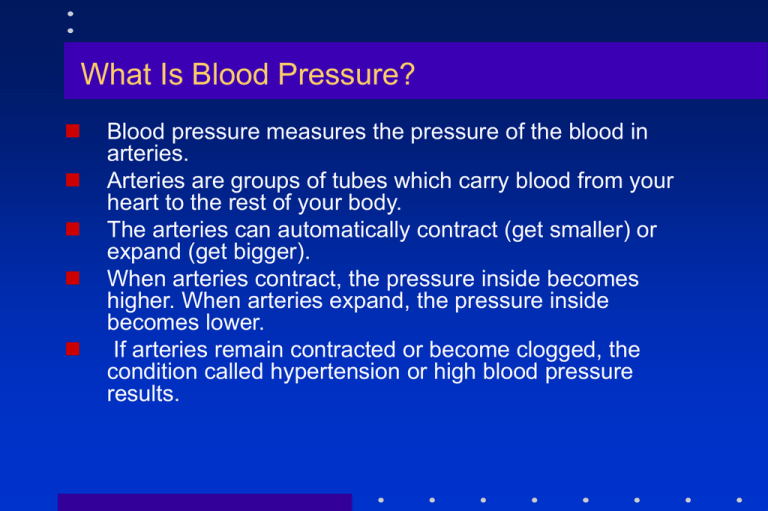
What Is Blood Pressure?
Blood pressure measures the pressure of the blood in
arteries.
Arteries are groups of tubes which carry blood from your
heart to the rest of your body.
The arteries can automatically contract (get smaller) or
expand (get bigger).
When arteries contract, the pressure inside becomes
higher. When arteries expand, the pressure inside
becomes lower.
If arteries remain contracted or become clogged, the
condition called hypertension or high blood pressure
results.
How Is Blood Pressure Measured?
A blood pressure reading consists of two
numbers: systolic and diastolic.
Systolic refers to systole, the phase when the
heart pumps blood out into the aorta.
Diastolic refers to diastole, the resting period when
the heart refills with blood.
At each heartbeat, blood pressure is raised to the
systolic level, and, between beats, it drops to the
diastolic level.
Hypertension is defined as systolic blood
pressure (SBP) of 140 mmHg or greater,
diastolic blood pressure (DBP) of
90 mmHg or greater, or taking
antihypertensive medication.
VI JNC, 1997
Types of hypertension
Essential hypertension
90%
No underlying cause
Secondary hypertension
Underlying cause
Causes of Secondary Hypertension
Renal Congenital anomalies, pyelonephritis, renal
artery obstruction, acute and chronic
glomerulonephritis Reduced blood flow to kidney
causes release of renin. Renin reacts with serum
protein in liver Coarctation of aorta
EndocrinePheochromocytoma Adrenal cortex
tumors Cushing’s syndrome Hyperthyroidism
Medications such as estrogens, sympathomimetics,
antidepressants, NSAIDs, steroids, Amphetamines
Neurogenic
Miscellaneous
Identifiable Causes of Hypertension
1.
2.
3.
4.
5.
6.
7.
Sleep apnea Drug-induced
Chronic kidney disease
Primary aldosteronism Renovascular disease
Chronic steroid therapy and Cushing’s syndrome
Pheochromocytoma
Coarctation of the aorta
Thyroid or parathyroid disease
Hypertension: Predisposing factors
Age > 60 years
Sex (men and
postmenopausal women)
Family history of
cardiovascular disease
Smoking
High cholesterol diet
High intake of alcohol
Sedentary life style
Too much salt in the diet
Stress
Chronic kidney disease
Co-existing disorders
such as diabetes, obesity
and hyperlipidaemia
Adrenal and thyroid
disorders
Causes Hypertension
The exact causes of hypertension are not
known. Several factors and conditions may
play a role in its development, including:
The old renin-angiotensin-aldosterone system...
1999 WHO-ISH Guidelines :
Definitions and Classifications of BP Levels
Category*
Optimal
Normal
High-normal
Grade 1 hypertension (mild)
Borderline subgroup
Grade 2 hypertension (moderate)
Grade 3 hypertension (severe)
ISH
Borderline subgroup
SBP
(mm Hg)
< 120
< 130
130-139
140-159
140-149
160-179
> 180
> 140
140-149
DBP
(mm Hg)
< 80
< 85
85-89
90-99
90-94
100-109
> 110
< 90
< 90
WHO-ISH Guidelines Subcommittee J Hypertens 1999; 17:151
JNC-VI, 1997
Optimal:
<120 / and <80
Normal: <130 / and <85
High-Normal: 130-139 / or 85-89
Stage I: 140-159 / or 90-99
Stage II: 160-179 / or 100-109
Stage III: ≥180 / or ≥110
Definitions thankfully simplified
JNC-VII, 2003
NORMAL: <120/ and <80
Pre-Hypertension: 120-139/ or 80-89
Stage I: 140-159 / or 90-99
Stage II: >160 / or ≥100-109
1999 WHO-ISH Guidelines:
Stratification of risk to Quantify Prognosis
Degree of hypertension (mm Hg)
Risk factors and
disease history
I
No other risk
factors
II 1-2 risk factors
III > 3 risk factors or
target organ disease
or diabetes
IV Associated
Clinical conditions
Grade 1-mild
(SBP 140-159
or DBP 90-99)
Low risk
Grade 2-moderate
(SBP 160-179
or DBP 100-109)
Med risk
Grade3-severe
(SBP > 180
or DBP > 110)
High risk
Med risk
High risk
Med risk
high risk
Very high risk
Very high risk
Very high risk
Very high risk
Very high risk
WHO-ISH Guidelines Subcommittee J Hypertens 1999;17:151
CLINICAL MANIFESTATIONS
There are usually no symptoms or signs of
hypertension.
In fact, nearly one-third of those who have it don't
know it.
The only way to know if you have hypertension
definitely is to have your blood pressure checked
May cause headache, dizziness, blurred vision
when greatly elevated BP readings more than
140/90 mm of Hg
DIAGNOSTIC EVALUATION
ECG
Chest X-ray
Proteinuria,
elevated serum blood urea nitrogen (BUN), and creatinine
levels Serum potassium Urine (24-hour) for
catecholamines
Renal scan Renal duplex imaging
Outpatient ambulatory BP measurements
Diseases Attributable to Hypertension
Gangrene of the
Lower Extremities
Heart
Failure
Left Ventricular
Hypertrophy Myocardial
Infarction
Hypertensive
Encephalopathy
Aortic
Aneurym
HYPERTENSION
Coronary Heart
Disease
Blindness
Chronic
Kidney
Failure
Stroke
Cerebral
Preeclampsia/ Hemorrhage
Eclampsia
Adapted from Dustan HP et al. Arch Intern Med. 1996; 156: 1926-1935
Health Problems Are Associated With Hypertension
1. Atherosclerosis: Blood vessel damage occurs through
arteriosclerosis in which smooth muscle cell
proliferation, lipid infiltration, and calcium accumulation
occur in the vascular epithelium Damage to heart,
brain, eyes, and kidneys is termed target organ
disease
2. Heart Disease: heart failure (the heart can't adequately
pump blood),
3. ischemic heart disease (the heart tissue doesn't get
enough blood),
4. and hypertensive hypertrophic cardiomyopathy
(enlarged heart) are all associated with high blood
pressure.
1. Kidney Disease: Hypertension can damage the
blood vessels and filters in the kidneys, so that the
kidneys cannot excrete waste properly
2. Stroke: Hypertension can lead to stroke, either by
contributing to the process of atherosclerosis
(which can lead to blockages and/or clots), or by
weakening the blood vessel wall and causing it to
rupture.
3. Eye Disease: Hypertension can damage the very
small blood vessels in the retina.
1999 WHO-ISH Guidelines: Desirable BP Treatment Goals
Optimal or normal BP (< 130/85 mm Hg) for
Young patients
Middle-age patients
Diabetic patients
High-normal BP (< 140/90 mm Hg) desirable for
elderly patients
Aggressive BP lowering may be necessary in patients
with nephropathy, chronic renal failure, particularly if
proteinuria is
< 1 g/d - 130/80 mm Hg
> 1 g/d - 125/75 mm Hg
Significant benefits from intensive BP reduction
in diabetic patients
Major CV events / 100 patient-yr
30
25
24.4
18.6
20
15
11.9
10
5
0
< 90 mm Hg
< 85 mm Hg
< 80 mm Hg (target
DBP)
Lancet 1998, 351, 1755
Relative risks of specific types of clinical complications
related to tight and less tight BP Control
Clinical end point
Any diabetes-related
end point
Deaths related to
diabetes
All cause mortality
Myocardial infarction
Stroke
Peripheral vascular
disease
Microvascular disease
Patients with
aggregate
and points
Tight
Less tight
control
control
(n=758)
(n=390)
259
170
Absolute risk
(events/1000
patients-yr)
Less
Tight
tight
control
control
50.9
67.4
p
0.0046
RR for
tight control
(95% Cl)
0.76 (0.62-0.92)
82
62
13.7
20.3
0.019
0.68 (0.49-0.94)
134
107
38
8
83
69
34
8
22.4
18.6
6.5
1.4
27.2
23.5
11.6
2.7
0.17
0.13
0.013
0.17
0.82 (0.63-1.08)
0.79 (0.59-1.07)
0.56 (0.35-0.89)
0.51 (0.19-1.37)
68
54
12.0
19.2
0.0092
063 (0.44-0.89)
Ref : UK Prospective Diabetes Study Group BMJ 1998; 317:703
Life style modifications
Lose weight, if overweight
Limit alcohol intake
Increase physical activity
Reduce salt intake
Stop smoking
Limit intake of foods rich in fats and cholesterol
Discourage excessive consumption of coffee and
other caffeine-rich products.
Diet
A healthy diet, such as the DASH (Dietary
Approaches to Stop Hypertension) diet, is very
effective at lowering high blood pressure. The
DASH diet calls for a certain number of daily
servings from various food groups, including fruits,
vegetables, and whole grains. The following steps
can also help: Eating more fruits, vegetables, and
low-fat dairy foods
Eating less of foods that are high in saturated fat
and cholesterol, such as fried foods Eating more
whole grain products, fish, poultry, and nuts Eating
less red meat and sweets Eating foods that are
high in magnesium, potassium, and calcium
Factors affecting choice of antihypertensive drug
The cardiovascular risk profile of the patient
Coexisting disorders
Target organ damage
Interactions with other drugs used for
concomitant conditions
Tolerability of the drug
Cost of the drug
Drug therapy for hypertension
Class of drug
Example
Initiating dose
Usual
maintenance dose
Hydrochlorothiazide
12.5 mg o.d.
12.5-25 mg o.d.
Atenolol
25-50 mg o.d.
50-100 mg o.d.
Calcium
channel
blockers
Amlodipine
2.5-5 mg o.d.
5-10 mg o.d.
-blockers
Doxazosin
1 mg o.d.
1-8 mg o.d.
ACE- inhibitors
Lisinopril
2.5-5 mg o.d.
5-20 mg o.d.
Angiotensin-II
receptor blockers
Losartan
25-50 mg o.d.
50-100 mg o.d.
Diuretics
-blockers
Diuretics
Example: Hydrochlorothiazide
Act by decreasing blood volume and cardiac output
Decrease peripheral resistance during chronic therapy
Drugs of choice in elderly hypertensives
Drawbacks
Hypokalaemia
Hyponatraemia
Hyperlipidaemia
Hyperuricaemia (hence contraindicated in gout)
Hyperglycaemia (hence not safe in diabetes)
Not safe in renal and hepatic insufficiency
Beta blockers
Example: Atenolol
Block 1 receptors on the heart
Block 2 receptors on kidney and inhibit release of renin
Decrease rate and force of contraction and thus reduce
cardiac output
Drugs of choice in patients with co-existent coronary
heart disease
Drawbacks
Adverse effects: lethargy, impotency, bradycardia
Not safe in patients with co-existing asthma and
diabetes
Have an adverse effect on the lipid profile
Calcium channel blockers
Example: Amlodipine
Block entry of calcium through calcium channels
Cause vasodilation and reduce peripheral
resistance
Drugs of choice in elderly hypertensives and
those with co-existing asthma
Neutral effect on glucose and lipid levels
Drawbacks
Adverse effects: Flushing, headache, Pedal
edema
ACE inhibitors
Example: Lisinopril, Enalapril
Inhibit ACE and formation of angiotensin
II and block its effects
Drugs of choice in co-existent diabetes
mellitus
Drawbacks
Adverse effect: dry cough, hypotension,
angioedema
Angiotensin II receptor blockers
Example: Losartan
Block the angiotensin II receptor
and inhibit effects of angiotensin II
Drugs of choice in patients with
co-existing diabetes mellitus
Drawbacks
Adverse effect: dry cough,
hypotension, angioedema
Alpha blockers
Example: Doxazosin
Block -1 receptors and cause vasodilation
Reduce peripheral resistance and venous
return
Exert beneficial effects on lipids and insulin
sensitivity
Drugs of choice in patients with co-existing
hyperlipidaemia, diabetes mellitus and BPH
Drawbacks
Adverse effects: Postural hypotension
Antihypertensive therapy:
Side-effects and Contraindications
Class of drugs
Main side-effects
Contraindications/
Special Precautions
Diuretics
Electrolyte imbalance,
(e.g. Hydrochloro- total and LDL cholesterol
thiazide)
levels, HDL cholesterol
levels, glucose levels,
uric acid levels
Hypersensitivity, Anuria
-blockers
(e.g. Atenolol)
Hypersensitivity,
Bradycardia, Conduction
disturbances, Diabetes,
Asthma, Severe cardiac
failure
Impotence, Bradycardia,
Fatigue
Antihypertensive therapy: Side-effects and Contraindications (Contd.)
Class of drug
Main side-effects
Contraindications/ Special
Precautions
Calcium channel blockers
(e.g. Amlodipine,
Diltiazem)
Pedal edema, Headache
Non-dihydropyridine
CCBs (e.g diltiazem)–
Hypersensitivity,
Bradycardia, Conduction
disturbances, Congestive heart
failure, Left ventricular
dysfunction.
Dihydropyridine CCBs–
Hypersensitivity
-blockers
(e.g. Doxazosin)
Postural hypotension
Hypersensitivity
ACE-inhibitors
(e.g. Lisinopril)
Cough, Hypertension,
Angioneurotic edema
Hypersensitivity, Pregnancy,
Bilateral renal artery stenosis
Angiotensin-II receptor
blockers (e.g. Losartan)
Headache, Dizziness
Hypersensitivity, Pregnancy,
Bilateral renal artery stenosis
Choosing the right antihypertensive
Condition
Preferred drugs
Other drugs
that can be used
Drugs to be
avoided
Asthma
Calcium channel
blockers
-blockers
Diabetes
mellitus
-blockers/ACE
inhibitors/
Angiotensin-II
receptor blockers
-blockers
-blockers/Angiotensin-II
receptor blockers/Diuretics/
ACE-inhibitors
Calcium channel blockers
ACE inhibitors/ Angiotensin-II
receptor blockers/ Calcium
channel blockers
-blockers/ACEinhibitors/Angiotensin-II
receptor blockers/- blockers
-blockers/
Diuretics
High cholesterol
levels
Elderly patients
(above 60 years)
Calcium channel
blockers/Diuretics
BPH
-blockers
-blockers/ ACE inhibitors/
Angiotensin-II receptor
blockers/ Diuretics/
Calcium channel blockers
Diuretics/
-blockers
Limitations on use of antihypertensives in patients
with coexisting disorders
-blocker
Coexisting
Disorder
Diuretic
Diabetes
Caution/x Caution/x
ACE
All
inhibitor antagonist
CCB
1-blocker
Dyslipidaemia
x
x
CHD
Heart failure
3/Caution
Caution
Asthma/COPD
x
/Caution
Peripheral
vascular
disease
Caution
Caution
Caution
Renal artery
stenosis
x
x
Effect of various antihypertensives on coexisting disorders
Total
LDLHDLSerum
Glucose
Insulin
cholesterol cholesterol cholesterol triglycerides tolerance sensitivity
Diuretic
-
-
-
-
-blockers
-
ACE
inhibitors
-
-
-
-
All
antagonists
-
-
-
-
CCBs
-
-
-
-
-blockers
Combination therapy for hypertension – Recommended by JNC-VI
guidelines and 1999 WHO-ISH guidelines
With any single drug, not more than 25–50% of hypertensives achieve
adequate blood pressure control
J Hum. Hypertens 1995; 9:S33–S36
For patients not responding adequately
to low doses of monotherapy
Increase the dose of drug.
This, however, may lead to
increased side effects
Substitute with another drug
from a different class
Add a second drug from a
different class
(Combination therapy)
If inadequate response
obtained
Add second drug from different class
(Combination therapy)
Advantages of fixed-dose
combination therapy
Better blood pressure control
Lesser incidence of individual
drug’s side-effects
Neutralisation of side-effects
Increased patient compliance
Lesser cost of therapy
Fixed-dose combinations as recommended by
JNC-VI (1997) guidelines and 1999 WHO-ISH guidelines
Calcium channel blocker and -blocker
(e.g. Amlodipine and Atenolol)
Calcium channel blocker and ACE-inhibitor
(e.g. Amlodipine and Lisinopril)
ACE-inhibitor and Diuretic (e.g. Lisinopril and
Hydrochlorothiazide)
-blocker and Diuretic (e.g. Atenolol and
Hydrochlorothiazide)
Efficacy and Tolerability of a fixed-dose combination of amlodipine and
atenolol (Amlopres-AT) in Indian Hypertensives (n=369)
90
200
80
150
100
175.4+
19.4
143.8
+ 13.2
106.8
+ 10.5
50
88.2
+ 7.6
0
% responders
Blood Pressure (mm Hg)
Reduces BP effectively
80.5%
70
60
50
40
30
20
Systolic
Basal
Diastolic
Week 4
10
0
Safe and well tolerated
Adverse events were reported in 7.9% of patients
Common side effects included edema, fatigue and headache
Indian Practitioner 1997; 50: 683-688.
Efficacy and Tolerability of combined amlodipine and
lisinopril (Amlopres-L) in Indian hypertensives (n=330)
90
200
150
100
80
175.4+
19.4
143.8
+ 13.2
106.8
+ 10.5
50
88.2
+ 7.6
0
% responders
Blood Pressure (mm Hg)
Reduces BP effectively
77.65
70
60
50
40
30
20
Systolic
Basal
Diastolic
Week 4
10
0
Safe and well tolerated
Adverse events were reported in 9.7% of patients
Side effects commonly reported included cough and edema
Only 1.76% of patients withdrew from the study.
Indian Practitioner 1998; 51: 441-447.
Drugs in special conditions
Condition
Preferred Drugs
Pregnancy
Nifedipine, labetalol,
hydralazine, beta-blockers,
methyldopa, prazosin
Coronary heart disease
Beta-blockers, ACE
inhibitors, Calcium channel
blockers
Congestive heart
failure
ACE inhibitors,
beta-blockers
1999 WHO-ISH guidelines
BEST MANAGEMENT OF HYPERTENSION
To use the fewest drugs at the lowest doses while
encouraging the patient to maintain lifestyle
changes.
After BP has been under control for at least 1
year, a slow, progressive decline in drug therapy
can be attempted.
However, most patients need to resume
medication within 1 year.
Summary
Hypertension is a major cause of morbidity
and mortality, and needs to be treated
It is an extremely common condition;
however it is still underdiagnosed and
undertreated
Hypertension is not controlled with
monotherapy in at least 50% of patients; in
these patients combination therapy is
required
ISOLATED SYSTOLIC HYPERTENSION
Systolic BP elevation in the absence of
elevated diastolic BP is termed isolated
systolic hypertension
Definitions
Hypertensive Crisis
Urgency or Emergency
Hypertensive Urgency
“Severe elevation of blood pressure”
Generally DBP >115-130
No progressive end organ damage
Hypertensive Emergency
“Severe elevation of blood pressure”
Generally occurs with DBP >130
WITH significant or progressive end organ damage
•
•
•
•
•
•
•
Hypertensive Encephalopathy
CVA – Ischemic versus hemorrhagic
Acute Aortic Dissection
Acute LVF with Pulmonary Edema
Acute MI / Unstable Angina
Acute Renal Failure
Eclampsia
Urgency vs. Emergency
Urgency
No need to acutely lower blood pressure
May be harmful to rapidly lower blood pressure
Death not imminent
Emergency
Immediate control of BP essential
Irreversible end organ damage or death within
hours