bacterial
advertisement

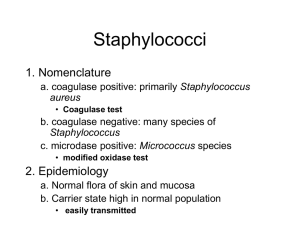
Bacterial infections Bacterial Skin Infections Pyodermas Soft tissue infections Superficial Pyodermas Pus forming condition of skin Causative organism: Staphylococcus aureus Group A ß haemolytic streptococci (GAS) Primary Primary pyoderma is often idiopathic in nature (occurring without any predisposing cause), and may be a result of suppressed or compromised immune status. Secondary Secondary occurs in pre-existing skin conditions such as eczemas, viral infections, scabies, etc. Impetigo Superficial epidermal infection Commonly seen in children Staphylococcus aureus, GAS Warmth, humidity, poor hygiene, Atopic dermatitis, diabetes mellitus Variable pruritus, fever uncommonly Clinical types: Impetigo Contagiosa, Bullous Impetigo Impetigo Contagiosa Non Bullous impetigo Small vesicles quickly become pustules Erosions with yellow brown crust Scattered, discrete, may become confluent Sites : face, arms, legs Bullous Impetigo Bullous Impetigo Vesicles / Bullae having turbid fluid Hypopyon sign No surrounding erythema Moist erosions Distribution Face, legs, arms Differential Diagnosis a) Erosion:dermatitis, scabies b) Bulla: Herpes zoster, bullous pemphigoid dermatitis herpetiformis, burns Ecthyma Develops in neglected lesions e.g. trauma in diabetes mellitus Pain, tenderness Deep, crusted lesions - ulcerates Tenderness, induration Sites: legs & buttocks Lymphadenopathy Heals with scars Impetigo and Ecthyma Diagnosis Mostly clinical; Gram’s stain, culture Treatment General – antiseptic baths Topical: Antibacterials such as mupirocin Oral: GAS – erythromycin, cephalexin S. aureus – cephalexin, amoxycillin – clavulinic acid MRSA - ciprofloxacin, trimethoprim sulphamethoxazole Infectious folliculitis Infection of upper portion of hair follicle Mostly Staphylococcus aureus Predisposing factors: Shaving hairy areas, extraction of hair, occlusion, high temperature, humidity, diabetes mellitus Progresses within days and extends upto months Pruritic, mild pain Lymphadenopathy rarely seen Grouped papules/pustules confined to ostium of hair follicle Minimal scarring, post inflammatory pigmentation seen Infectious folliculitis Face - coexist with acne Beard - Sycosis barbae Neck - Keloidal folliculitis Legs - involvement common in India Trunk - Hot tub folliculitis, Pityrosporum folliculitis Folliculitis - face Superficial folliculitis with thin walled pustules at follicular orifice Can present on scalp and face, especially seen at perioral areas May arise at sites of trauma Develops in crops and heals within few days Most frequent cause Staphylococcus aureus Sycosis barbae Chronic, follicular, perifollicular, pustular, staphylococcal infection of the beard area Develops as erythema, itching near upper lip or nose Pin head sized pustules may develop, pierced by hair Differential diagnosis: Dermatophytic infection, acne vulgaris, herpetic sycosis Keloidal folliculitis Keloid like papules and plaques on the occipital scalp and the back of the neck Starts as chronic folliculitis and perifolliculitis Heals with keloidal scars, sometimes with discharging sinuses Painful and cosmetically disfiguring Treatment : with topical antibacterials, Intralesional Steroids, Prevention of trauma Chronic folliculitis DCPA (Dermatitis cruris pustulosa et atrophicians) Chronic folliculitis seen especially in young Indian males Involves anterior aspect of lower legs bilaterally; may extend upto the thigh Recalcitrant, lasting for several years Usually clears after development of atrophy Differential diagnosis of folliculitis Fungal Pityrosporum folliculitis Tinea capitis Tinea barbae Viral Herpes simplex Molluscum contagiosum Syphilitic Secondary syphillis Infestation Demodicidosis Acneiform eruptions Management: Folliculitis Diagnosis - Gram’s stain -KOH mount - Culture Management - Prevention - Antibiotics Topical – Mupirocin, Clindamycin Oral as per culture and sensitivity studies Abscess, Furuncle and Carbuncle Staphylococcus aureus Predisposing factors - Chronic carrier states - Diabetes Mellitus - Obesity - Poor hygiene - Bactericidal defects (e.g. chronic granulomatous disease) - Hyper - IgE syndrome Abscess, Furuncle and Carbuncle Abscess is circumscribed collection of pus Furuncle is an acute deep necrotising infection of a hair follicle and perifollicular area Carbuncle is a deep infection involving multiple contiguous hair follicles Clinical Presentation Abscess Erythematous, warm, painful/tender Arises in the dermis, subcutaneous fat or muscle Tender nodule; central pus collection Furuncle Arise in hair bearing area Firm tender nodule Central necrotic plug Usually follow staphylococcal folliculitis Abscess formation below necrotic plug Clinical Presentation Carbuncle Evolution similar to furuncle Deep infection of a group of contiguous follicles with Staphylococcus aureus Sieve like openings draining pus Management Grams’ stain and culture Treatment Incision and drainage Systemic antibiotics Recurrent furunculosis Due to persistent S. aureus Proper cleansing measures Nasal, inguinal, axillary and perianal mupirocin Rifampicin 600 mg PO for 7 - 10 days for MRSA Erysipelas and Cellulitis Soft tissue infections – Acute, diffuse, edematous inflammation of dermis and subcutaneous tissue. Erysipelas – Superficial soft tissue infection of dermis & upper subcutaneous tissue. Raised plaque with sharp margins. Cellulitis – Inflammation of subcutaneous tissue. Not raised and no clear margins. Erysipelas and Cellulitis GAS (erysipelas) or S. Aureus Arises via a portal of entry in skin or mucous membrane Fever with chills, malaise, local pain and tenderness May become necrotising Clinical Presentation Red, hot, edematous shiny plaque Well demarcated border in erysipelas Vesicles, bullae, erosions, abscesses and necrosis Breaks in skin, chronic dermatitis Risk factors Diabetes Immunodeficiency Drug and alcohol abuse Cancer and chemotherapy Chronic lymphedema Cirrhosis Neutropenia Renal failure Systemic atherosclerosis Management Diagnosis Gram’s stain and culture Rule out systemic involvement by blood tests and imaging Prognosis Favorable if treatment started early Hematological and lymphatic dissemination if treatment delayed Treatment Supportive: rest, leg elevation, analgesia Appropriate antibiotics Superficial Cutaneous Infections Affect stratum corneum Overgrowth of normal flora Three infections Erythrasma Pitted keratolysis Trichomycosis axillaris Erythrasma Corynebacterium minutissimum Humid climate and occlusion Asymptomatic; occasional pruritus Sharply marginated reddish brown patch/macules Groin fold, axillae, intergluteal & submammary folds Wood’s lamp: coral red fluorescence Treatment: Erythromycin, oral and topical if extensive lesions. Topically azole antifungal agents-clotrimazole & miconazole for 2 weeks Pitted Keratolysis Micrococcus sedentarius Hyperhidrosis of feet; occlusive footwear Asymptomatic, foot odour, itching Discrete / confluent pits in toe webs or on heels Treatment: Reduce moisture, absorbing powders, erythromycin oral/topical, benzoyl peroxide Trichomycosis Axillaris Aerobic Corynebacteria Adherent brown black, yellow, red concretions on hair shaft which can be hard, soft, nodular/more diffuse Axillae and pubic areas Underlying skin normal Treatment: Shaving/ clipping/ topical antimicrobials Other Bacterial Infections Paronychia Periporitis Staphylococcal scalded skin syndrome Toxic shock syndrome Scarlet fever Paronychia Acute infection of the nail fold Facilitated by cuticular damage. Clinically manifested as painful swelling of the proximal/ lateral nail fold Bacterial Culture and sensitivity helps in diagnosis Differential diagnosis: Herpetic whitlow, fungal paronychia Treatment involves incision and drainage; systemic and topical antibiotics Periporitis Pustular lesion, mostly in children during summers, due to staphylococcal infection of sweat gland Sites: face, buttocks, upper trunk, scalp May progress to sweat gland abscess Clinically present as erythematous deep seated nodules. May localize and rupture, leaving behind scar Differential diagnosis: Furuncles, Miliaria pustulosa Treatment : topical &/or oral antibiotics. Prevention: minimizing sweat retention in the affected area Staphylococcal Scalded Skin Syndrome Generalized, confluent, superficially exfoliative disease Mostly occurs in neonates and young children. Due to action of exfoliative exotoxins type A and B liberated by staphylococcus aureus. Fever, skin tenderness and erythema involving the neck, groins and axillae followed by generalized desquamation. Diagnosis by histopathology, immunofluorescence and frozen section of peeled skin. Treatment: Immediate institution of appropriate antibiotic therapy such as methicillin, erythromycin. Toxic Shock Syndrome Acute febrile multisystem disease Mediated by one or more toxins elaborated by staphylococcus aureus Occurs due to infections in wounds, catheters, nasal packs Diagnosis: primarily clinical, supported by the confirmation of staphylococcal infection Treatment: systemic antibiotics; Intensive supportive treatment Scarlet Fever Streptococcal pharyngitis, tonsilliits or cellulitis causing diffuse erythematous exanthem because of pyrogenic exotoxin. Manifested as red tonsils, strawberry tongue, diffuse erythema, Pastia’s lines, circumoral pallor with facial flushing. ASO titre may be diagnostic Treatment: systemic antibiotics Secondary Pyodermas Secondary bacterial infections in pre-existing dermatological conditions May complicate conditions such as scabies, pediculosis, atopic dermatitis and neurodermatitis Treatment: appropriate oral and/or topical antibiotics; treat pre-existing disease Management of Pyodermas: General Principles Identify, Assess and Treat Predisposing factors: Poor hygiene, Malnutrition, Recurrent trauma, Diabetes mellitus, Pre existing skin diseases , Congenital and acquired Immunodeficiency Investigations:(recalcitrant and recurrent infections) For the identification of predisposing factors Smear, Culture and Antibiotic Sensitivity test (SCABS). Management of Pyodermas: General Principles Topical Therapy: Soaks /compresses: Condy’s solution (KMNO4), Burrow’s solution (aluminum chlorohydrate) Topical Antiseptics: Chlorhexidine, Povidine iodine. Topical antibiotics : Mupirocin, Framycetin, Sisomicin, Nadifloxacin, Neomycin, Gentamicin Polymyxin B, Bacitracin, Fusidic acid. Systemic therapy : Semi synthetic penicillins, Cephalosporins, Macrolides, Tetracyclines, Quinolones. Thank you