HPI
advertisement

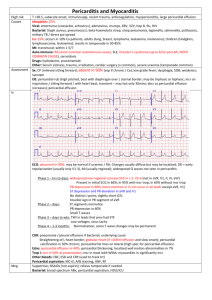
HPI • A 35 yo female presents to the ED with chest pain that started this morning. She had coldlike symptoms earlier in the week. She has an important presentation at work this afternoon about her recent meeting with investors in Japan and wants to know how long it is going to take to find out what is wrong. • What else would you like to ask? HPI • • • • • • • • • • Onset Setting Severity Quality Location, Radiation Duration Frequency Aggravating Factors Alleviating Factors Associated Symptoms HPI • • • • • • • • Onset - Sudden, acute Setting - Started when she woke up this morning Severity - 10/10! Quality - Sharp Location, Radiation - Left-sided, radiating to left shoulder Duration - 2 hours Frequency - No previous episodes Aggravating Factors - Inspiration, lying down, coughing, swallowing • Alleviating Factors - Sitting up and leaning forward • Associated Symptoms - palpitations • What else do you want to know? PMH • Medical Hx: C-section (2009) • Family Hx: non-contributory, no family history of heart disease or bleeding disorders • Social: Married with 2 children, works in finance, one glass of wine per week, denies tobacco and illicit drug use • What is your differential diagnosis? DDx • • • • • • • • Acute MI Pulmonary Embolism Pneumothorax Pneumonia Pericarditis Asthma GERD Anxiety • What do you want to do next? Physical Exam • Vitals: BP 120/80, T 99.0, HR 80, RR 20 • General: Patient is sitting on the edge of the hospital bed leaning forward • HEENT, Abdominal, Neuro, and Psych Exams: wnl • CV: RRR, no murmurs, rub heard at left lower sternal border at the end of expiration • Respiratory: shallow breaths, able to speak in full sentences, lungs clear to auscultation bilaterally • What labs do you want to order and why? Lab Tests • Cardiac Markers – rule out MI • CBC – evaluate for infection, inflammation • Electrolytes – increased risk of arrhythmias in pericarditis • CRP, ESR – evaluate for inflammation • D-dimer – rule out PE (low suspicion) • CXR – evaluate for pneumonia, pneumothorax, PE, effusion • ECG – rule out MI, pericarditis Lab Results • • • • • Troponin I - < 10 μg/L CBC, electrolytes – normal CRP – 16 mg/L ESR – 25 mm/h D-Dimer – 100 ng/mL ECG • What’s your impression of the ECG? • Widespread ST elevation without reciprocal depression • PR depression in lead II Chest X-Ray • Note the cardiomegaly • How can we further evaluate this enlarged heart? Cardiac Echo shows pericardial effusion • RV – right ventricle • LV – left ventricle • LA – left atrium • Ao – aorta • PE – pericardial effusion Chest CT – Thick arrow – pericardial effusion – Thin arrow – pleural effusion Overview of Acute Pericarditis • Inflammation of the pericardial sac accompanied by pericardial effusion “Bread and Butter Heart” Histology of Acute Pericarditis – PMNs adhering to the epicardium Overview of Acute Pericarditis • Many possible causes, including: – – – – – – – – – Idiopathic (usu. post-viral) Infection (viral, bacterial, fungal) Acute MI Dressler’s syndrome SLE Drug-induced (procainamide, hydralazine) Amyloidosis Radiation Post-surgery Hallmarks of Acute Pericarditis • Symptoms: – Chest pain • Pleuritic, associated with breathing • Positional relieved by sitting up and leaning forward – Dyspnea – Palpitations – +/- fever, non-productive cough Hallmarks of Acute Pericarditis • ECG Changes – diffuse ST-segment elevation and PR depression • Physical Exam Findings: – Friction rub – Pulsus paradoxus – Distant Heart Sounds Pericardial Friction Rub • Pathognomonic for acute pericarditis • Heard best at left lower sternal edge with patient sitting up, leaning forward, & exhaling • High-pitched, grating sound with 3 components • http://www.youtube.com/watch?v=J1R8Oxgq hfk Pulsus Paradoxus • > 10 mmHg fall in systolic blood pressure during inspiration • Seen with cardiac tamponade, asthma, pericarditis Treatment • NSAIDs, medium to high doses – 1st line • Corticosteroids – if NSAIDs fail or are contraindicated, recurrent pericarditis • Colchicine – prevents recurrent pericarditis • Pericardiocentesis – for large effusion with hemodynamic compromise, cardiac tamponade, or diagnostic purposes • Pericardiectomy – for persistent constrictive pericarditis Pearls • Acute Pericarditis Key Findings (need 2 of 4 for diagnosis): – Pleuritic chest pain improved by leaning forward – Pericardial friction rub – Widespread ST elevation on ECG – Pericardial effusion Summary • The patient was diagnosed with acute pericarditis and started on NSAID therapy • She continued to be in stable condition and was discharged from the ED with instructions to follow-up with her PCP • She was told to expect her symptoms to resolve in 2 weeks to 3 months