Resp. Drugs
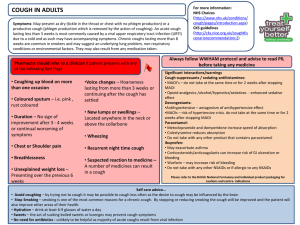
advertisement
LAKSHMAN KARALLIEDDE JANUARY 2011 1. Deliver oxygen to the cells 2.To eliminate carbon dioxide from the body 3.To regulate the pH of the blood VENTILATION Movement of air to and from the lungs DISTRIBUTION Air entering lungs are distributed to all parts including the alveoli DIFFUSION Oxygen from the inspired air diffuses through the walls of the alveoli to the blood capillaries surrounding the alveoli-similarly carbon dioxide diffuses in opposite direction PERFUSION Blood with high concentrations of carbon dioxide and low in oxygen is pumped to the pulmonary arteries by the right ventricle and after diffusion, the arterial blood is returned to the left atrium by the pulmonary veins PASSAGE OF OXYGEN AND CARBON DIOXIDE SOURCE OF OXYGEN – INSPIRED AIR SOURCE OF CARBON DIOXIDE-ALVEOLIFollowing diffusion from the blood due to metabolism in the body. PATHWAY FOR THE GASES: PHARYNX LARYNX-TRACHEA BRONCHI BRONCHIOLES ALVEOLI atmosphere c Carbon dioxide o oxygen Right heartarteries Left heart-arteries Systemic circulation Carbon dioxide oxygen COMMON SIGNS AND SYMPTOMS 1. COUGH 2. WHEEZING 3. SHORTNESS OF BREATH-DYSPNOEA 4. CYANOSIS 5. PAIN AROUND CHEST COUGH – FORCED EXPIRATION AGAINST A CLOSED GLOTTIS WHICH SUDDENLY OPENS TO EXPEL AIR AND UNWANTED MATERIAL FROM THE RESPIRATORY TRACT MAY BE VOLUNTARY OR INVOLUNTARY Mucosal surface lining respiratory tract Impulses relayed via vagus Cough centre in brain Efferent's diaphragm glottis muscles of chest and abdomen Used in treatment of cough The cough reflex- involves both central and peripheral nervous system as well as the smooth muscle of the bronchial tree. 1. Irritation of the bronchial mucosa causes broncho-constriction, which stimulates cough receptors located within the tracheo-bronchial tree.- when coughing as a result of broncho-constriction may be relieved by bronchodilators acting simply to dilate airways 1. Afferent nerves from these receptors via the vagus reaches multiple centres within the medulla that are distinct from the actual respiratory centre. Drugs acting primarily on the peripheral or central nervous system components of the cough reflex. 2. Most effective antitussives have been shown to elevate the threshold for coughing by poorly understood centrally mediated mechanisms. COUGH SUPPRESSANTS Unproductive distressing cough- central cough depressants e.g. pholcodine, dextromethorphan Productive cough-do not use cough suppressants Use expectorants and mucolytics Expectorants-act by increasing the volume of secretions in respiratory tract so that they may be more easily removed by ciliary action and coughing e.g.ammonium salts, guaphenesin, ipecacuanha Mucolytics- considered to affect sputum viscosity e.g.acetylcysteine, bromhexine, carbocisteijne, methyl cysteine The principal non-opioid antitussive Dextromethorphan-has a central action on the cough centre. Morphine and related opioids depress the cough reflex , at least in part by a direct effect on the cough centre in the medulla. Suppression of cough by such agents appear to involve receptors in the medulla that are less sensitive to naloxone than are those responsible for analgesia. Structurally related to morphine but little or no analgesic properties, And minimal (little) sedative activity. Antitussive effects may persist for up to 5 hours. Dextromethorphan should not be administered to patients with or at risk of •Developing respiratory failure. •Do not administer to patients on monoamine oxidase inhibitorsrisk of severe reactions-hyperpyrexia, fatalities PHOLCODINE CENTRALLY ACTING COUGH SUPPRESSANT UNLIKE CODEINE, THERE IS LITTLE OR NO METABOLISM TO MORPHINE LONGER HALF-LIFE THAN CODEINE- DOSES MAY BE GIVEN ONCE OR TWICE A DAY ANTIHISTAMINES E.G. DIPHENHYDRAMINE OFTEN USED AS ANTI-TUSSIVES MODE OF ACTION – UNCERTAIN SUGGESTIONS- a. Reduction in cholinergic transmission b. Suppression of cough because of sedative action c. Reduces nasal secretions and therefore the post-nasal drip that causes cough d. Should not be used to treat productive cough as it increases the viscosity of the mucus The viscosity of pulmonary mucus secretions depends on the concentrations of mucoproteins and deoxyribonucleic acid (DNA). While mucoprotein is the main determinant of viscosity in normal mucus, in purulent inflammation the mucoid concentration of DNA increases (due to increased cellular debris) and so does its contribution to mucoid viscosity. Some patients with respiratory tract disease, the bronchial inflammation will be associated with the presence of large amounts of relatively viscous, inflammatory exudate and mucus which is firmly attached to the lining of bronchioles and bronchi. This would in practical terms increase bronchial wall thickness. Adverse effects of increased mucus accumulation are 1. Increase the "lumen narrowing" effects of bronchial constriction 2. Enhance the overall inflammatory process 3. Potentiate persistent coughing. Mucolytics would be useful in facilitating recovery/relief of symptoms The two most frequently prescribed mucolytics • bromhexine hydrochloride • Acetylcysteine-probably reduces viscosity by splitting the disulphide bonds in mucoproteins • Other forms: Normal saline, directly administered to the airways by effective nebulisation therapy-extremely effective mucolytic and expectorant DORNOSA ALFA ACTS AS A MUCOLYTIC BY HYDROLYSING DNA THAT HAS ACCUMULATED IN THE SPUTUM FROM DECAYING NEUTROPHILS USED AS A NEBULIZING SOLUTION IN PATIENTS WITH CYSTIC FIBROSIS Physiological bronchial tone mediated by three neuro-endocrine systems: 1. Parasympathetic system: dominant efferent pathway providing the baseline tone of mild broncho-constriction - characterizes the normal respiratory tract 2.Sympathetic system -mediates these inherent broncho-constrictive effects through a. beta 2-adrenergic-mediated broncho-dilation b. alpha 1-mediated broncho-constriction c. possibly beta 2-mediated reduction of parasympathetic broncho-constriction 3. The non-adrenergic, non-cholinergic (NANC) system: a. mediates broncho-dilation through various neurotransmitters e.g. Vaso-active intestinal peptide. BRONCHODILATION ACHIEVED • via anticholinergic agents- ipratropium bromide 0.5 mg nebulised repeat every six hours (including beta 2 agonists), • beta 2 adrenergic receptor agonists –nebulised salbutamol (2.5-5.0 mg every two to six hours, terbutaline • agents such as the methylxanthines which produce bronchodilation at least in part due to increased intracellular cAMP levels in bronchial smooth muscle. •Inhaled anti-inflammatory agents- corticosteroidsbeclomethasone or budenoside 100-400 micrograms twice daily • Oral corticosteroids-40-60 mg once daily •Intravenous hydrocortisone- 200 mg every six hours Adrenergic agonists All adrenergic agonists have variable alpha and beta receptor affinity. Due to the distribution of alpha and beta receptorsnon-selective beta receptor agonists such as isoprenaline or mixed alpha and beta receptor agonists such as adrenaline are more likely to produce cardiovascular side effects than similarly administered selective beta agonists. THEREFORE DRUGS WITH PREFERENTIAL AFFINITY FOR BETA 2 RECEPTORS PROVIDE MORE EFFECTIVE BRONCHODILATION WITH FEWER SIDE EFFECTS. A possible exception may be with the treatment of acute allergic bronchospasm. The M-2 receptor-mediated inhibition of cholinergic bronchospasm may be helpful. For this reason, the use of an adrenergic agent with both alpha 2 and beta 2 agonist activity may be beneficial in the peracute management of allergic bronchospasm. Due to risks associated with administering systemic non-selective adrenergic agonists to a hypoxic and already tachycardic patient, it is preferable for them to be administered by inhalation. Selective beta 2 agonists- lead to rapid and effective pulmonary beta 2 receptor activation with low systemic drug concentrations by inhalation of small doses of the drug in aerosol form. METHYLXANTHINES POSSIBLE ACTIONS 1.Relaxation of smooth muscle, particularly bronchial smooth muscle 2.Stimulate the central nervous system 3.Weakly positive chronotropes and inotropes 4.Mild diuretics. Naturally occurring methylated xanthines Caffeine, theophylline and theobromine - relatively insoluble. Solubility enhanced by the formation of complexes with a wide variety of compounds e.g. aminophylline which is the ethylenediamine complex of theophylline with differing quantities of water of hydration. When dissolved in water, aminophylline readily dissociates to its parent compounds. Theophylline has a low therapeutic index- Therefore dose rates should be determined on lean body mass. The dose rate of theophylline varies depending on the preparation used. OPIOID ANTITUSSIVES Widely available at present- codeine phosphate and hydrocodone. Codeine has a high oral-parenteral potency with oral administration providing around 60% of its parenteral efficacy. Once absorbed, codeine is metabolized by the liver . Inactive metabolites excreted predominantly in the urine. In man approximately 10% of administered codeine is demethylated to form morphine -and both free and conjugated forms of morphine can be found in the urine of patients receiving therapeutic doses of codeine. In man, codeine's plasma half-life is around 2 to 4 hours. Codeine phosphate is contained in numerous "over the counter" analgesic preparations as well as in 30 and 60mg tablets which have restricted scheduling. Hydrocodone is generally marketed in combination with homatropine as both an elixir and tablet formulations. The addition of homatropine is designed to enhance any reduction in respiratory secretions, which may come about as a result of the administration of hydrocodone. BENZONATATE Cough suppressant believed to act both centrally and peripherally. Related to amethocaine ( a local anaesthetic) and therefore has a local anaesthetic action on the mucosa. . LEUKOTRIENE RECEPTOR ANTAGONISTS Inflammation of the respiratory tract is frequently characterised by the classical markers of inflammation; •accumulations of inflammatory cells •exudate. •associated with varying degrees of bronchoconstriction •and, or, bronchospasm. • Additionally "airway hyper reactivity" may become a standard response of sensitised patients to various inhaled compounds. Although glucocorticoids remain the "gold standard" in controlling this inflammatory-induced bronchoconstriction, the leukotriene receptor antagonists represent a new class of drugs which may facilitate management of these various forms of bronchoconstriction. DEMULCENTS INDIRECTLY ACTING COUGH SUPPRESSANTS ? MODE OF ACTION POSSIBLY BY PROVIDING A PROTECTIVE COATING OVER THE SENSORY RECEPTORS IN THE PHARYNX EXAMPLES- GLYCEROL, HONEY, LIQUORICE AND SUCROSE SYRUPS HYDRATION 1.LIQUEFYING MUCUS 2.DEMULCENT EFFECT 3.METHODS DRINK PLENTY OF FLUIDS STEAM INHALATION INHALATION OF AEROSOLS CONTAINING WATER, SODIUM BICARBONATE, SODIUM CHLORIDE, SURFACTANTS E.G. TYLOXAPAL PROTEOLYTIC ENZYMES E.G. CHYMOTRYPSIN, TRYPSIN BTS GUIDELINES FOR MANAGEMENT OF ASTHMA 1. INHALED SHORT-ACTING BETA-2 AGONIST AS REQUIRED 2. ADD INHALED STEROID-200800MICROGRMS/DAY 3. ADD INHALED LONG-ATINGBETA 2 AGONIST- CONSIDER INCREASING STEROID INHALED DOSE 4. CONSIDER USING LEUKOTRIENE RECEPTOR ANTAGONIST OR THEOPHYLLINE ADAPTED FROM THORAX 2008;63 (suppl 4): ACUTE BRONCHITIS TREATMENT USUALLY NOT REQUIRED IN PREVIOUSLY HEALTHY PATIENTS BELOW AGE 60 EXACCERBATION OF COPD-START WITH DOXYCYCLINE 200MG OD -SECOND LINEAMOXICILIIN (OR CO-AMOXICLAV) BRONCHIECTASIS-CO-AMOXICLAV 1.2 G TDS IV OR IF AVAILABLE PIPERICILLIN + TAZOBACTAM 4.5 G TDS CYSTIC FIBROSIS- CIPROFLOXACIN 500MG BD ORALLY OR 400MG BD IV IF PSEUDOMONAS IS SUSPECTED Adapted from Pocket Prescriber ADVERSE EFFECTS OF INHALED CORTICOSTEROIDS EXAMPLE BECLOMETASONE 1. ORAL CANDIDIASIS ( decreased by rinsing mouth with water after use) 2. HOARSE VOICE3. RARELY GLAUCOMA 4. INCREASING DOSES MAY CAUSE ADRENO-CORTICAL SUPPRESSION, CUSHING’S 5. DECREASE IN DENSITY OF BONES 6. DECREASE IN GROWTH HORMONE ? 7. Very rarely-paradoxical bronchospasm Adapted from Pocket Prescriber SALBUTAMOL BETA 2 AGONIST- SHORT ACTING ACTIONS: 1. DILATES BRONCHIAL SMOOTH MUSCLE 2. RELAXES UTERINE SMOOTH MUSCLE 3.INHIBITS MAST-CELL MEDIATOR RELEASE BEWARE USE -IN CARDIO-VASCULAR DISEASE Esp. arrhythmias-susceptibility to increased QTc - DIABETES MELLITUS- MAY INCREASE RISK OF DIABETIC KETO-ACIDOSIS - MAY INCREAE THYROXINE LEVELS SIDE EFFECTS- FINE TREMOR, HEADACHE, NERVOUSNESS INCREASE IN HEART RATE, PALPITATIONS, ARRHYTHMIAS DECREASE IN SERUM POTASSIUM MUSCLE CRAMPS Prolonged treatment -? Increased risk of glaucoma THEOPHYLLINE METHYLXANTHINE BRONCHODILATOR- Additive effects with beta 2 agonists but increases risk of hypokalaemia Beware – caution in patients with • Cardiac disease especially risk of arrhythmias, • Epilepsy • Peptic ulcer • Hypertensive heart disease • Fever • Porphyria • In acute febrile illness • Glaucoma • Diabetes mellitus THEOPHYLLINE SIDE EFFECTS• ARRHYTHMIAS • SEIZURES • GASTRO-INTESTINAL UPSET- NAUSEA • RESTLESSNESS, INSOMNIA • HEADACHE • LOWERS SERUM POTASSIUM MONITOR- SERUM POTASSIUM, BLOOD LEVELS 6 HR AFTER ADMINISTRATION TOXIC EFFECTS MAY OCCUR EVEN WITH NORMAL BLOOD LEVELS E.G. 10-20MG/L MONTELUKAST LEUKOTRIENE RECEPTOR ANTAGONIST CAUTION 1. ACUTE ASTHMA 2. CHURG-STRAUSS SYNDROME (asthma with + or – rhinitis, sinusitis with sytemic vasculitis and increased eosinophil counts MONTELUKAST SIDE EFFECTS 1. HEADACHE 2. GASTRO-INTESTINAL UPSET 3. MYALGIA 4. DRY MOUTH/THIRST MONITOR FULL BLOOD COUNT WATCH FOR VASCULITIS PERIPHERAL NEUROPATHY INCREASED CARDIAC AND RESPIRATORY SYMPTOMS