Chronic Pericarditis
advertisement

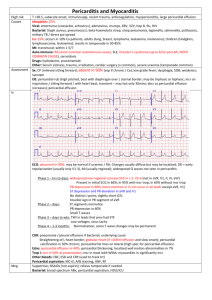
CHRONIC PERICARDITIS… A Rheumatologist’s Perspective Steven S. Overman, MD, MPH, FACR The Seattle Arthritis Clinic Clinical Professor of Medicine University of Washington, Seattle, Washington USA CHRONIC PERICARDITIS A ‘Window’ to Chronic Arthritis • The pericardial tissue that covers the heart is similar to the synovial tissue that lines the joints. • The diagnostic and treatment principles for pericarditis are the same as those for chronic arthritis. • This means that a physician who specializes in chronic arthritis may be able to help your chronic pericarditis patients. My Background • Private rheumatology practice for over 25 years • Masters Degree in Public Health • Robert Wood Johnson Clinical Scholar • Board Certified: Rheumatology, Internal Medicine, & Quality Assurance • Medical Directorships • Clinical Investigator • American College of Rheumatology committees and strategic planning Clinical Professor of Medicine University of Washington, Seattle 5 Principles of Rheumatology Diagnosis & Chronic Pericarditis 1) Search for infections 2) Understand how rheumatology tests can be useful (or misleading!) 3) Re-examine for rheumaticdisease signs 4) Search for organ problems 5) Treat and then re-evaluate Sandra’s Pericarditis • Sandra, age 49, developed a sore throat and cough after noticing an unusual smell coming from her home’s heating vents. • Three weeks later, she presented with syncope and right-sided CHF. Sandra’s Pericarditis HOSPITAL • Pericardial effusion and tamponade diagnosed with echocardiography • Pericardial window placed • Cultures and tissue samples were culture (-) • Troponins suggested myocardial damage RHEUMATOLOGY TESTS • ANA, RF were negative • A family history of rheumatoid arthritis and rheumatic fever was noted Sandra’s Pericarditis Outpatient • Initially improved with colchicine and tapering prednisone 8 • • • weeks Major flare with a 15x increase in C-reactive protein Legionella IgM antibody found positive Spondylitis was diagnosed based on X-ray diagnosis of sacroiliitis and a (+) HLA-B27 12 months • Recurrent flares of “reactive pericarditis” were treated with typical anti-rheumatic drugs methotrexate, tapering prednisone, and biologic therapies. Sandra has improved. MILD Acute Pericarditis • No hemodynamic problems • No fever • Not immunosuppressed • Responds to aspirin or NSAIDs and colchicine SEVERE Acute Pericarditis • Fever >38 C • Follows trauma or myocardial infarcts • Cardiac tamponade • Does not respond to first-line therapy Pericarditis Differential Diagnosis • Infections tuberculosis, malaria, bacterial, atypical bacterial, viral, spirocheaeteal, fungal, helminthes infections • Inflammatory • Neoplastic • Myocarditis or post-myocardial infarct • Metabolic • Traumatic • Radiation 5 Principles of Rheumatology Diagnosis & Chronic Pericarditis 1)SEARCH FOR INFECTIONS • Routine blood and pericardial fluid examinations • Adenosine deaminase <40 means no TB 97% of the time • Serologies check for infections not easily cultured Diagnosing Active Tuberculosis NEWEST TEST GeneXpert is the newest gene array identification technology that can identify the tuberculosis bacillus from body fluid in 2 hours. This test can simultaneously identify TB and resistance to rifampicin. Sandra’s Infection • Legionnaire’s disease – Acute respiratory illness after heating system smell. The organism is found in heating, cooling, and humidifying systems in communities and hospitals. – Pericardial fluid culture (-) Myocarditis with pericarditis is the most common extrapulmonary manifestation (30%). – IgM Legionnella Ab positive proved the diagnosis. 5 Principles of Rheumatology Diagnosis & Chronic Pericarditis 1) Search for infections 2) UNDERSTAND HOW RHEUMATOLOGY TESTS CAN BE USEFUL (OR MISLEADING!) Common Inflammation Markers • C-reactive protein and sedimentation rate are often - but not always increased in rheumatic syndromes. • Unfortunately, they are still non-specific and are increased in infections. Auto-antibody Patterns in Inflammatory Rheumatic Diseases • SERO-POSITIVE means an auto-antibody is positive – Rheumatoid Factor (RF) – Anti-cyclic citrullinated peptide (anti-CCP) – Antinuclear Antibody (ANA) – Anti-double stranded DNA (anti-dsDNA) – Extractable Nuclear Antibody (ENA), SSA, SSB, Scl-70, RNP, Sm, and others – Anti-neutrophil cytoplasmic antibody (pANCA/cANCA) • SERO-NEGATIVE means ALL auto-antibodies are negative Sandra’s Post-infectious, Sero-negative Inflammatory Reaction • INITIAL: Legionella myocarditis and pericarditis • BUT, LATER: reactive pericarditis “skyrocketed” her CRP, although all autoantibodies were negative. 5 Principles of Rheumatology Diagnosis & Chronic Pericarditis 1) Search for infections 2) Understand how rheumatology tests can be useful (or misleading!) 3) Re-examine for rheumatic-disease signs Sero-negative SYSTEMIC LUPUS ERYTHEMATOSIS • • • • • • • • • • Malar rash Discoid rash Photosensitivity Oral ulcers Arthritis Pleuritis or pericarditis Renal disorder Seizures or psychosis Hematologic disorder Anti-dsDNA, anti-Sm, or anti-phospholipid Ab • Antinuclear antibodies Sero-negative MEDIUM VESSEL VASCULITIS • Polyarteritis nodosa • Behcet’s syndrome • Churg-Strauss syndrome Sero-negative RHEUMATOID ARTHRITIS • Rheumatoid nodules • Pericarditis • Premature cardiovascular mortality • Vasculitis • Lung disease Sero-negative RHEUMATIC FEVER • Erythema marginatum • Subcutaneous nodules • Migratory arthritis • Carditis and valvulitis • Central nervous system involvement Sero-negative ADULT STILL’S DISEASE • Arthralgias or arthritis • Nonpruritic, ‘salmon’ colored, maculopapular rash • Lymphadenopathy • Hepatomegaly or splenomegaly • • • • Leukocytosis Sore throat Abnormal liver function Negative tests for antinuclear antibody and rheumatoid factor Sero-negative SPONDYLOARTHRITIS SYNDROMES Sandra’s Sacroliitis Sero-negative SPONDYLOARTHRITIS SYNDROMES • Ankylosing spondylitis • Psoriatic spondyloarthritis • Reactive spondyloarthritis • Inflammatory bowel-associated spondyloarthritis • Undifferentiated spondyloarthritis and enthesitis Sero-negative PSORIASIS ARTHRITIS DIP Swelling, but not osteoarthritis Sero-negative PSORIASIS nail-bed pitting Sero-negative PSORIASIS Onycholysis Sero-negative REACTIVE ARTHRITIS keratoderma blennorrhagicum Sero-negative REACTIVE ARTHRITIS dactylitis and keratoderma 5 Principles of Rheumatology Diagnosis & Chronic Pericarditis 1) Search for infections 2) Understand how rheumatology tests can be useful (or misleading!) 3) Re-examine for rheumatic-disease signs 4) SEARCH FOR ORGAN PROBLEMS SEARCH FOR ORGAN PROBLEMS Sandra’s evaluation • Heart • Lungs • Gastrointestinal • Endocrine • Renal • Liver • Eyes and Brain • Large vessels • Joints 5 Principles of Rheumatology Diagnosis & Chronic Pericarditis 1) Search for infections 2) Understand how rheumatology blood tests can be useful (or misleading!) 3) Re-examine for rheumaticdisease signs 4) Search for organ problems 5) TREAT & RE-EVALUATE Chronic Pericarditis Treatments are the same as Chronic Arthritis Treatments • Antibiotics • NSAIDs (ibuprofen; aspirin) and colchicine • Corticosteroids • Disease-modifying drugs • Biologic injects Sandra’s Chronic Pericarditis 5 PRINCIPLES SANDRA’s CARE 1) Search for infections 1) Pericardial fluid cultures were negative, but her serology for Legionella infection was positive. 2) Understand rheumatology tests 2) General inflammation tests became positive, but all auto-antibody tests were negative. 3) Re-examine for rheumatic disease signs 3) She had no new signs, but showed sacroiliitis on X-ray. 4) Search for organ problems 4) Kidney and liver function normalized when the tamponade was relieved. 5) Treat and re-evaluate 5) With treatment for reactive pericarditis and spondyloarthritis, Sandra is improved, but not cured. The Seattle Arthritis Clinic The Pericarditis Charts on My Desk When I Left Seattle… Seattle Arthritis Clinic 18 Chronic Pericarditis Cases • Ages: 16 to 83 years • Gender: 11 women and 7 men • Sero-positive Conditions: 5 Antibodies: Anti-DNA, ANA, RNP, SS-A, SS-B Diagnoses: Systemic Lupus Erythematosis (1) Sjogren’s Syndrome (1) Undifferentiated Connective Tissue Disease (3) • Sero-negative Conditions: 13 Antibodies: ALL NEGATIVE Diagnoses: Reactive Spondyloarthropathy (1) Psoriasis Spondyloarthropathy (2) Undifferentiated Spondyloarthropathy (8) No underlying disease identified (2) Sandra’s ‘Take Home Message’ 1) Infections can trigger reactive inflammatory pericarditis and arthritis. 2) Sero-negative syndromes such as spondyloarthritis are very common. 3) The 5 Principles of Rheumatology Diagnosis will help you rule out infections, and identify the patterns of rheumatic disease. THANK YOU University of Washington and Northwest Medical Center