Secondary Amenorrhea
advertisement

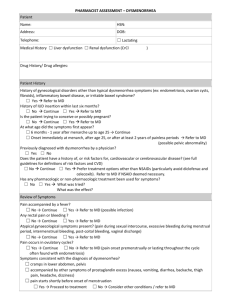
2015 PEDIATRIC BOARD REVIEW COURSE ADOLESCENT MEDICINE WARREN M. SEIGEL M.D., M.B.A., F.A.A.P., F.S.A.H.M. Chairman, Department of Pediatrics Director of Adolescent Medicine Coney Island Hospital Brooklyn, NY Vice-Chair, American Academy of Pediatrics District II – New York CASE #1 Katherine is a 14 year old female who presents for a routine examination for sports. She has no complaints. Her past medical history and family history are unremarkable. On physical examination, you note that she has Tanner 3 breasts and pubic hair. Which of these would indicate sexual maturity rating (Tanner) stage 3 development in a female? 1. 2. 3. 4. 5. 40% Fine hair on the upper lip Acne Darkly pigmented, slightly curly pubic hair Breast and papilla elevated as a small mound Menstruation 40% 20% 0% 1 0% 2 3 4 5 PUBERTY Physical changes associated with development Sequence of change is similar for all adolescents Variations in tempo and timing are common Physical changes reflect underlying hormonal changes SEQUENCE OF PUBERTY GIRLS Breast Buds Pubic Hair Appears Growth Spurt Axillary Hair Pubic Hair Matures Breasts Mature Menarche (First Period) Adult Height BOYS Testicular enlargement Growth of penis/scrotum Appearance of pubic hair Axillary Hair First ejaculations Growth spurt Facial hair Adult Height Features of Female Development Onset: Growth spurt: Height Achieved: Menarche: Acne: 10 years (8-13) Tanner 2 - 3 4 inches/year 12 years common at Tanner 3 - 4 A 13 year old boy is seen in your office because of breast enlargement over the past 6 months. He denies pain, galactorrhea and marijuana use. He is taking no medications. Physical examination reveals sexual maturity rating (Tanner) stage 2 genitalia and pubic hair growth and asymmetric breast buds beneath each nipple, with the left measuring 1 cm and the right 3 cm. Of the following, the most appropriate INITIAL management for this boy is: 1. Head CT with contrast 2. MRI of the abdomen 3. Serum beta-human chorionic gonadotropin level 4. Reassurance that this is a normal occurrence 5. Ultrasonography of the testes 0% 1 0% 0% 2 3 0% 0% 4 5 Features of Male Puberty Onset: Peak Height Velocity: First Ejaculations: Average Height Gained: Strength Peak: 9-13 years (average = 12) Tanner 3 - 4 Tanner 3 5-7 inches/year Tanner 4 – 5 Gynecomastia occurs in approximately 60% CASE #1 (continued) Later in the course of your history, you find out that Katherine has tried tobacco, drinks alcohol “on weekends with my friends” and “smokes weed once in a blue”. Adolescence is best described as the period: 1. Immediately before, during, and after puberty 2. Of physiologic adjustment to maturity 3. Of psychosocial transition from childhood to adulthood 4. Of maximal physical growth 5. Of maximal sexual development 0% 1 0% 0% 2 3 0% 0% 4 5 FEATURES OF EARLY ADOLESCENCE (Am I Normal?) Physical Changes and Concerns Sense of Being “Center Stage” Sense of Invulnerability Wide Mood Swings Rejection of Childhood Things Beginnings of Emancipation Non-Parent Adult Role Models Same-Sex Friendships Concrete Thinking FEATURES OF MIDDLE ADOLESCENCE (Am I Liked?) Puberty (Almost) Complete Testing/Showing Off “New Body” Independence-Dependence Conflicts Strong Peer Attachments Concern With Sexual Appeal Experimentation/Risk-Taking Abstract Thinking Begins FEATURES OF LATE ADOLESCENCE (Am I Loved?) Definition of Adult Role in Society Definition of Adult Role in Family Mainly Independent Decisions, Actions Established, Realistic, Self-Identity Realization of Vulnerability, Limitations Abstract Thinking Well Established High Risk Behaviors Alcohol 66% acknowledge use Cocaine Tobacco 41% acknowledge use 23% currently smoking Inhalants 41% acknowledge use 16% currently smoking Marijuana 5.5% acknowledge use 3% currently use 9% acknowledge use Prescription Drugs 18% acknowledge use CASE # 2 Jonathon is a 16 year old male who comes to your office complaining of a clear urethral discharge and burning on urination for the past 1 week. He admits to being sexually active, the last time being 10 days ago. The MOST prevalent sexually transmitted infection (STI) among adolescents and young adults in the US is: 3. Chlamydia Genital herpes Gonorrhea 4. HPV 5. Syphilis 1. 2. 0% 1 0% 0% 2 3 0% 0% 4 5 6 CHLAMYDIA TRACHOMATIS MALES FEMALES Asymptomatic Asymptomatic Urethritis Cervicitis Epididymitis CHLAMYDIA: SIGNS AND SYMPTOMS MALE: FEMALE: Burning, Urethral Discharge, Pain in Epididymis Vaginal/Cervical Discharge, Pelvic Pain, Painful Intercourse, Burning MAY BE NO SYMPTOMS IN MALE OR FEMALE. CHLAMYDIA TRACHOMATIS DIAGNOSIS Culture: “gold standard” Leukocyte esterase; urine dip in males Enzyme linked assay (EIA or ELISA) Direct Fluorescent Antibody (DFA) DNA probes Nucleic Acid Amplification Tests (NAATs) CHLAMYDIA TRACHOMATIS TREATMENT Azithromycin 1 gm single dose by mouth Doxycycline 100 mg by mouth twice daily for 7 days PARTNER TREATMENT!!! Follow-up “Test of Cure” recommended An 18 year old girl complaining of heavy menstrual periods that last 8-10 days. Physical examination reveals a creamy, greenish vaginal and cervical discharge that contains many leukocytes and Gram negative diplococci in pairs. A pregnancy test is negative and syphilis serology is pending. Of the following, the BEST antibiotic therapy for this patient is: 1. 2. 3. 4. 5. Amoxicillin Amoxicillin and Erythromycin Ceftriaxone Ceftriaxone and Azithromycin Spectinomycin and Doxycycline 0% 1 0% 0% 2 3 0% 0% 4 5 6 GONORRHEA: SIGNS AND SYMPTOMS MALE: FEMALE: Yellow “Drip” from Penis, Burning, Pain in Epididymis Vaginal/Cervical discharge, Heavy Menses, Painful Intercourse, Burning, Frequency MAY BE NO SYMPTOMS IN MALE OR FEMALE Neisseria Gonorrhea MALE Urethritis Epididymitis FEMALES Asymptomatic Cervicitis Bartholin’s gland abscess Pelvic Inflammatory Disease (PID) NEISSERIA GONORRHEA DIAGNOSIS Culture: “Gold Standard” Leukocyte esterase suggestive in males DNA probes, PCR, EIA are all available Nucleic Acid Amplification Tests (NAATs) NEISSERIA GONORRHEA TREATMENT Ceftriaxone Cefixime Ofloxacin Ciprofloxacin 250 mg IM in single dose 400 mg PO in single dose 400 mg PO in single dose 500 mg PO in single dose ADDITIONAL TREAMENT FOR CHLAMYDIA TRACHOMATIS IS TYPICAL SYPHILIS: SITE OF INFECTION MALE: FEMALE: INFANT: Penis, Anus, Mouth, Lips Vulva, Vagina, Cervix, Anus, Mouth, Lips Acquired During Pregnancy, Birth Defects, Death Spread to entire body in male and female including heart and brain! SYPHILIS: SIGNS AND SYMPTOMS PRIMARY SYPHILIS Chancre on sex organs Painless indurated ulcer with smooth border Incubation = 3 weeks, healing = 6 weeks SECONDARY SYPHILIS Fever, rashes, generalized illness TERTIARY SYPHILIS Infection of brain, blood vessels SECONDARY SYPHILIS CONSTITUTIONAL SYMPTOMS Fever, malaise, adenopathy, musculoskeletal symptoms SKIN AND MUCOUS MEMBRANE FINDINGS Rash – begins on trunk Rash – involves palms and soles Condyloma lata – moist plaques Alopecia SKIN LESIONS ARE HIGHLY INFECTIOUS! Diagnosis – Syphilis Serologic – nontreponemal RPR, VDRL, ART Serologic – treponemal FTA-ABS, MHATP,TPHA Treatment – Syphilis Less than 1 year duration – Benzathine Penicillin-G 2.4 million units IM Greater than 1 year duration – Benzathine Penicillin-G 7.2 million units, 3 divided doses A 16 year old girl has had dysuria and a vaginal discharge for 2 weeks. Findings on pelvic examination include a frothy vaginal discharge and cervical petechiae. Microscopic examination of the discharge reveals flagellated organisms. Results of a urinalyis are normal. Among the following, the BEST treatment for this patient’s problem is: 1. 2. 3. 4. 5. Azithromycin Cefixime Ciprofloxacin Doxycycline Metronidazole 0% 1 0% 0% 2 3 0% 4 0% 5 6 Trichomonas Males Generally asymptomatic Females Malodorous vaginal discharge Cervicitis Vulvitis with labial edema Trichomonas Diagnosis Observation of flagellate on saline wet mount Treatment Metronidazole 2 gm po x 1 dose Bacterial Vaginosis Non-gonococcal Non-chlamydial Non-trichomonal Non-candidal Due to Gardnerella vaginalis Bacterial Vaginosis Symptoms Vaginal discharge- grey-white, thin , watery Pruritis and itching may accompany Worsens with intercourse Malodorous Diagnosis Saline wet prep with “clue” cells Treatment Metronidazole 500mg PO bid x 7 days Genital Herpes: Site of Infection Males: Blisters on Penis, Scrotum, Buttocks Females: Blisters on Vulva, Vagina, Cervix, Buttocks Infants: Systemic Genital Herpes: Signs and Symptoms Primary Infection: Very Painful Painful Urination 1-3 weeks Repeat Infections: Less Painful 1 Week or less Herpes Simplex - HSV Skin lesions appear at site within 2-14 days Grouped papules on erythematous base Ulceration Erosion Very painful Constitutional symptoms Genital Herpes: Treatment Treat Virus Treat Symptoms No sex until 1 week after blisters heal Treat partner only if infected Treatment: Genital Herpes Primary Recurrent A) ACV 400 mg PO BID B) ACV 200 mg po 2-5 times/day Severe disease Acyclovir 400 mg oral bid Suppressive Therapy Acyclovir 400 mg oral tid X 5 days Prophylaxis Acyclovir 400 mg oral tid X 7-10 days ACV 5 -10 mg/kg IV every 8 hours X 5-7 days No role for topical ACV Human Papilloma Virus Most common STI Increasing prevalence among teens Associated with majority of Pap smear abnormalities Treatment Podophyllin Cryotherapy with liquid nitrogen Podofilox (home treatment) CASE # 3 Over the past 6 months, Marianne, a 15 year old girl in your practice, has missed 8 days of school because of severe, episodic lower abdominal pain that coincides with menses. Menarche was at age 13 and menses are regular. She states that she is not sexually active. Findings on physical exam are normal. Of the following, the BEST treatment for this girl’s abdominal pain is: 1. 2. 3. 4. 5. Abdominal exercises Acetaminophen Hydrochlorothiazide Low-salt diet Naproxen 0% 1 0% 0% 2 3 0% 0% 4 5 6 Normal Menstruation Normal menstruation is an indication that the hypothalamic--pituitary--ovarian-uterine axis is intact and responsive. Physiology of Menses FSH - stimulates the maturation of ovarian follicles - directs the conversion of androgens in the granulosa cells of the ovary to estrogens LH - stimulates theca cells of the ovary to produce androgens - midcycle LH surge stimulates ovulation Physiology of Menses Estrogens- stimulate the proliferation of endometrial epithelial and stromal cells. Stimulate glandular formation. Progesterone- produced by corpus luteum, causes the endometrium to function in a secretory manner, leading to increased blood vessel growth and tortuosity. Normal Menstrual Cycles Follicular Phase Ovulatory Phase Luteal Phase Follicular Phase Endometrial proliferation under estrogen influence Endometrial stroma becomes compact Estrogen triggers midcycle LH surge Cervical mucus is watery Ovulatory Phase Following ovulation, corpus luteum produces both Estrogen and Progesterone. Progesterone exerts suppressive effect on Estrogen resulting in the conversion of the endometrium to a secretory state. Ovulatory Phase Vaginal secretions and Cervical mucus are copious and clear. Secretions placed on glass slide will demonstrate “ferning” pattern when allowed to dry. (know this !) Case # 3 (continued) Upon further questioning, Marianne admits that her last menstrual period was approximately 8 weeks ago. She is sexually active with a single male partner and does not use condoms consistently. Menstrual Abnormalities Primary Amenorrhea Secondary Amenorrhea Dysmenorrhea Dysfunctional Uterine Bleeding Polycystic Ovary Disease Amenorrhea Definition: Amenorrhea is the absence of menses. Amenorrhea Secondary Amenorrhea: Primary Amenorrhea: The lack of menses Absence of menses by age 14 with the for a period of at least absence of 3 cycle lengths or for secondary sexual a period of 6 months characteristics. The lack of menses by age 16 regardless of the status of secondary sexual characteristics. Primary Amenorrhea Differential Diagnosis Hypothalamus Pituitary Ovary Uterus & Outflow Tract Primary Amenorrhea Hypothalamic Causes Physiologic delay – often familial Systemic disease – often chronic Stress Athletics Eating Disorders Obesity Drugs Cytoxin, Phenothiazines, Isotretinoin, Amphetamines Steroids, Opiates Primary Amenorrhea Pituitary Causes Idiopathic Hypopituitarism Tumor Hemochromatosis Primary Amenorrhea Thyroid & Adrenal Gland Causes Hypothyroidism Hyperthyroidism Congenital Adrenal Hyperplasia Tumor Gonadal Causes Turner Syndrome and Mosaicism Pure Gonadal Dysgenesis Testicular Feminization Syndrome Hermaphroditism Ovarian Failure Primary Amenorrhea Uterus and Outflow Tract Causes Synechiae Pregnancy Agenesis Imperforate Hymen A 15 year old girl has reached Tanner Stage 4. She has had periodic abdominal discomfort but has never menstruated. Physical examination reveals a midline abdominal mass. Pregnancy test is negative. On genital examination, you are MOST likely to see: 1. A bluish, bulging hymen 2. A hymenal opening of about 1 cm An annular hymenal membrane Labial adhesions obscuring the hymen Vaginal discharge and labial irritation 3. 4. 5. 0% 1 0% 0% 2 3 0% 0% 4 5 6 Evaluation of Primary Amenorrhea History Physical Examination Pelvic Examination Ultrasound if needed to define anatomy FSH, LH, Prolactin, Testosterone Bone Age Karyotype Secondary Amenorrhea Think Pregnancy Pregnancy Pregnancy Secondary Amenorrhea Hypothalamic Causes Stress Athletics Eating Disorders Obesity Drugs Cytoxin, Phenothiazines, Isotretinoin, Amphetamines Steroids, Opiates Systemic Enteritis, colitis Diabetes CF, renal disease Secondary Amenorrhea Pituitary Causes Hyperprolactinemia Pituitary Adenoma Post-Oral Contraception Thyroid Causes Hyperthyroidism Hypothyroidism Secondary Amenorrhea Adrenal Causes Congenital Adrenal Hyperplasia Adrenal Tumor Gonadal Causes Polycystic Ovary Syndrome Gonadal Dysgenesis Ovarian Failure Secondary Amenorrhea Uterus and Outflow Tract Causes Asherman Syndrome scarring from D&C Tumor Evaluation of Secondary Amenorrhea Complete History & Physical Exam Pelvic Examination Pregnancy Test Evaluation of Secondary Amenorrhea Pregnancy Test NEGATIVE: Provera, 10 mg BID X 5 days Withdrawal bleed indicates: Ovaries produce adequate estrogen to stimulate endometrial proliferation in the uterus. Also indicates that the outflow tract is intact and functioning normally. Evaluation of Secondary Amenorrhea Lab Evaluation: CBC with diff, ESR UA FSH, LH, prolactin Radiologic Evaluation: pelvic ultrasound Dysmenorrhea Definition – pain associated with menses Etiology: Prostaglandin PGE2 and PGF2 implicated Endometriosis Onset within 6-12 months following Menarche Dysmenorrhea Lower abdominal to back/thigh pain reported Polyps, benign tumors Infection Dysmenorrhea Differential Diagnosis Endometriosis Pelvic Inflammatory Disease Benign Tumor Anatomic abnormality Workup for Dysmenorrhea Complete physical examination including pelvic exam CBC with differential, ESR/CRP GC/chlamydia screen Wet mount of discharge if present Management of Dysmenorrhea Primary Dysmenorrhea (no abnormality on evaluation) Non-steroidal anti-inflammatory agent Reassurance If no improvement with NSAIDS, estrogen/progesterone combination contraceptive Secondary Dysmenorrhea Infection – treat Endometriosis – refer to GYN CASE #4 Adrienne is a 14 year old female who complains of vaginal bleeding for the past month. She states that she has been using approximately 6 – 8 pads per day and that her bleeding has been heavier than usual. Menarche was at 13 years. She denies sexual activity. Which of the following statements is true regarding Dysfunctional Uterine Bleeding (DUB) in the adolescent? 1. It is diagnosed by excluding bleeding of organic cause. 2. If exsanguinating and unresponsive to all other measures, it is better treated by hysterectomy than by irradiation. It can usually be controlled by administration of estrogens and progestigens. It is frequently associated with dysmenorrhea. It occurs as a normal part of adolescent growth and development. 3. 4. 5. 0% 1 0% 0% 2 3 0% 0% 4 5 6 Dysfunctional Uterine Bleeding Polymenorrhea – bleeding which occurs at regular intervals of less than 21 days Menorrhagia – prolonged or excessive bleeding at regular intervals of 21-35 days Metrorrhagia – irregular interval bleeding Dysfunctional Uterine Bleeding Etiology – anovulatory bleeding secondary to immature hypothalamic-pituitaryovarian axis Dysfunctional Uterine Bleeding Differential Diagnosis Anovulatory Bleeding Pregnancy complications Ectopic, spontaneous abortion Endometritis Malignancy Iatrogenic Ovarian Dysfunctional Uterine Bleeding Evaluation Complete History and Physical Exam Menstrual and Sexual History Pregnancy Test CBC with differential Platelet Count PT/PTT Von Willebrand Factor Antigen/Panel, Ristocetin Cofactor Management of Dysfunctional Uterine Bleeding If Hemoglobin is stable Observation and reassurance Begin Iron Therapy Combination estrogen/progestin contraceptive pills Management of Dysfunctional Uterine Bleeding If bleeding is severe, Hemoglobin unstable Estrogen every 4-6 hours until bleeding is stopped Then begin Estrogen and Progesterone containing pills as maintenance daily Polycystic Ovary Disease Anovulatory cycles with irregular bleeding Suspect in the mid adolescent with menstrual irregularity Polycystic Ovary Disease Etiology: Defect in gonadotropin secretion leading to elevated LH. FSH is normal/borderline low. Acyclic estrogen/progesterone secretion Elevated Androgen secretion Anovulation Polycystic Ovary Disease Presentation Amenorrhea Hirsuitism Obesity Infertility Polycystic Ovary Disease Differential Diagnosis Familial Hirsuitism Cushing’s Syndrome Androgen excess Late onset CAH (21-hydroxylase deficiency) Androgen producing tumor Anabolic steroid use Polycystic Ovary Disease Evaluation History including PMH Medication History Menstrual History Sexual History including pregnancy, infection, abortion Physical Exam Obesity Hirsuitism Clitoromegaly Polycystic Ovary Disease Pelvic Examination Size of ovaries Ultrasound Size of Ovaries Laboratory Evaluation LH/FSH, E2, DHEAS, Testosterone, 17-OH Progesterone Polycystic Ovary Disease Treatment Normalization of Menses Estrogen Dominant Oral Contraceptive Pill Hirsuitism Weight Loss Cosmetics Fertility Clomid Metformin CASE #5 Mark is a 15 year old boy who comes to your office for a routine physical examination. His mother asks to meet with you alone and says that a few weeks ago she found a plastic baggy with marijuana under his bed. She requests that you perform a drug test without telling her son. QUESTIONS Will you perform the drug test without telling Mark? If not, what will you tell Mark as an alternative? What will you tell Mark about drug testing? The most commonly abused substance by adolescents is: 1. 2. 3. 4. 5. Marijuana Tobacco Cocaine Alcohol Ecstasy 0% 1 0% 0% 2 3 0% 0% 4 5 6 Substance Abuse Definition: The persistent use of illicit substances despite experiencing negative consequences from their use. Substance abuse is a multi-dimensional disorder with a complex biopsychosocial etiology. Multiple Drug Use Adolescents rarely report a “drug of choice” but rather use multiple substances. Age at First Use The age of first use for US teens is 11-12 years of age. Case #5 (continued) Mark’s grades have been falling and he quit the football team recently. He has a new group of friends that he never brings home. Mark tells you that he occasionally smokes marijuana but he denies using any other drugs. He admits to being sexually active and drinking beer with his friends on weekends. His parents are concerned because they recently smelled alcohol on his breath when he returned from a party. Of the following behaviors, which would be MOST suggestive of a serious problem with substance abuse? 1. 2. 3. 4. 5. Associating with teenagers who use drugs Dropping his grades from A’s to B’s Quitting the football team Sleeping more than 12 hours per night Smoking cigarettes 0% 1 0% 0% 2 3 0% 4 0% 5 6 Risk Factors for Illicit Drug Use Family Tolerance Peer Influences- The most positive predictor of drug and alcohol use among teens, is a positive history of use among peers. Other Factors Early Academic Failure Isolation Criminal Activity Recognizing Substance Abuse Problems Behavioral Change Unexpected Decline in School Performance School Problems & Behavioral Concerns Isolation from peers Outbursts of anger or abusive behavior without remorse Obtaining the History With the teen separated from parent/s With assurance that the substance use history is part of a routine interview (it should be!) With appropriate lead in questions... Many teens your age go to parties where alcohol is available…do you? Have you ever consumed a drink containing alcohol? Have you ever been drunk? The “C.R.A.F.F.T.” C -- Have you ever ridden in a CAR driven by someone (including yourself) who was "high" or had been using alcohol or drugs? R -- Do you ever use alcohol or drugs to RELAX, feel better about yourself, or fit in? A -- Do you ever use alcohol or drugs while you are by yourself, ALONE? F -- Do you ever FORGET things you did while using alcohol or drugs? F -- Do your family or FRIENDS ever tell you that you should cut down on your drinking or drug use? T -- Have you gotten into TROUBLE while you were using alcohol or drugs Drug Screening Ethical Issues- screening without the knowledge and consent will likely have a negative effect on the doctor-patient relationship. The AAP does not endorse such “non-informed” screening. In the habitual user, which of the following substances is MOST likely to be detected by a urine screening test up to 1 month after last use? 1. 2. 3. 4. 5. Alcohol Barbiturate Cocaine Marijuana Phencyclidine 0% 1 0% 0% 2 3 0% 0% 4 5 6 Drug Screening... Obtain the appropriate sample Either urine or serum are adequate for general screening. The use of hair for screening is more sophisticated than generally necessary for routine screening. Drug Screening... How long will drug screening remain positive ? Ethanol 2-14 hours Amphetamines < 48 hours Opiates 2 days Barbiturates 3-4 days Cocaine 2-4 days maximum Cannabinoids 10 - 20 days maximum FIVE STAGES OF SUBSTANCE ABUSE STAGE 1 STAGE 2 STAGE 3 STAGE 4 STAGE 5 CURIOSITY EXPERIMENTATION REGULAR USE PSYCHOLOGIC OR CHEMICAL DEPENDENCY USING DRUGS TO FEEL “NORMAL” CASE #6 Adrienne is a 13 year old female who is brought to you by her mother for a physical examination. She has no complaints and her past medical history is unremarkable. The mother requests that you examine her daughter “to see if she’s a virgin” and if not, the mother requests that you start her on some form of contraception. Adolescent Sexual Behavior 80% of Males and 70% of Females have intercourse before age 20 Average age of first intercourse is 16 Often a series of single partners Considerations in Contraceptive Choice for Adolescents Frequency of intercourse Number of partners Acceptability Motivation and self-discipline Access to medical care Effectiveness Safety vs. Risk Cost Which of the following is a RELATIVE CONTRAINDICATION to prescribing hormonal contraceptives that contain both estrogen and progestin? 1. 2. 3. 4. 5. Diabetes mellitus Fibrocystic breast disease Ovarian cyst Pelvic inflammatory disease Rheumatoid arthritis 0% 1 0% 0% 2 3 0% 0% 4 5 6 Prevention Abstinence Effective No cost Applicable for all Requires willpower for both partners Withdrawal Effective 77-84% No cost Does not prevent STIs Always available Choice of last resort Prevention Fertility Awareness Recognition of fertile and safe times in cycle Effectiveness 76-98% No major health concerns No cost Difficult if irregular cycles Requires discipline in both partners Poor choice for adolescents Condoms Prevent sperm from entering vagina Must be in place prior to contact and during withdrawal Effectiveness 90-98% Over-the-counter Best protection against STIs Requires motivated couple Appropriate for casual sex partner Prevention Diaphragm Barrier to cervix Must be in place prior to sexual contact & 6 hrs after Effective 81-98% Requires physical exam Can be inconvenient Very motivated teen in stable relationship Intrauterine Device (IUD) Prevents implantation Device placed inside uterus Effectiveness 95-98% Requires medical surveillance May be appropriate for adolescents who desire long term contraception Prevention Sponge Disposable barrier to cervix Moistened sponge used similar to Diaphragm Effectiveness 80-91% Over-the-counter Some STI protection Expensive Appropriate for motivated teen Good back-up method Foam & Spermicides Chemical destruction of sperm in vagina Must be in place prior to intercourse Effectiveness 82-97% Over-the-Counter Some STI protection Requires motivated couple Appropriate for motivated adolescents Prevention Sterilization Permanent surgical sterilization 99% Effectiveness Medically performed Not appropriate for adolescents Hormonal Contraceptives Prevents ovulation Effective 98-99% Multiple health benefits Medical complications lowest in adolescents Must be taken daily Minor side effects Often method of choice for adolescents A 14 year old girl who has sickle cell disease wishes to use hormonal contraception. She had a stroke 3 years ago associated with persistent left-sided weakness and a seizure disorder. Menarche occurred at age 12 and menses are irregular. She has been sexually active for 2 years and has had 3 partners. Her current partner occasionally uses condoms. The most important CONTRAINDICATION to the use of hormonal contraceptives in this patient is her history of 4. Epilepsy Inconsistent use of condoms Irregular menstrual bleeding Multiple sexual partners 5. Stroke 1. 2. 3. 0% 1 0% 0% 2 3 0% 0% 4 5 6 Prevention Injectable Hormones Suppresses hormone cycle Injection every 1-3 month 98-99% effective Long lasting, unrelated to intercourse Requires more frequent medical visits Emergency Contraception Prevents implantation Taken post intercourse Effective 99% Emergency method for Rape, Contraceptive Failure Available Over-theCounter for those 17 years of age and older Prevention Contraceptive Patch Delivers continuous systemic doses of hormones Change weekly x 3 weeks then patch-free x 1 week Patch contains 6.00 mg norelgestromin and 0.75 mg ethinyl estradiol Vaginal Ring Progestin: Etonogestrel: 120 µg/day & Estrogen: Ethinyl Estradiol: 15 µg/day Worn for three out of four weeks Self insertion & removal Contraindications for Hormonal Contraception Absolute Past or current history of thromboembolic disorder, cerebrovascular disease, Breast cancer or Estrogen dependent neoplasia Prolonged immobilization Acute liver function impairment Pregnancy Relative Vascular or migraine headaches Collagen vascular diseases Severe hypertension Chronic heart disease Sickle cell disease Severe renal disease Diabetes mellitus