Palliative Care - Rachel Dawson

Palliative Care
Dr Rachel Dawson
Objectives
Increase your confidence in dealing with palliative care cases
Content
Who is a palliative care patient?
Presentation/ likely symptoms
Palliative care emergencies
Help available
Medication – what, when & how much to use
Setting up a syringe driver
Case studies/ ethical dilemmas
Who Is a Palliative Care
Patient?
A patient for whom the objective of any treatment is to
offer symptom relief only
For example –
- Any end-stage chronic illness; cancer, heart failure, renal failure, COPD, MS
….
- Dementia
- Old age
It is NOT just for cancer patients
Common Symptoms
(PEPSI COLA)
Pain
Drowsiness
Breathlessness
Nausea / Vomiting
Constipation
Anxiety/ Agitation / Restlessness/ Confusion – remember carer
Dysphagia
Other symptoms are more common in certain scenarios e.g. ascites in ovarian cancer
Palliative care Emergencies
Hypercalcaemia
Spinal cord compression
SVC obstruction
GI obstruction
Haemorrhage – esp Upper GI
( Raised ICP)
Palliative Care Emergencies
– Hypercalcaemia
Calcium > 2.6mmol/l
Suspect if known bony mets or any common tumour; Breast/ kidney/ myeloma/ lung or CRF
Symptoms – non-specific : thirst, constipation, N/ V, Abdo pain, anorexia
Management – STOP any calcium (!) & admit for re-hydration & IV Pamidronate
Palliative Care Emergencies –
Spinal Cord Compression
Incidence of ~5% of all cancer patients
– 70% occur in T spine
Always suspect if known bony mets/ common metastasising tumours
Symptoms include – pain / leg weakness/ constipation/ incontinence
Management: ADMIT – IV
Dexamethasone, MRI & RTx
Palliative Care Emergencies –
GI Obstruction
Can occur with any cancer – not just physical obstruction
Symptoms include – V (faeculent),
Constipation (empty rectum), Abdo distension, Pain
Management - ? Admit, ? NGT, Consider stopping prokinetic (dom/ met) & switch cyclizine/ haloperidol, buscopan. Soften stool
& consider dexamethasone
Palliative Care Emergencies –
SVC Obstruction
Rare – 75% are due to 1y lung cancer.
~3% lung cancers develop SVCO
Symptoms – periorbital oedema, SOB/ stidor, neck or arm swelling. Usually dilated veins can be seen on chest wall.
Management – Treat breathlesness/ anxiety with opioid +/- BZD. ADMIT – IV dexamethasone & RTx
Palliative Care Emergencies-
Haemorrhage
Rare, but most common with upper GI
(Remember steroids)
Usually fatal
Need to anticipate / warn carer
Management – Midazolam +/diamorphine to alleviate suffering
Palliative Care Emergencies
(7)
Raised ICP – presents with drowsiness/ headache/ V. Can usually be anticipated. Mx= dexamethasone
16mg/day
In essence emergency drugs include –
Diamorphine, Anti-emetic, Midazolam &
Dexamethasone
Help Available
-
-
-
-
-
-
COMMUNITY
District Nurses ->LCP
Macmillan Nurses
Hospice at home ->LCP
Consultants
Pharmacist – Twycross/
Pall care BNF
Bradford Cancer
Support ->benefits
-
-
-
HOSPITAL
Consultants
Specialist nurses
2 nd opinion
Medication – What, When &
How Much to Use
Analgesia
Antiemetic
Anticholinergics
Sedatives/ Anxiolytics
Anti-inflammatory
Others – secretions, mouth care & constipation.
Analgesia
Tailor analgesic choice to type of pain – may need a combination
Give clear instructions
Gradually increase dose
Give regular dosage +/- PRN
Consider potential SE & co-prescribe
Follow up to ensure ok
Analgesia – Types of Pain
‘Standard’ = WHO Analgesic ladder = Opioid
Bony pain – consider NSAID, RTx,
Bisphosphonates
Neuropathic – Opioids, Gabapentin,
Pregabalin
Abdo Spasm – Anticholinergics
Muscular – NSAID, Baclofen, BZD’s
Analgesia - Types
Non-opioids: Paracetamol, NSAID
Weak Opioid : Codeine,
Dihydrocodeine, Tramadol
Strong Opioids : Morphine (1 st line),
Diamorphine, Fentanyl, Oxycodone,
Hydromorphone, Methadone
Others – Ketorolac; Ketamine
Analgesia – choice
Choose on basis of type of pain, route of delivery & previous analgesia used
1 st line build up ladder to morphine.
Start regular oromorph eg 5-10mg qds + prn.
Review amounts used & convert to MST. Can then convert to diamorphine as necessary.
Switch to oxycodone/ hydromorphone / fentanyl if morphine SE
REMEMBER to co-prescribe + PRN
Antiemetic
Likely to be used a co-prescription or to reduce established nausea.
Try simple meds 1 st line
1 st line = Cyclizine, Stemetil, Metoclopramide
Consider other choices if co-existing symptoms e.g. Haloperidol, Dexamethasone
Can use combinations.
Doses may be higher eg 60-100mg metoclopramide over 24hrs.
Avoid Metoclopramide if obstruction
Agitation/ Anxiety
Consider reversible causes inc pain
Consider non-drug treatments
Consider underlying depression
Medication: Haloperidol, BZD’s
Shortacting BZD’s eg lorazepam s/l
Sedating BZD’s eg Midazolam s/c
Sedatives eg Phenobarbitol
Other meds
Secretions – consider hyoscine patch or s/c
Constipation – try & avoid with coprescribing
- Prescribe regular laxatives
- Remember Co-danthrusate/ docusate
- Seek nurse advice/ involvement
Mouth Care – consider saliva sprays/ gel
Other meds - dexamethasone
Has multiple uses at different doses & compatible in syringe drivers
Anorexia - 2-4mg/ d
Raised ICP – 16mg/d
Gut obstruction – 4-8mg/d
Hiccoughs – 4-12mg/d
Anti-inflammatory – 4 –16mg/d
Medication example
If opioid naïve a good starting point for oral route:
Oramorph PRN & convert OR 10mg MST bd, then review. PLUS…
Cyclizine 50mg tds. PLUS…
Movicol1 sachet 2-4x per day
Review regularly & if problems – seek help
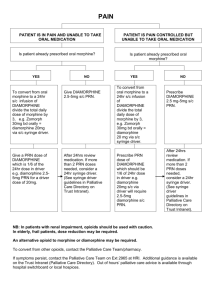
When
Syringe Drivers –
When, What , How
- Try & anticipate
- Team decision
- Can always be stopped
- Ensure family aware.
- Communicate well
- STOP all other meds
What
-
-
-
-
-
Diamorphine (510mg if naïve)
Cyclizine (150mg) &/or Metoclopramide
(60mg)
WFI
+/- Midazolam – 20-30mg/24hrs initailly
Ensure stat doses available & instructions to increase after 24hrs if necessary.
Special instructions eg GI haemorrhage.
How
-
Inform/ Involve family in decision
Inform DN’s or H at H
- Prescribe meds
-
- Write up instructions – Syringe driver & stat sheet. Be clear.
Inform LCD – fax
Ensure follow up in place
Other considerations
Always ensure the person still wishes to remain at home.
Keep family informed & advise re action to take in event of death
Benefits – DS1500
Level 6 care/ Continuing care – poor prognosis
LCD/ OOH form
DNR form for transport
Cases
Conclusion
Hopefully confidence increased
Information packs include:
- Handout
- Yorkshire cancer network booklet
- Dose comparisons of Strong Opioids
- Syringe driver compatability info
- Local pharmacy info
- Forms – DNR, Level 6, LCD, Syringe driver,
PEPSI COLA + DS1500 advice.
Marie Curie Talks