12. Pulmonary mycosis, work related pulmonary diseases
advertisement

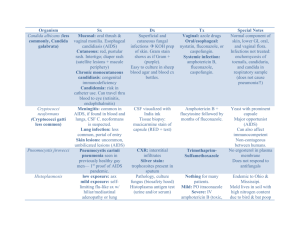
Fungal lung diseases Occupational lung diseases Edit Csada, MD 19.11.2014. PATHOGEN FUNGI Facultative pathogens Saprophyte Aspergillus fumigatus Aspergillus flavus Cryptococcus neoformans Mucoraceae Parasite Candida albicans Candida tropicalis Obligate pathogens Histoplasma capsulatum Coccidioides immitis Blastomyces dermatitidis Sporothrix shenckii RISK FACTORS Immuncompromised state, treatment Cytostatic treatment Antibiotic and steroid treatment Leukemy Neutropenic patients Malignancies Diabetes mellitus AIDS After intensive therapy After transplantation PATHOLOGICAL FINDINGS Epitheloid hyperplasia Histocyte granulomas Thrombotic arteriitis Caseation granuloma Fibrosis Calcification DIAGNOSTIC METHODS Microscopic examination native smear different stainings Culture Special culture media Histology + culture Skin test Serology Differential diagnosis tumor tuberculosis chr pneumonia THERAPY Medical treatment Polyens Amphotericin B (Fungisone) Nystatin Pimafucin 5 fluorocytosin Ancotil Azoles Ketoconazole (Nizoral) Clotrimazole (Canesten) Caspofungin (cancidas) Fluconazole (Diflucan) Itraconazole (Orungal) Voriconazole (Vfend) (2. gen.) Surgery CLINICAL MANIFESTATION OF ASPERGILLOSIS Allergic aspergillosis Extrinsic allergic alveolitis hypersensitivity pneumonitis Allergic bronchopulmonary aspergillosis Aspergillomas Invasive aspergillosis Rare manifestations Aspergillus endocarditis Aspergillus pneumonia Endophthalmitis ALLERGIC BRONCHOPULMONARY ASPERGILLOSIS Type I immediate hypersensitivity reaction Type III antigen, antibody, immune komplex reaction Diagnosis Bronchial obstruction Fever Eosinophylia Skin test IgG se precipitating antibody Total, specific IgE X-ray Small, fleeting inflitrates Hilar, paratracheal adenopathy Chronic consolidation Alveolitis – fibrosis Bronchiectasis Therapy Chromoglycate Corticosteroid ASPERGILLOMA Saprophytic colonisation of fungi in pulmonary cavities Manifestation No symptoms Haemoptysis Fever Cachexia Chraracteristic x-ray picture! Therapy: surgery INVASIVE ASPERGILLOSIS Immuncompromised host! Necrotising pneumonia Empyema Pulm., extrapulm. Dissemination Symptoms: fever, pleural pain, haemotysis Therapy: Amphotericin B or voriconazole itraconazole, caspofungin CANDIDIASIS Normal inhabitants of mucocutaneous body surfaces. 80% of all systemic fungal infection Manifestation Disease of skin and mucosa Gynecological disease Oesophagitis In the lung: Bronchitis Pneumonia Pleurisy Therapy: Amphotericin B, caspofungin, fluconazole, itraconazole, voriconazole CRYPTOCOCCOSIS It is the 4. Most common cause of opportunistic infections in AIDS patients in the US. Manifestations: asymptomatic colonisation ext. All. Alveolitis primary complex toruloma Diagnosis: Masson-Fontana staining Complication: meningoencephalitis Therapy: spontaneous healing, amphotericin B, fluconazole, flucytosine HISTOPLASMOSIS It is the most common systemic mycosis in the USA. Manifestation Subclinical Acute form: Influenzalike disease X-ray: small scattered, patchy infiltrates calcification Progressive, disseminated form Rare (AIDS) Chr. pulmonary form (COPD) Segmental, interstitial pneumonitis Chr cavitary disease Diagnosis: Wright’s or Giemsa staining Prognosis: good Therapy: itraconazole, amphotericin B COCCIDIOIDOMYCOSIS Acute, benign disease Primary infection: infuenzalike symptoms Radiological findings: Segmental pneumonia Minimal infiltrates Adenopathy, pleural effusion Nodular lesions, cavities Prognosis is good without any therapy. Diagnosis: eosinophilia, IgG Progressive, extrapum. manifestation COCCIDIOIDOMYCOSIS • Risk factors for dissemination of Coccidioides Immitis infection • Older age • Males • Non-caucasians, Filipinos • Immunsuppression • Gravidity • Therapy • Azoles • Fluconazole > Itraconazole • Ketoconazole: less effective 20 Occupational lung diseases Pneumoconiosis Hypersensitivity pneumonitis Obstructive airway diseases Toxic damages Malignant lung diseases Pleural diseases 21 Common causes of occupational asthma Agents Occupational exposure Isocyanates Spray paints, varnishes, adhesives, polyurethane foam manufacture Flour Bakers Epoxy resins Hardening agents, adhesives Animals (rats, mice) Laboratory workers Wood dusts Sawmill workers, joiners Azodicarbonamide Polyvinyl plastics manufacture Persulphate salts Hairdressers Latex Healthcare workers Drugs Pharmaceutical industry Grain dust Farmers, millers, bakers Occupational asthma • Diagnosis: – Asthma diagnosis – Causative connection between asthma and working place • Clinical manifestations – Immediate asthmatic response – Delayed asthmatic response – Combined response • Therapy: – Avoidance of exposition – Protective devices – Asthma treatment 23 PNEUMOCONIOSIS Etiologic agents: dusts inhalation of inorganic metal dusts free silica coal dusts 24 SILICOSIS The base of disease is the progressive concentric fibrosis with hyalinisation in the centre. Free silica: mining stone cutting road and building construction blasting 25 DETERMINING FACTORS IN DEVELOPMENT OF SILICOSIS Silicic acid content Content of dusts in the place of work (200 000/m3) Size of dust (<2 micron) Time of exposure Individual inclination (smoking) 26 SILICOSIS Symptoms: no symptoms dyspnoe hypoxaemia, hypercapnia=> ventilatory failure=> cor pulmonale X-ray: nodular dissemination silicomas (=>emphysematic bullae) hilar adenopathy calcification, egg shell pattern Complications:chr. bronchitis emphysema ptx Tb is more frequent Caplan’s syndroma Therapy: symptomatic Prophylaxis! 27 28 29 30 Silicosis 31 32 ASBESTOSIS • Hydrosilicate – fibre, thread • Pulmonal clearence depends on the ratio of length and diameter of fibers • 50-100 asbest particula/cm3 → mesothelioma • Basal and subpleural fibrosis 33 34 HYPERSENSITIVE PNEUMONITIS (Extrinic allergic alveolitis) It is an immunologically induced inflammation of lung parenchyma involving alveolar walls and terminal airways secondary to repeated inhalation of a variety of organic dusts and other agents by susceptible host. Manifestations: Farmer’s lung (1932) – thermophylic actinomycetes Bird fancier’s breeder’s or handler’s lung Miller’s lung Bagassosis Byssinosis Air conditioner’s lung Coffee worker’s lung 35 HYPERSENSITIVE PNEUMONITIS Clinical forms: Acute: (type III. reaction) cough, fever, chills, malaise, dyspnoe may occur 6-8 hours after exposure and usually clear within few days Subacute: (type IV reaction) symptoms appear over a period of week( cough, dyspnoe, cyanosis). Symptoms disappear within weeks, or months, if causative agent is no longer inhaled. Chronic: (type IV reaction) gradually progressive intersistial disease associated with cough, exertional dyspnoe without a prior history of acute or subacute disease. 36 37 38 HYPERSENSITIVE PNEUMONITIS Diagnosis: anamnesis x-ray: normal poorly defined patchy or diffuse infiltrates reticulonodular lesions lung function tests:impaired diffusing capacity, decreased comliance exercise induced hypoxaemia Se precipitins against suspected antigens BAL: acute : neutrophyls, monocytes(5%) chr: lymphocytes(60-70%) Lung biopsy: intersitial alveolar infiltrates bronchiolitis Therapy: avoidance of antigens 39 corticosteroids Thank you for your attention! 40