Headache
advertisement

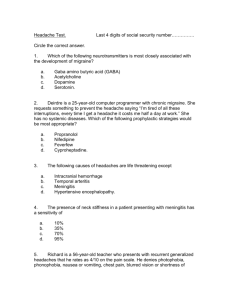
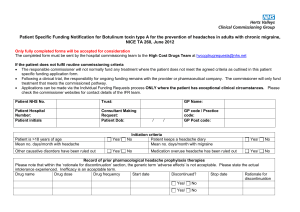
Headache diagnosis and treatment : now and the future Paul Rolan MBBS MD FRACP FFPM DCPSA Professor of Clinical Pharmacology Senior Consultant, Pain Management Unit, RAH Headache • in 99.9% of people with headache there is no sign of tissue damage • injuring the brain itself does not cause pain – it causes altered brain function • however the membrane and blood vessels of the brain are very pain sensitive Headache: causes • Primary (99%+) • • • • • Tension – type Migraine Stabbing Exertional Cluster 69 16 2 1 0.1 • Due to something else (<1%) • Systemic infection • Head injury • Vascular / bleeding 63 4 1 • Brain tumour 0.1 Headache diagnosis • almost entirely on the patients story • tests, scans etc rarely helpful. Headache: history • • • • • • • • • • • • How old were you when the headaches started? How often do they come? Do they come in relationship to anything else? At what time do they come on? How do they start? Where is the pain? How long does it last? How bad is it? Are there other symptoms? Does anything bring it on? What helps? How long does it last? Pattern recognition pick the odd one out Tension-type Headache • Frequency chronic often daily • Pain mild-moderate pressure, tightness • Duration 30 mins - 7 days • Location both sides whole head and neck • Symptoms no light / sound sensitivity no aura Typical patient : any Typical patient : any Tension-type headache • now thought to be due to increased brain sensitivity to normal sensory inputs • few effective treatments : we are trialling a non-drug treatment Migraine (“half-head”) • Frequency 1-2/year- 2-3/week • Pain moderate - severe pulsating, throbbing • Duration 4 hrs - 3 days • Location usually one sided (but side can swap between attacks) • Symptoms aura nausea, vomiting sensitive to light, sound, smells Typical migraine patient • onset often as child / teenager / young adult • but can start at any age • 2-3 x more common in women than men • typical patient : young woman (15% of all young women) What happens during a migraine? Migraine cause • cause unknown but strongly inherited • a lower threshold to spontaneously produce symptoms as if the head and brain had been injured • many effective treatments Triggers • • • • • foods : spices, wine , chocolate, citrus food additives : monosodium glutamate sleep : both too much and too little stress : mainly offset female hormones : fluctuating or falling oestrogen Migrainous Aura Migrainous Aura Migrainous Aura Medication overuse headache • headache made WORSE by pain killers • only occurs in people who already had headache • mainly due to codeine-containing medicines or stronger morphine-like drugs • need to stop responsible medicines : easier said than done • we are trialling a new treatment for this Cluster Headache • Frequency clusters – every time each year or season; then free • Pain excruciating penetrating, boring continuous, non-throbbing • Duration 15mins-3 hrs; same clock time each day (2am); several episodes / day • Location ALWAYS the same side • Symptoms watering eyes nasal stuffiness, runny nose red eye, swollen eyelids sweating Typical patient : middle aged male smoker Cluster Headache Trigeminal Neuralgia • VERY short (<1 sec) severe pain • Knife-like • Local triggering : eating etc Typical patient : middle aged / elderly woman Other headaches • Paroxysmal hemicrania • “SUNCT” – short lasting neuralgiform;conjunctival injection, tearing • • • • Stabbing headaches After head injury / head surgery Sexual headaches Altitude sickness Treatment Explanation, set realistic objectives Treatment of the attack Treatment to reduce attack frequency Lifestyle change Treatment of the attack 1 2 3 General pain relievers Migraine-specific treatments - triptans and ergots Cluster specific treatment - oxygen - triptans General pain relievers : migraine, tension aspirin Fast? ✔✔ codeine tramadol ✔ ✔ ✔✔ Safe? OK for long term? paracetamol ibuprofen ✖ ✔✔ ✖ ✖✖✖ Additives : metoclopramide (nausea) caffeine Not suitable : dextropropoxyphene “Doloxene; Di-Gesic” morphine, pethidine Triptans : Imigran, Zomig, Naramig, Maxalt, Relpax FOR • can be very effective : migraine, cluster (NOT tension) • tablets, wafers, nasal spray, injection • AGAINST • feel strange, chest pain • expensive, small supply • overuse makes headaches more frequent • constrict blood vessels Ergots : migraine, cluster FOR • can be very effective when others fail • nasal spray, suppository injection • AGAINST • hard to get • overuse causes poor circulation and more headache • not for tension Preventative drugs • “mixed bag” of drugs used for other conditions found to be effective in headache usually by chance • usually for high blood pressure, depression, epilepsy • all work in somebody ; none works in everybody • generally reduce frequency but do not change attacks • key to success : trial and error : persist • need to start at low dose and increase until effective or not tolerated • about 50 % of patients will get 50% or more reduction in attacks Main migraine preventers Effectiveness Tolerability / safety Good Fair Poor Good propranolol verapamil Botox Fair amitriptyline topiramate valproate pizotifen ibuprofen Poor methysergide Tension preventers Effectiveness Tolerability / safety Good Fair Poor Good Fair Poor amitriptyline ibuprofen Cluster preventers - balance of effectiveness and safety / tolerability Effectiveness Tolerability / safety Good Fair Good verapamil Fair topiramate Poor methysergide steroids Poor lithium Non drug Herbal •feverfew – no •butterbur – possibly Manual therapies •physiotherapy – caution •acupuncture – no Electrical occipital nerve stimulation : possibly Closure of hole in heart - no In the pipeline In the pipeline • “vaccination” for migraine • new classes of drugs Our research • we are trialling a non-drug electrical therapy for tensiontype headache • we are trialling a completely new drug approach to medication overuse headache • we may be trialling new agents for migraine in the near future http://www.adelaide.edu.au/painresearch/participate/