David Watson Migraine Management presentation
advertisement

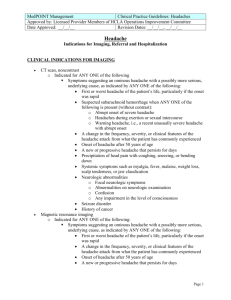
Dr David PB Watson Hamilton Medical Group Aberdeen Theories of Migraine Acute Treatment Prevention Case Studies A chronic disorder with episodic attacks Complex changes in the brain During attacks – – – Headache Several associated symptoms Functional disability In-between attacks – – Enduring predisposition to future attacks Anticipatory anxiety Cortical events Meninges and other peripheral structures TNC Trigeminal ganglion Brainstem Neuropeptides TGS = trigeminal system; TNC = trigeminal nucleus candalis. Bigal ME et al. Neurology. 2008;71:848–855; Brandes JL. Headache. 2008;48:430–441; Coppola G et al. Cephalalgia. 2007;27:1429–1439; Goadsby PJ et al. N Engl J Med. 2002;346:257–270; Haut SR et al. Lancet Neurol. 2006;5:148–157; Lovati C et al. Headache. 2008;48:272–277; Pietrobon D. Neuroscientist. 2005;11:373–386. Premonitory Mood changes Fatigue Cognitive changes Muscle pain Food craving Preheadache Aura Early Headache Fully reversible Dull headache Neurological changes: Nasal congestion Visual somatosensory Muscle pain Mild Unilateral Throbbing Nausea Photophobia Phonophobia Osmophobia Moderate Headache Cady R et al. Headache. 2002;42:204–216. Linde M. Acta Neurol Scand. 2006;114:71–83. Linde M. Cephalgia. 2006; 26; 712–721. Advanced Headache Postdrome Severe Fatigue Cognitive changes Muscle pain Post headache Time Advanced Headache Unilateral Throbbing Nausea Photophobia Phonophobia Preheadache Severe Headache Phase Cady R et al. Headache. 2002;42:204–216. Linde M. Acta Neurol Scand. 2006;114:71–83. Linde M. Cephalgia. 2006; 26; 712–721. Postheadache Time The case for the sensitive migraine brain Normal life events trigger or are associated with attacks in those predisposed Dehydration Sleep disturbance Hunger Stress Diet Environmental stimuli Changes in oestrogen level in women CNS = central nervous system. Coppola G et al. Cephalalgia. 2007;27:1429–1439; Kelman L. Cephalalgia. 2007; 27:394–402; Pietrobon D et al. Nat Rev Neurosci. 2003;4:386–398. Headache threshold variability Patient 4 Patient 3 Patient 2 Patient 1 Trigger Beware of using painkillers more than 2 days a week Medicines taken during a headache to reduce or put the pain away and to help sickness Painkillers Anti-sickness medications Migraine specific medicines Triptans Ergotamine (Cafergot, Migril includes cyclizine and caffeine) Best evidence ASPIRIN 900 mg IBUPROFEN 400 mg In pregnancy PARACETAMOL 1000mg Take early in headache May be combined with anti-sickness medicines such as Domperidone, Metoclopramide and Prochloroperazine Migraleve = paracetamol, codeine, (yellow) buclizine (pink) MigraMax = aspirin and metoclopramide Paramax = paracetamol and metoclopramide Clotam Rapid = Tolfenamic Acid Almotriptan Eletriptan Frovatriptan Naratriptan Rizatriptan Sumatriptan Zolmitriptan Brain Nerve Blood Vessel Decreased pain Decreased pain transmission Decreased pain transmission Decreased Decreasain BBbBion pain transmission transmissioned transmission p Early in the headache phase Not during aura Can repeat after 2hours if migraine recurs No response, don’t repeat Response idiosyncratic Tablet ( gastric absorption) Melts (gastric absorption) Nasal Spray ( Gastric and nasal absorption) Injection ( subcutaneous) Most patients have few problems Sensations of tingling, heat, heaviness, pressure, tightness of throat or chest Flushing Dizziness Feeling of weakness, fatigue Nausea and vomiting Take early in headache phase Rescue Treatment (include rectal) Naproxen Consider if frequent debilitating migraine Not a cure Good response is works in 50 out of 100 patients to reduce headache frequency and severity by half Can be combined Need adequate doses Headache threshold variability Patient 4 Patient 1 Preventer Patient 3 Patient 2 Patient 1 Trigger B Blockers Tricyclic Antidepressants Anti Epileptics Pizotifen Venlafaxine Candesartan (Flunarazine) (Methysergide) Propranolol 80-240 mg Avoid in asthma Side Effects (rarely a problem) Fatigue Coldness of extremities Sleep disturbance and nightmares Gastro intestinal disturbance Dizziness Headache Amitriptyline 10 -125 mg Nortriptyline 10-125 mg Patient Information Leaflet = anti-depressant Side effects Sedation Dry mouth Constipation Headache Sodium Valproate 600-1200 mg daily Weight gain Hair Loss Nausea, Diarrhoea Topiramate 50-150 mg daily Weight Loss Sedation and slowed thinking Irritability and Depression Pins and Needles Start low and aim high Combinations can be effective Consider reducing/stopping in 6-12 months 25 year old lady Migraine with aura twice a month, always with menstruation. Can vomit late in headache. Menstrual migraine can be 2 days Never misses work Migraine can be present on waking Aspirin 2 tabs partially helps some headaches Consider Dose. Aspirin 900 mg helps day time migraine Timing. Taken early in headache works better Nausea/vomiting . Required triptan for menstrual migraine Rescue = triptan 37 year old lady, 4 migraine without aura a month, last 2 days each Misses 3 days of work a month Can vomit within 2 hours Naratriptan helps some time Consider Take triptan early Faster acting triptan Nasal triptan Naproxen Rescue Rx suppositories