibrium of the drug Plasma proteins exert a buffer and transport function in the distribution process Only free and unbound drug acts can leave the circulatory system and diffuse into the tissue Disease and Protein Binding Protein binding will be affected by the presence of diseases Drugs showing Decrease Extent of Protein Binding in the following diseases: LIVER RENAL Dapsone Diazepam Morphine Phenytoin Prednisolone Quinidine Tolbutamide Triamterene Barbiturates Cardiac Glycosides Chlordiazepoxide Clofibrate Diazepam Diazoxide Furosemide Morphine Phenylbutazone Phenytoin Salicylates Sulfonamides Triamterene Disease and Protein Binding When drugs bind to protein, Albumin concentration is reduced The exchange of proteins between plasma and interstitial compartment (normally proceeds at a rate of 5% plasma protein per our) will be hampered. The diffusion of plasma the to interstitial fluid is increased by: Inflammatory process Pregnancy use of oral contraceptives Diabetes Septic shock Pulmonary Edema Disease and Protein Binding The reduced albumin concentration and binding capacity is due to: Change in albumin molecule presence of endogenous binding inhibitors such as free fatty acids, and metabolic acidosis. Disease and Protein Binding Hypoalbuminemia may result in patients with cancer, burms, cardiac failure, cystic fibrosis, enteropathy, inflammations, liver impairment, malabsorption, nephrotic syndrome, renal failure, sepsis and trauma. Disease and Protein Binding Pathological Conditions in which Plasma Concentration of ∂1ACIDGLYCOPROTEIN is increased Cancer Carcinoma, Leukemia, Lymphoma, Malignant melanoma, myeloma Inflammation Crohn’s disease, Inflammatory polyarthritis, pneumonia, rheumatoid arthritis, ulcerative colitis, systemic erythematosus Myocardial Infarction Trauma Burns, extensive tissue damage, surgery, transplantation Binding of Drugs to RBC Lipophilic molecules dissolved in the lipid material of the RBC membrane Anions can be attracted to and enter the positively charged pores of RBC Lipopilic drugs may be absorbed to rBC membrane due to change of: Change of shape of membrane and membrane proteins Membrane extension which may lead to chane of RBC shape Drugs absorbed in the RBC membrane inhibits the deformity of RBC thus becoming lodged in the capillaries Macrophages may remove the RBC, that results in increase free drug concentration Binding of drugs to RBC may be dependent on age (meperidine) and concentration dependent (diazepam) The RBC binding sites are: Intracellular proteins Hemoglobin Carbonic anhydrase Cell membrane ATPase Beneficial effects of tissue binding: Lower tissue uptake Lesser retention in critical organ such as kidney, etc. Displacement of drugs from Protein Binding is due to: Total amount of protein-bound drug in that body Extent of tissue binding structure Apparent volume of distribution Displacement of Drugs from their Plasma Protein Binding by Other Drugs given concomitantly Drug Displaced By Concomitant Drug Warfarin and other highly bound coumarin-type anticoagulants Clofibrate Phenylbutazone Ethacrynic acid Mefenamic Acid Nalidixic Acid Oxyphebutazone Chloral hydrate Tolbutamide Phenylbutazone Salicylates Sulfafurazole