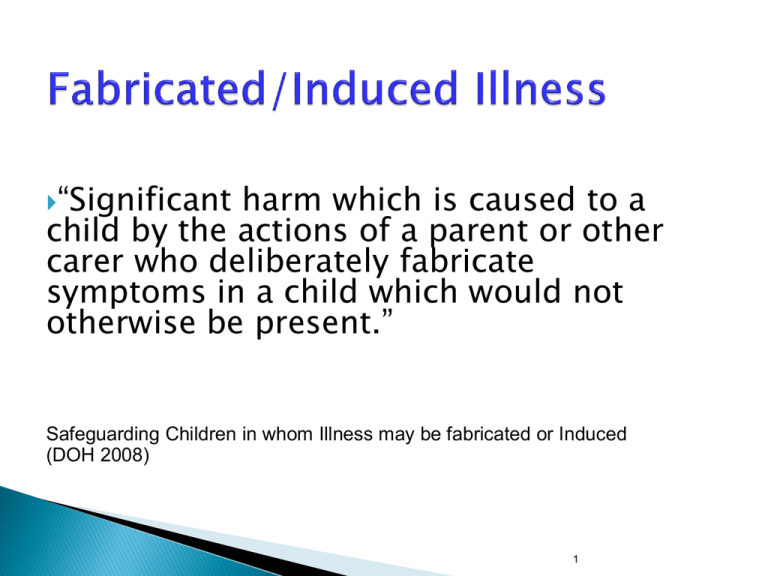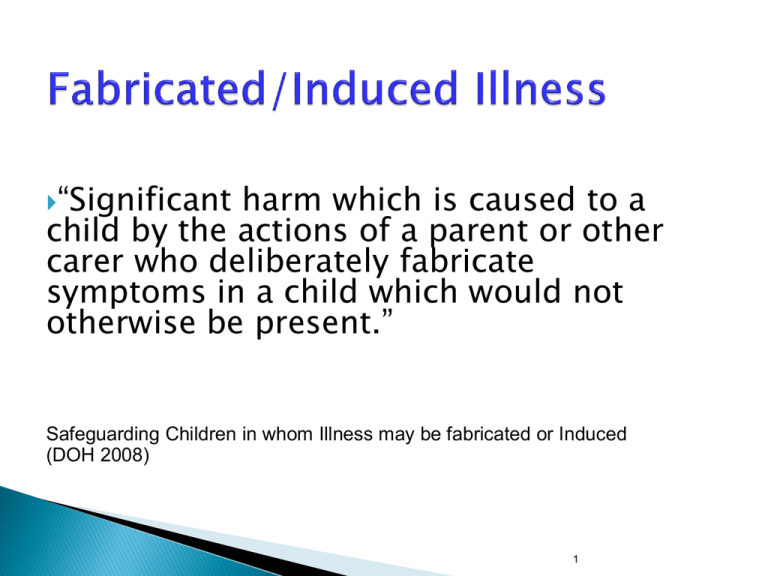
“Significant
harm which is caused to a
child by the actions of a parent or other
carer who deliberately fabricate
symptoms in a child which would not
otherwise be present.”
Safeguarding Children in whom Illness may be fabricated or Induced
(DOH 2008)
1
•
•
•
Fabrication – signs and symptoms past
medical history
Falsification – hospital charts and records;
specimens of body fluids; letters and
documentation
Induction – by a variety of means
2
At the point of “dawning” practitioners should consult a
Named Nurse/Doctor without delay for advice.
The child must be made safe whilst the investigation is
ongoing.
Suspicions should not be discussed widely.
The parent/family must not be informed.
When, in discussion with the Named Professional, it is
thought that there is some foundation to suspect the
abuse, a referral must be made to Children’s Social Care
3
“Emotional abuse is the persistent emotional illtreatment of a child such as to cause severe and
persistent adverse effects on the child’s emotional
development.
…Some level of emotional abuse is involved in all
types of maltreatment of a child, though it may occur
alone.”
WTSC 2013
4
Conveying to children that they are worthless or unloved,
inadequate, or valued only insofar as they meet the needs of
another person.
May include not giving child opportunities to express their views,
deliberately silencing them or ‘making fun’ of what they say or
how they communicate.
May feature age or developmentally inappropriate expectations.
Overprotection and limitation of exploration and learning or
preventing the child participating in normal social interaction.
Seeing/hearing ill treatment of another.
Serious bullying (including cyber-bullying) causing children to
feel frightened or in danger.
May involve exploitation or corruption.
“Sexual abuse involves forcing or enticing a child or
young person to take part in sexual activities, not
necessarily involving a high level of violence,
whether or not the child is aware of what is
happening”
Physical contact, including penetrative (e.g. rape or
buggery) or non-penetrative acts.
Involving children in looking at, or in the production of,
pornographic material.
Watching sexual activities.
Encouraging children to behave in sexually inappropriate
ways.
Grooming a child in preparation for abuse.
WTSC 2013
6
“Sexual exploitation of children and young people under 18 involves
exploitative situations, contexts and relationships where young people
(or a third person or persons) receive ‘something’ (e.g. food,
accommodation, drugs, alcohol, cigarettes, affection, gifts, money) as a
result of them performing, and/or another or others performing on
them, sexual activities.
Child sexual exploitation can occur through the use of technology
without the child’s immediate recognition; for example being persuaded
to post sexual images on the Internet/mobile phones without immediate
payment or gain.
In all cases, those exploiting the child/young person have power over
them by virtue of their age, gender, intellect, physical strength and/or
economic or other resources.
Violence, coercion and intimidation are common, involvement in
exploitative relationships being characterised in the main by the child or
young person’s limited availability of choice resulting from their
social/economic and/or emotional vulnerability.
2009 Guidance
Going missing for periods of time or regularly
coming home late;
Regularly missing school/not taking part in
education;
Appearing with unexplained gifts or new
possessions;
Associating with other young people involved in
CSE;
Having older boyfriends or girlfriends;
Suffering from sexually transmitted infections;
Mood swings or changes in emotional wellbeing;
Drug and alcohol misuse;
Displaying inappropriate sexualised behaviour.
2009 Guidance
Neglect is the persistent failure to meet a child’s
basic, physical and/or psychological needs, likely to
result in the serious impairment of the child’s health
or development. Neglect may occur during
pregnancy as a result of maternal substance misuse.
Once a child is born, neglect may involve a parent or
carer failing to:
provide adequate food, clothing and shelter;
protect a child from physical and emotional harm or danger;
ensure adequate supervision;
ensure access to appropriate medical care or treatment.
WTSC 2013
9
•
Dirty clothes/skin/nails/odour;
•
Chronic infestation;
•
Hair matted or thin;
•
Chronic nappy rash;
•
Infected sores (especially in skin folds);
•
A long history of illness, accidents, ingestions and
repeated hospital admission;
•
Delay in presentation to health professionals.
10
1.
Listen and observe
2.
Seek an explanation
3.
4.
5.
Record what is observed and heard and why
this is a concern
Either consider, suspect or exclude child
maltreatment
Record actions taken and the outcome
CG89 When to suspect child
maltreatment: quick reference guide
Available at:
<http://guidance.nice.org.uk/CG89/Quic
kRefGuide/pdf/English>
Listen carefully and take it seriously
Reassure children they are right to tell
Negotiate getting help and obtain help quickly
Do not jump to conclusions
Ask open questions
Do not make promises you cannot keep – in
particular, never promise confidentiality
Do not make the child repeat what he or she has
said to another member of staff
In addition to previous slide –
Try to ascertain if the perpetrator may still pose a risk to
children. If so, you have a responsibility to protect
those children
Encourage and support the adult in disclosing as much
information as they are willing and refer the child/ren to
Social Care Services
Provide information about services
Ask adult to consider a formal disclosure to the Police
It is your last patient on Friday afternoon
before a Bank Holiday.
Whilst carrying an examination on a 6 week old
baby boy you notice what appears to be a
fading bruise on his forehead and another on
his left cheek. You draw these to the attention
of his mother who says that she does not know
how they were caused, but thinks he might
bruise easily. She thinks he may have hit
himself with a toy.
Are these marks significant.
What action will you take in the short term?
You discuss the child with the Paediatric
SpR on call and agree to send the child to
CAU. The mother explains that she needs to
collect the other children from their
granny’s and she’ll take him up as soon as
she has done so.
After you have made the referral whose
responsibility is it to ensure they arrive at
the hospital?
You are asked by the Health Visitor to examine
a 3 year old child who has a badly infected toe.
Mother reports that the child injured his toe two
to three weeks previously, and for the last five
to six days it has been red and inflamed and
obviously causing the child some distress.
The mother apologises for the state of the
child, who is dressed in dirty clothes, and all
exposed areas are also covered in dirt. She
says he had been playing outside when the
Health Visitor visited and insisted he was taken
to the doctor.
cont…
Mother is seven months pregnant, looks tired
and unwell and has a fading bruise on her left
cheek. You note she has an older child aged
5 who is at school.
Discuss the issues raised by this scenario and
prioritise your actions.
The receptionist witnesses a mother of two
young children aged 3 and 5 hitting them
across the head in the waiting room of your
surgery. The children had been very noisy
and disruptive in the waiting room whilst
waiting to see the doctor.
What should the receptionist do?
What should the doctor/nurse do?
The Practice Nurse is told by a patient that a
man that she knows is a sex offender has
moved in to live with her next door neighbour
who has three young children.
What should the GP/Practice Nurse do?
GP is contacted by telephone. The caller says
she works for Children’s services and needs
some information about a family where a
child may be at risk. She says that she will
require photocopies of the child’s notes and
that a colleague will drop into the practice in
the morning to collect the copied notes.
What is your response?
Sam is 14. He has a life limiting condition
and the family understand that he is unlikely
to reach adult life.
The family call the medical centre first thing
in the morning , leaving a message to tell you
that Sam died in the night.
What should you do?
Who should you inform?
Mrs. Roberts brings her granddaughter, 14
year old Alice, to see you. She is requesting
contraception for Alice.
Alice is a physically mature girl who is
home educated. She is polite and quiet in
clinic and appears to be content playing
with a Barbie doll.
Mrs Roberts is concerned that Alice is a
little immature. She feels Alice would be
safer on the pill.
Mother brings her 12 year old daughter to
surgery. The 12 year old has disclosed to
her that she has had sex two weeks
previously. She will not disclose the
identity of the other person and has refused
to speak to the Police.
What should you do, who would you take
advice from and what advice would you give
the mother?
A baby is brought for routine
immunisations by a woman who describes
herself as his auntie.
Should the immunisation be given?
What are the issues that need to be
considered?
CP PROCESS
Referral to Social Care
ROLE OF GP
-Identification of concerns
-Timely & detailed referral
Assessment
Sharing of proportionate
information re children &
parents/carers
Strategy Meeting/ Discussion
Attendance (if possible)
Initial Child Protection
Conference
- Submission of reports
regarding all children &relevant
information re parents/carers
- Attendance (if possible)
Core Group Meetings to
develop Child Protection
Plan
GPs unlikely to be member of
Core Group
Review Child Protection
Conference/s until Plan
no longer required
Submission of reports regarding
all children and relevant
information re parents/carers
i. Policies and Procedures
iv. Inter-agency
partners
ii. Training
iii. Access to advice and support
Wyllie E., 2010
North Yorkshire LSCB Procedures
(supporting protocols including Pre-Birth
Protocol)
www.safeguardingchildren.co.uk
City of York LSCB Procedures
www.saferchildrenyork.org.uk
NYLMC Child Protection Guidelines
Practice Policy
Over a three year period, professionals should receive
refresher training equivalent to 1 – 1.5 PAs/sessions (for
those at Level 3 core this equates to 0.5 PA per annum).
Training, education and learning opportunities should be
multi-disciplinary and inter-agency, and delivered internally
and externally. It should include personal reflection and
scenario-based discussion, drawing on case studies and
lessons from research and audit. This should be appropriate
to the speciality and roles of the participants.
RCPCH (2010) Intercollegiate Document
http://www.rcpch.ac.uk/safeguarding
Lead GP for Safeguarding within practice
Named Doctor or on-call paediatrician
Designated Doctor or Nurse - role is to
provide advice, support and supervision
(consulting your Designated professionals
does not constitute a child protection
referral).
‘Hypothetical’ discussion with Children’s
Social Care or Police – no names
Are contact numbers readily available?
Identify key individuals from your local
partner agencies (Children’s Social Care;
Protecting Vulnerable Person’s Unit; Women’s
Refuge, etc.)
Are local contact numbers readily available to
all staff in the practice?
RCPCH Toolkit (2011)
- Contents
Aim of the Toolkit
What is Safeguarding?
Who is Responsible?
Why is Safeguarding
Necessary in General
Practice?
Barriers
Barriers to Children Telling
Monitoring and Reviewing
Parental Responsibility
Practice Policy and Procedure
Working in Partnership with
Parents
Domestic Violence
Thank you
and
good luck!