the session PowerPoint
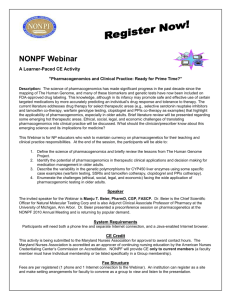
advertisement

Clinical Pharmacogenomics: Implications of New Developments for the NHS Munir Pirmohamed NHS Chair of Pharmacogenetics Department of Molecular and Clinical Pharmacology Institute of Translational Medicine University of Liverpool The Next 20 Years Prediction is very difficult, especially about the future Niels Bohr, Danish Physicist The best way to predict the future is to invent it Alan Kay, American Computer Scientist Definitions Pharmacogenetics (after Vogel, 1957) The study of the genetic basis for the difference between individuals in response to drugs Pharmacogenomics (after Marshall, 1997) 1. Use of population genetic information for drug research, design and development 2. Clinical management of drug therapy (drug dosing and drug choice) Evolution of Clinical Pharmacogenomics Phenotype Individual genes GWAS Sequencing Probe drug PCR-based Increasing use Future? Metabolite: parent drug ratio Current Standard Robust findings Implementation Thiopurine Methyl Transferase (TPMT): A Phenotypic Test Metabolises azathioprine and 6-mercaptopurine Thioguanine accumulation inversely related to TPMT activity Associated with severe haemopoietic toxicity Molecular basis defined Phenotyping assays available and still used PATCHY UPTAKE and dependent of specialty Evolution of Clinical Pharmacogenomics Phenotype Individual genes GWAS Sequencing Probe drug PCR-based Increasing use Future? Metabolite: parent drug ratio Current Standard Robust findings Implementation Technology-Based Reduction in the Burden of ADRs: The Case of Abacavir Hypersensitivity NH N H2N Clinical genotype N N Association with HLA-B*5701 N CH2OH Clinical phenotype Incidence before and after testing for HLA-B*5701 Country Pre testing Post testing Reference Australia 7% <1% Rauch et al, 2006 France 12% 0% Zucman et al, 2007 UK (London) 7.8% 2% Waters et al, 2007 Effect of Pharmacogenetics on Drug Usage 6000 Combivir Kivexa Truvada Trizivir Atripla 700 HLA tests 650 5500 600 550 4500 500 4000 450 3500 400 350 3000 300 2500 250 2000 200 1500 150 1000 100 500 50 0 0 Jul Jun May Apr Mar Feb Jan Dec Nov Oct Sep Aug Jul Jun May Apr Mar Feb Jan Dec Nov Oct Sep Aug Jul Jun May Apr Mar Feb Jan Dec Nov Oct Sep Aug Jul Jun May Apr Mar Feb Jan Dec Nov Oct Sep Aug Jul Jun May Apr Mar Feb Jan 2005 2006 2007 2008 2009 Cumulative number of HLA tests Patient days of treatment 5000 Evolution of Clinical Pharmacogenomics Phenotype Individual genes GWAS Sequencing Probe drug PCR-based Increasing use Future? Metabolite: parent drug ratio Current Standard Robust findings Implementation Evolution of Clinical Pharmacogenomics Phenotype Individual genes GWAS Sequencing Probe drug PCR-based Increasing use Future? Metabolite: parent drug ratio Current Standard Robust findings Implementation Malignant Melanoma and BRAF Inhibitor: Baseline and 2 Weeks After Evidence What type of evidence is required for demonstration of clinical utility? Warfarin Pharmacogenetics: Controversy Regarding Genotyping Change in warfarin label (2007) and dosing tables (2010) Pharmacogenetic-Based Dosing: Warfarin Randomised Controlled Trial FP7 sponsored EU trials 3 trials: warfarin, phenprocoumon, acenocoumarol 400-450 patients in each %TIR as primary outcome measure Point of Care test for genotyping European Union Pharmacogenetics of AntiCoagulant Therapy HLA Genotyping to Prevent Serious Adverse Drug Reactions Since 2001, 22 new alleles associated with serious immunemediated adverse drug reactions have been identified Many of these have been based on genome wide association studies with initial results being replicated Examples include: Carbamazepine: HLA-B*1502 and Stevens-Johnson Syndrome Carbamazepine: HL-A*3101 and hypersensitivity syndrome Allopurinol: HLA-B*5801 and serious cutaneous adverse reactions Flucloxacillin: HLA-B*5701 and cholestatic hepatitis Are we going to require RCTs for all of these association? Can we afford it? “Hierarchies of evidence should be replaced by accepting—indeed embracing—a diversity of approaches..... ...It is a plea to investigators to continue to develop and improve their methods; to decision makers to avoid adopting entrenched positions about the nature of evidence; and for both to accept that the interpretation of evidence requires judgment.” Evidence standards differ between non-genetic and genetic tests 3 examples given: Drug exposure Prevention of adverse drug reactions Health technology assessment Drug Exposure: Differential Evidential Standards Example: Aztreonam SmPC “after an initial usual dose, the dosage of aztreonam should be halved in patients with estimated creatinine clearances between 10 and 30 mL/min/1.73 m2” Many different examples in hepatic and renal impairment with dose instructions based on PK studies and occasionally PK-PD modelling No need for RCTs – in fact, would be impractical However, a genetic polymorphism leading to same degree of change in drug exposure is often ignored and/or RCT data are required for implementation Differential Evidence Standards Unfamiliarity with genetic tests Lack of experience in interpretation Perceived cost of genetic testing Lack of availability of tests Poor turnaround time recommendations on dosing evaluation in patients with polymorphisms in known metabolic pathways The Future? 10 years A whole genome costs less than £100 Only needs to be done once Good visualisation software Patient who requires a drug metabolised by CYP2D6 Absent in 8% of the population Are you going to ignore the genetic data in the patient’s medical record? Patient Empowerment Translation into Clinical Practice Lost in Translation • • • • Major on-ongoing advances Identify evidence needs Consistency in evidence standards Streamlined processes for adoption into NHS • Innovation into practice a major driver for the AHSN Poste, Nature, 2011 Acknowledgements Dept of Pharmacology Ana Alfirevic, Dean Naisbitt, Andrea Jorgensen, Dan Carr, Mas Chaponda, Fabio Miyajima, Kevin Park plus many others Collaborators • Wellcome Trust Sanger Institute (Panos Deloukas, Stephane Bourgeois, Trevor Lawley, Gordon Dougan) • University of Bangor (Dyfrig Hughes) • Epigen, DILIGEN, iSAEC Funders • Department of Health (NHS Chair of Pharmacogenetics), NIHR programme, MRC, EU-FP7, Wellcome Trust